The older the better:The characteristic of localized prostate cancer in Chinese men
Haifeng Wang,Xu Gao,Ziyu Fang,Xin Lu,Yan Wang, Chunfei Ma,Zhenkai Shi,Bo Yang,Shancheng Ren, Chuanliang Xu,Yinghao Sun*
Department of Urology,Changhai Hospital,Second Military Medical University,Shanghai,China
ASIAN FOCUS
The older the better:The characteristic of localized prostate cancer in Chinese men
Haifeng Wang1,Xu Gao1,Ziyu Fang1,Xin Lu,Yan Wang, Chunfei Ma,Zhenkai Shi,Bo Yang,Shancheng Ren, Chuanliang Xu,Yinghao Sun*
Department of Urology,Changhai Hospital,Second Military Medical University,Shanghai,China
Objective:To assess the clinicopathological features and overall survival between two groups of Chinese patients older or younger than 70 years after retropubic radical prostatectomy.
Prostate cancer;
Age;
Biochemical recurrence-free survival;
Radical prostatectomy
1.Introduction
In 2013,prostate cancer was the most commonly diagnosed malignancy and the second leading cause of cancerrelated death in men in America[1].However,the incidence rate of prostate cancer in China is signif i cantly lower.A study had reported a 26-fold higher incidence rate of prostate cancer in American than in Chinese men with an intermediate rate in Chinese-American men.Such differences may be due to genetic and/or environment factors[2].An RNA-seq study using prostate cancer tissue from Chinese patients found two novel gene fusions which appear to be specif i cally associated with Chinese patients [3].In this article,we will reveal an age-related Chinese people specif i c feature.
2.Patients and methods
From January 2001 to February 2010,a cohort of 390 men underwent retropubic radical prostatectomy in our institution for the treatment of clinically localized prostate cancer.Eighty-nine cases were excