Percutaneous nephrolithotomy in octogenarians and beyond: How old is too old?
Bradley Morganstern*,Riccardo Galli,Piruz Motamedinia, David Leavitt,Mohamed Keheila,Eric Ghiraldi,David Hoenig, Arthur Smith,Zeph Okeke
The Smith Institute for Urology,NorthShore-Long Island Jewish Health System,New Hyde Park,NY,USA
ORIGINAL ARTICLE
Percutaneous nephrolithotomy in octogenarians and beyond: How old is too old?
Bradley Morganstern*,Riccardo Galli,Piruz Motamedinia, David Leavitt,Mohamed Keheila,Eric Ghiraldi,David Hoenig, Arthur Smith,Zeph Okeke
The Smith Institute for Urology,NorthShore-Long Island Jewish Health System,New Hyde Park,NY,USA
Percutaneous
nephrolithotomy;
Elderly;
Percutaneous stone extraction
complications;
Clavien;
Octogenarians;
Percutaneous stone extraction
Objective:To specifically report perioperative characteristics and outcomes in patients 80 years and older undergoing percutaneous nephrolithotomy(PCNL).PCNL has been established as feasible in the elderly;however,to our knowledge no one has specifically reported feasibility in patients 80 years and older.
Methods:We retrospectively reviewed perioperative data of octogenarians who underwent PCNL at a high stone volume single institution,and matched them to patients<65 years of age by stone burden and sex.Patient demographics,perioperative outcomes and postoperative complications were compared.
Results:Thirty-three octogenarians(mean age 83.6 years)with 36 renal units were matched to 67 controls(mean age 48.6 years)with 72 renal units.Octogenarians had a higher mean American Society of Anesthesiologists(ASA)score,more comorbidities,and worse renal function. There were no differences in operative characteristics,length of hospital stay or stone free rates.Of the patients with preoperative urinary decompression(ureteral stent or nephrostomy tube)prior to PCNL,the elderly were more likely to have a history of urosepsis.Octogenarians did not experience more minor Clavien(I-II)or major Clavien(IIIa-IVb)complications.
Conclusion:Octogenarians who undergo PCNL were more likely to have cardiovascular comorbidities and a prior history of sepsis.Despite these risk factors,in appropriately selected patients PCNL can be safely and successfully performed in octogenarians without increased perioperative complications relative to a younger cohort.
?2015 Editorial Office of Asian Journal of Urology.Production and hosting by Elsevier (Singapore)Pte Ltd.This is an open access article under the CC BY-NC-ND license(http:// creativecommons.org/licenses/by-nc-nd/4.0/).
1.Introduction
Though age itself is not considered an illness,decreased functional reserve and associated comorbid conditions[1] that manifests with increasing age results in excess surgical risk in elderly patients and plays a critical role in perioperative outcomes,thereby influencing the surgeon’s decision to proceed[2].However,as we learn more about the physiology of aging surgeons are reducing their thresholds for invasive,high-risk surgery[2].An example is the increasing rate of cystectomies performed for elderly patients,with contemporary results from high volume centers showing no significant increase in complications or mortality for octogenarians[3,4].The incidence of nephrolithiasis in octagenarians is growing as well[5]and because of the high risk of urinary tract infection and renal dysfunction with untreated large kidney stones,the conservative approach,even in elderly patients,may not always be wise[6,7].Percutaneous nephrolithotomy(PCNL) has been shown to be an effective and safe procedure in patients of all ages but the data pertaining to elderly mostly include patients around the age of 70 years[8-10]. Unfortunately,little if any data exist for complex stone treatments in the small but expanding segment of the stone bearing patients 80 years and older.To this end,we present our experience with PCNL in octogenarian patients,and compare their outcomes with a younger matched cohort.To our knowledge this is the first report to specifically address and include octogenarians.
2.Patients and methods
We retrospectively reviewed our nephrolithotomy database and identified 33 patients(36 PCNLs)80 years and older (80-97 years)who underwent PCNL between July 2011 and May 2014.Using a one-to-two case controlled study design, 72 procedures were identified in 67 younger patients (21-64 years),who had undergone PCNL during the same period.The sample was balanced according to mean stone area(measured in at least two dimensions),number of staghorn stones,and gender.
All PCNL procedures were performed by one of three experience dendourologists(DH,ZO,or AS).With patients in the prone position,renal calyceal punctures were accomplished under fluoroscopic guidance using an 18G diamond-tipped needle.The percutaneous access tract was dilated up to 30 Fr with sequential Amplatz renal fascial dilators or a balloon dilator at the surgeon’s discretion. Stones were grasped and extracted or fragmented using an ultrasonic probe with suction(Olympus CyberWand?Dual Ultrasonic Lithotriptor,Center Valley,PA,USA).
Initial intra-operative stone clearance was determined with flexible nephroscopy,antegrade nephrostography,andfluoroscopy at the end of the procedure.For patients withfluoroscopically visible fragments that could not be identi fied under direct vision,a noncontrast CT scan was performed on the first postoperative day and if significant residual fragments existed,a second stage procedure was performed.The final stone-free status was assessed for all patients at the 3-month follow-up visit with renal ultrasonography or CT scan based on the imaging available at the time of analysis.We defined stone clearance as those patients with no residual fragments.Operative time was calculated between anesthetic induction and extubation.
Patient demographics,comorbidities,perioperative data and complications were compared between groups. Statistical analysis was performed using t-test for continuous variables with normal distribution,and Chi-square test for categorical covariates by Stata 11.0(Stata Corporation, College station,TX,USA).A p-value<0.05 was considered statistical significance.IRB approval was granted for the study.
3.Results
The mean age in the octogenarian cohort was 83.6 years (range 80-97 years).Gender and laterality of stones were comparable.Those in the elderly group were more likely to have cardiovascular comorbidities,a higher American Society of Anesthesiologists(ASA)score,worse renal function,and were more likely to be on anticoagulant and antiplatelet therapy.Aspirinwascontinued in five octogenarians and three younger patients(Table 1).
Octogenarians were more likely to have preoperative urine analyses which were nitrite positive(32%vs.15%, p=0.034),have positive(44%vs.28%)or contaminated (28%vs.15%,p=0.026)preoperative urine cultures,have received preoperative antibiotics(69%vs.31%,p<0.001), and have a history of urosepsis(47%vs.13%,p<0.001)prior to PCNL.In patients with a stent or nephrostomy tube placed prior to PCNL,the elderly were more likely to have a history of sepsis as well as preoperative antibiotics(Table 2). However,the two groups showed no significant difference in postoperative urinary tract infections(UTI)or sepsis within 30 days.
Stone area and percentage of staghorn stones were similar between groups,consistent with our methods for matching patients.Mean postoperative reduction in hemoglobin,transfusion rate(with the need for being based clinical variables such as light headedness,lethargy,hematuria as well as relative blood loss seen on routine laboratory values and operative losses)and length of stay were similar across both groups(Table 3).Stone free status was achieved with no statistical significant difference between groups.
Perioperative complications were assessed according to the modified Clavien-Dindo classification(Table 4)[11]. There was no difference between groups in the rates of overall(36%vs.46%,p=0.29),minor(Clavien I-II)or major(Clavien IIIa-IVb)complications.Minor complications were predominately fevers managed with antipyretics and antibiotics.Major complications included one bowel injury in the≥80-year-old group,and there was no signif icant difference in the number of sepsis episodes requiring intensive care(3 vs.6;Clavien IVa)or angioembolization(4 vs.5;Clavien IIIb)between groups.There were no mortalities(Clavien V).
4.Discussion
The feasibility of PCNL in the elderly has been reported, but to our knowledge this is the first report specifically examining PCNL in patients 80 years and older.It isimportant to note that the patients in our cohort were all symptomatic with chronic kidney disease(CKD),UTIs,pain, and/or prior stone procedures.The evidence presented here points to the safety and efficacy of treatment despite the attendant co-morbid medical conditions in this population.
Benson and colleagues[12]reported on 219 patients who underwent PCNL:none of those who had a nephrostomy tube placed prior to PNCL had episodes of systemic inflammatory response syndrome(SIRS)whereas 5.9%of the patients without nephrostomy drainage did.This apparently protective procedure may have played a role in our patients both elderly and young.In our study there was no significant difference between the elderly and the younger cohort in regards to having preoperative drainage with either a nephrostomy tube or stent(p=0.14).However, when comparing patients who had a stent or nephrostomy tube prior to PCNL,the elderly cohort were more likely to have a history of sepsis(47%vs.13%,p<0.001)as well as be on preoperative antibiotics(69%vs.31%,p<0.001). Here again we highlight a tendency for elderly patients to require multiple procedures/medications and more infections,and hence increased potential morbidity.Interestingly,the elderly in our cohort with upper urinary tract drainage present at the time of the PCNL were not more likely to have fevers,SIRS,sepsis or overall complications which may be due to the protective mechanism Benson et al.[12]observed.
When examining other methods of stone management for larger stones,Moreno et al.[13]noted increased age as an independent risk for bacteriuria after extracorporeal shock wave lithotripsy(ESWL).Polat and colleagues[14] found an 84.4%stone free rate after ESWL for stones>10 mm with an overall complication rate of 24.4%.The mean stone size was 12.65 mm and patients on average had 2.04 treatments.In our elderly cohort we found 78%stonefree rate with an overall complication rate of 35%after PNCL.The differences may reflect a larger and more complex stone burden in our patients(average stone size 345.8 mm2).Furthermore,the patients in the current study required fewer auxiliary procedures,with only three second stage procedures in the elderly(8%)and younger(4%) cohorts apiece.When exploring retrograde ureteroscopy as an option for large renal stones,Riley et al.[15]noted an average of 1.82 procedures required with an overall 90.9% stone free rate for stones larger than 3 cm;and Ricchiuti et al.[16]found that as size increases stone free rates decline from 87.5%in the 2-3 cm stone size down to 40%in the greater than 4 cm groups.In addition,they note that overall 43%of patients required a second procedure to achieve a stone free state.Thus,in our estimation,PCNL achieves acceptable stone free rates with comparable complications despite the larger stone burden and more invasive nature of the procedure,minimizing the need for secondary procedures and consistent with other studies examining PCNL in the elderly[7,8,10].
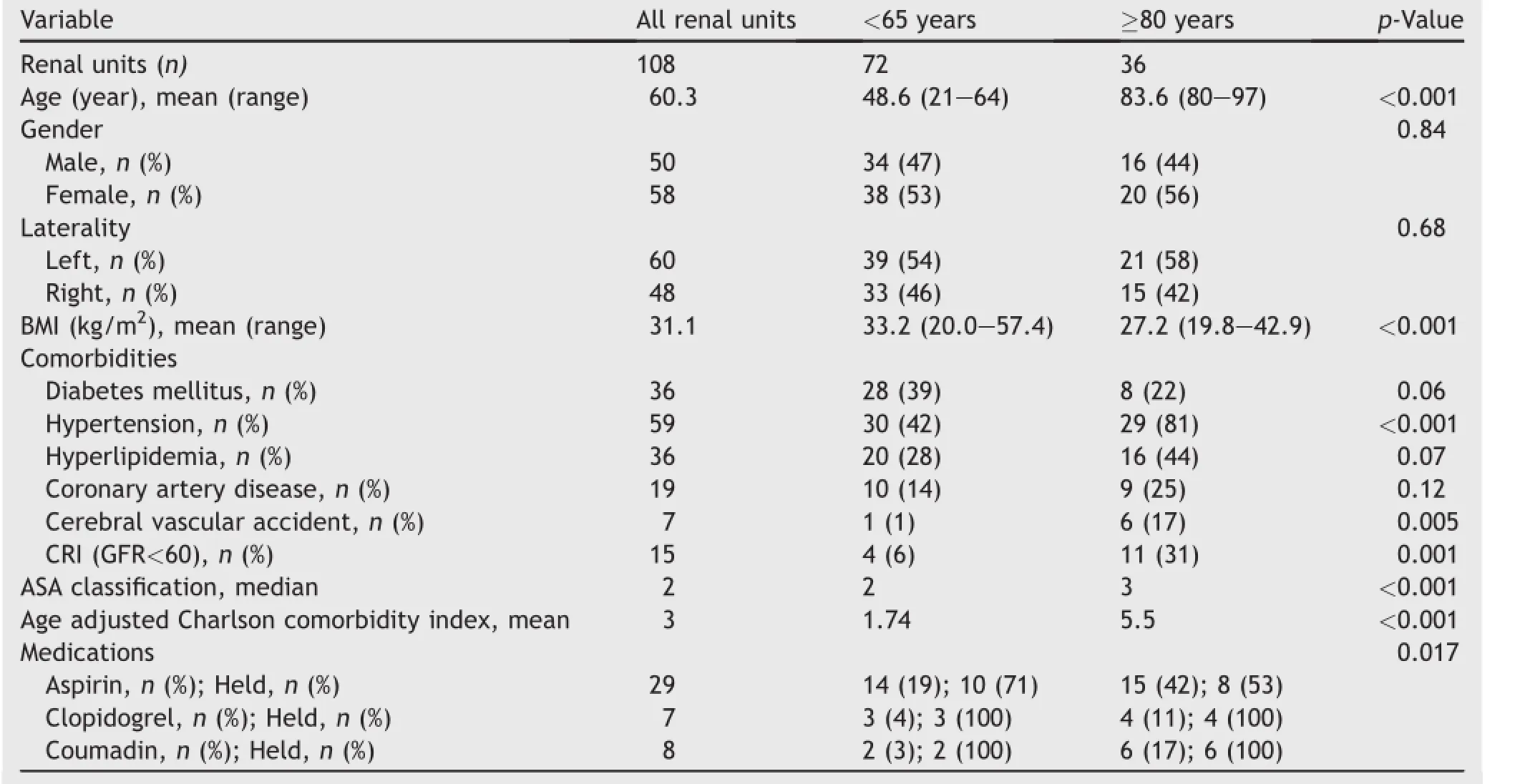
Table 1Patient demographics in the two study groups.
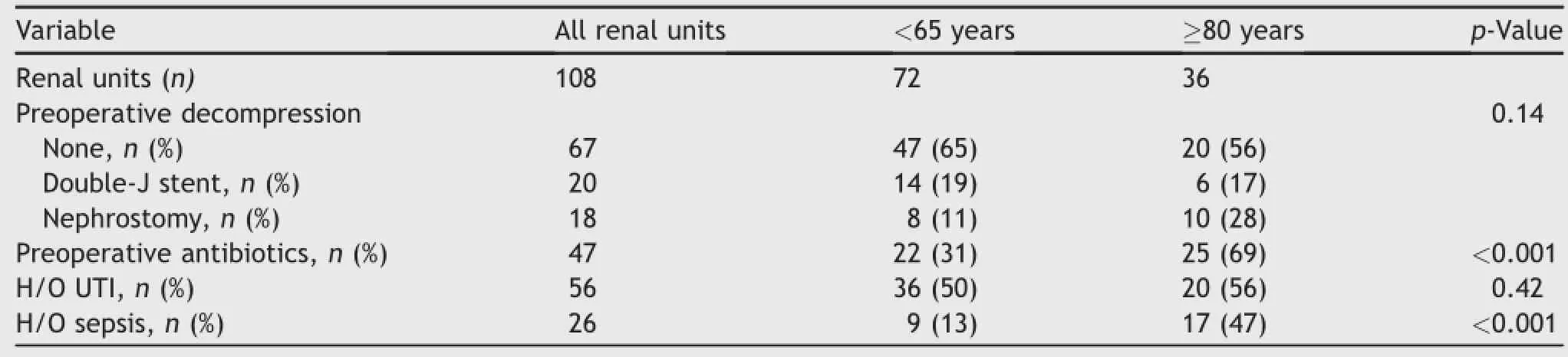
Table 2Preoperative data in the two study groups.
We do note the relatively high,though statistically similar rate of transfusions(14%and 15%,p=0.54)and angioembolizations(11%vs.3%,p=0.09)for the elderly and younger cohort,respectively.With regards to the high transfusion rate we believe this is acceptable percentage with the inherent risks of the procedure and the low rate of necessary second stage procedure.In fact contemporary papers have reported transfusion rates as high as 12%[17]. In addition,based on previously published literature by our institution examining vascular complications after renal parenchymal surgery,we opt for early diagnostic angiography rather computer tomography with contrast as angiography can be diagnostic and therapeutic when delayed bleed is suspected.This strategy does not appear to worsen renal function[18].Moreover,early angioemoblization rather than observation can reduce further transfusions and minimize duration of hospitalization[10].
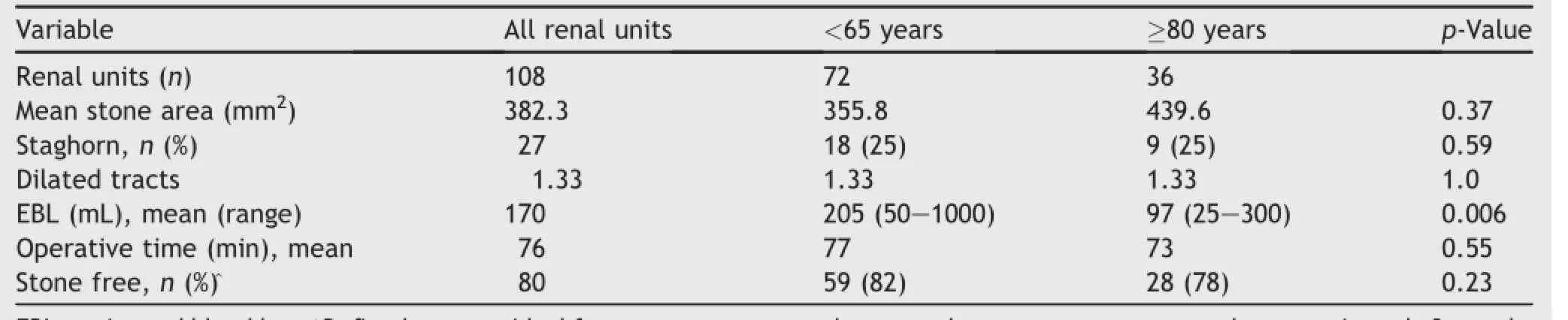
Table 3Stone and operative characteristics.
The elderly patients in our study had more comorbidities,worse ASA scores,and more UTIs requiring preoperative antibiotics;nevertheless,their outcomes were comparable to the younger cohort.The elderly endured the procedure without increased risk of bleeding as evidenced by similar decreases in hemoglobin,transfusion rates and angioembolization rates.Contrary to previous studies finding a slightly increased risk of complications and hospital stays,our patients over the age of 80 were not more likely to experience complications post-PCNL(36%vs.46%; p=0.29)and we saw only a slightly longer,though nonsignificant,trend toward increased length of stay[10]. The successful outcomes of these patients may in part be due to the medical community’s increasing comfort in managing and understanding the potential pitfalls inherent with high-risk procedures in elderly patients.A multidisciplinary preoperative evaluation is necessary and increasingly routine in these complex patients.
Regarding asymptomatic patients,it has been well documented that individuals,especially women,with a history of kidney stones have an increased risk of CKD(odds ratio 1.5)as well as a higher likelihood of requiring dialysis (odds ratio 2.37)[19].In patients with CKD(pre-PCNL GFR of 32.1 mL/min/1.73 m2)who undergo PCNL it has been shown that up to 86.8%will have stable or improved renalfunction 5 years following the procedure[20]suggesting an imperative to treat patients preventatively[21].In our population we noted a higher prevalence of CKD in the elderly population(≥80 year old)compared with those<65 years old(31%vs.6%,p<0.001),which is in stark contrast to the national overall prevalence of 14.0%[19].This difference may be due to a combination of factors for which nephrolithiasis likely contributesor may be a consequence of failure to treat asymptomatic stones aggressively earlier. This subject is beyond the scope of this paper and requires further study.
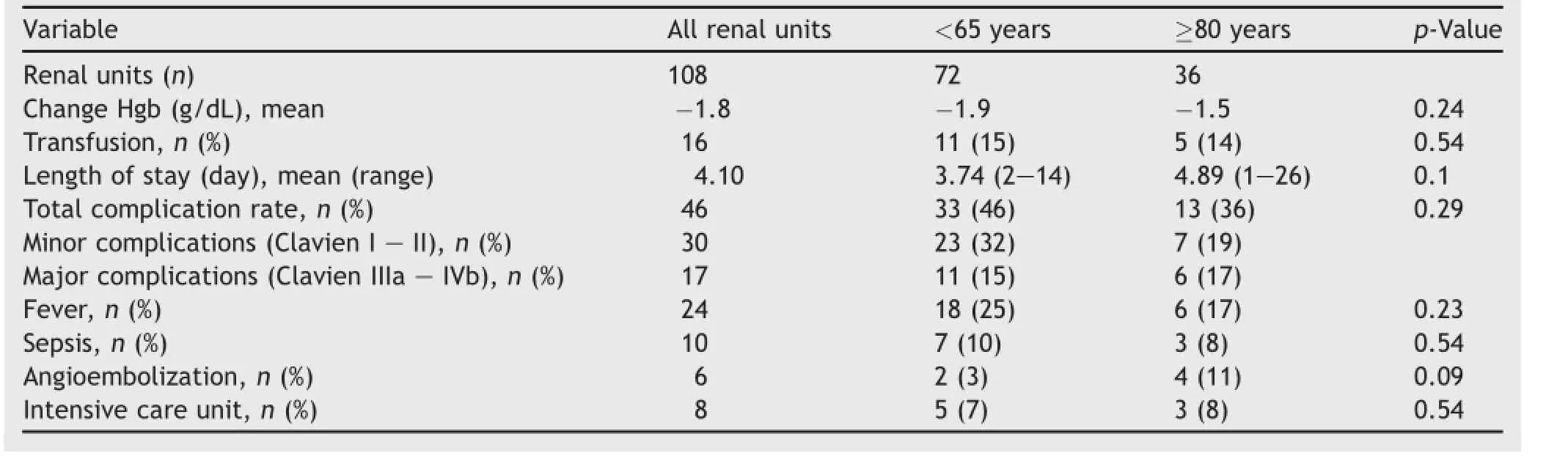
Table 4Postoperative outcomes and complications.
The risk of acute and recurrent urinary infections and their impact on long-term renal deterioration is of paramount importance when deciding between stone observation and intervention in the elderly.Krambeck et al.[22] reported as age increases,nephrolithiases in the elderly were more likely to present with fevers and UTIs rather than acute colic,and stones were less likely to pass spontaneously,thus increasing the need for intervention. Saucier et al.[23]found that stone formers with CKD had more frequent UTI’s than those without CKD(22.6%vs. 6.6%,p=0.004).Furthermore,the need for emergency urinary tract drainage approximately doubles for patients≥75 years[24].Consistent with previously reported findings,the elderly group in our study was more likely to have CKD,positive or contaminated preoperative urine cultures, and have received preoperative antibiotics.Taken together,these findings help highlight the importance of managing nephrolithiasis in the elderly in a timely controlled manner.
Through our experience with performing PCNL on the elderly we have noted eight key observations/suggestions when managing these patients:
1)Ensure patients have undergone necessary preoperative clearances and treatments to optimize reserves prior to the procedure.
2)Consider having a lower threshold to intervene earlier rather than observe stone growth overtime as evidence points increasing medical comorbidity as age increases.
3)At initial presentation of acute crisis with patients who meet reasonable criteria for percutaneous intervention (i.e.,large stone burden,narrow infundibulum,acute angle of lower pole,etc.)consider placing nephrostomy tube prior to stone manipulation(stenting may be an acceptable alternative).
4)If complications(i.e.,bleeding,sepsis)occur consider early intervention and closer observation.
5)If medically appropriate,percutaneous nephrolithotomy is preferred over shock wave lithotripsy,as it tends to have higher stone free rates with fewer secondary procedures.
6)Ensure adequate padding of pressure points during procedure.
7)Recommend family members are present evenings after the procedure to help with events such as sun downing.
8)Recommend early ambulation with assistance and early physical therapy consult.
There are several limitations to our study including the retrospective design.Prospective controlled studies with patients randomized to treatment versus observation,if deemed to be ethically advisable,would be needed to fully evaluate if surgery is necessary in these patients.However, the patients who were in these cohorts were symptomatic deeming intervention appropriate.Another limitation is the relatively small sample size.It is conceivable that with only 36 elderly renal units analyzed more subjects may reveal significant differences.Last,the fact that the study was carried out at high volume single institution limits its generalizability.
5.Conclusion
Percutaneous nephrolithotomy,in appropriately selected individuals,is safe and effective in patients over the age of 80 years despite the relative increase in comorbidities when compared to a matched cohort of younger patients. Treating the elderly with symptomatic stones may lead to less health care dollars spent and improved quality of life for those afflicted.As such,PCNL should not be denied to patients 80 years and older on the basis of age alone.
Conflicts of interest
The authors declare no conflict of interest.
[1]Smith R,Osterweil D,Ouslander JG.Perioperative care in the elderly urologic patient.Urol Clin North Am 1996;23:27-41.
[2]Tonner PH,Kampen J,Scholz J.Pathophysiological changes in the elderly.Best Pract Res Clin Anaesthesiol 2003;17:163-77.
[3]Donat S,Siegrist T,Cronin A,Savage C,Milowsky M,Herr H. Radical cystectomy in octogenarians-does morbidity outweigh the potential survival benefits?J Urol 2010;183:2171-7.
[4]Roghmanna F,Sukumarc S,Ravic P,Trinha V,Meskawia M, Ghanic K,et al.Radical cystectomy in the elderly:national trends and disparities in perioperative outcomes and quality of care.Urol Int 2014;92:27-34.
[5]Curhan GC.Epidemiology of stone disease.Urol Clin North Am 2007;34:287-93.
[6]Gupta M,Bolton DM,Gupta PN,Stoller ML.Urolithiasis in renal failure.J Urol 1994;152:1086-90.
[7]Stoller ML,Bolton D,Lezin M,Lawrence M.Percutaneous nephrolithotomy in the elderly.Urology 1994;44:651-4.
[8]Sahin A,Atsu¨N,Erdem E,Oner S,Bilen C,Bakkaloˇglu M,et al. Percutaneous nephrolithotomy in patients aged 60 years or older.J Endourol 2001;15:489-91.
[9]Streem SB.Stone extraction.In:Smith AD,Badlani GH, Bagley DH,et al,editors.Smith’s textbook of endourology.St. Louis:Quality Medical Publishing;1996.p.239-63.
[10]Okeke Z,Smith AD,Labate G,D’Addessi A,Venkatesh R, Assimos D,et al.CROES PCNL study group.Prospective comparison of outcomes of percutaneous nephrolithotomy in elderly patientsversus youngerpatients.J Endourol2012;26:996-1001.
[11]Dindo D,Demartines N,Clavien P.Classification of surgical complications:a newproposalwith evaluation in a cohortof6336 patients and results of a survey.Ann Surg 2004;240:205-13.
[12]Benson A,Juliano T,Miller N.Infectious outcomes of nephrostomy drainage before percutaneous nephrolithotomy compared to concurrent access.J Urol 2014;192:770-4.
[13]Moreno M,Lirola M,Tabar G,Baena G,Tenza T,Encinas L. Incidence of infectious complications after extracorporealshock wave lithotripsy in patients without associated risk factors.J Urol 2014;192:1446-9.
[14]Polat F,Yes S,Ak E,Farahvash A,Karaog U,Biri H,et al.Safety of ESWL in elderly:evaluation of independent predictors and comorbidity on stone-free rate and complications.Geriatr Gerontol Int 2012;12:413-7.
[15]Riley JM,Stearman L,Troxel S.Retrograde ureteroscopy for renal stones larger than 2.5 cm.J Endourol 2009;23:1395-8.
[16]Ricchiuti DJ,Smaldone MC,Jacobs BL,Smaldone AM, Jackman SV,Averch TD.Staged retrograde endoscopic lithotripsy as alternative to PCNL in select patients with large renal calculi.J Endourol 2007;21:1421-4.
[17]Resorlu B,Diri A,Atmaca A,Tuygun C,Oztuna D,Bozkurt O, et al.Can we avoid percutaneous nephrolithotomy in high-risk elderly patients using the charlson comorbidity index?Urology 2012;79:1042-7.
[18]Montage S,Rais-Bahrami S,Seideman C,Rastinehad A,Vira M, Kavoussi L,et al.Delayed haemorrhage after laparoscopic partial nephrectomy:frequency and angiographic findings.BJU Int 2011;107:1460-6.
[19]Shoag J,Halpern J,Goldfard D,Eisner B.Risk of chronic and end stage kidney disease in patients with nephrolithiasis.J Urol 2014;192:1440-5.
[20]Kurien A,Baishya R,Mishra S,Ganpule A,Muthu V,Sabnis R, et al.The impact of percutaneous nephrolithotomy in patients with chronic kidney disease.J Endourol 2009;23:1403-7.
[21]Fassett R.Current and emerging treatment options for the elderly patient with chronic kidney disease.Clin Interv Aging 2014;9:191-9.
[22]Krambeck A,Lieske J,Li X,Bergstralh E,Melton J,Rule A. Effect of age on the clinical presentation of incident symptomatic urolithiasis in the general population.J Urol 2013; 189:158-64.
[23]Saucier N,Sinha M,Liang K,Krambeck A,Weaver A, Bergstralh E,et al.Risk factors for CKD in persons with kidney stones:a case-control study in Olmsted County,Minnesota. Am J Kidney Dis 2009;55:61-8.
[24]Yoshimura K,Utsunomiya N,Ichioka K,Ueda N,Matsui Y, Terai A.Emergency drainage for urosepsis associated with upperurinary tract calculi.J Urol 2005;173:458-62.
Received 24 April 2015;received in revised form 14 August 2015;accepted 17 August 2015
Available online 4 September 2015
*Corresponding author.
E-mail address:bam040880@yahoo.com(B.Morganstern).
Peer review under responsibility of Shanghai Medical Association and SMMU.
http://dx.doi.org/10.1016/j.ajur.2015.08.005
2214-3882/?2015 Editorial Office of Asian Journal of Urology.Production and hosting by Elsevier(Singapore)Pte Ltd.This is an open access article under the CC BY-NC-ND license(http://creativecommons.org/licenses/by-nc-nd/4.0/).
 Asian Journal of Urology2015年4期
Asian Journal of Urology2015年4期
- Asian Journal of Urology的其它文章
- Contemporary outcomes in the detection of prostate cancer using transrectal ultrasound-guided 12-core biopsy in Singaporean men with elevated prostate specific antigen and/or abnormal digital rectal examination
- Diagnosis and management of ureteral complications following renal transplantation
- Three-dimensional printing technique assisted cognitive fusion in targeted prostate biopsy
- Does the presence of a percutaneous renal access influence fluoroscopy time during percutaneous nephrolithotomy?
- Prostate chronic inflammation type IV and prostate cancer risk in patients undergoing first biopsy set:Results of a large cohort study
- Implication of ultrasound bladder parameters on treatment response in patients with benign prostatic hyperplasia under medical management
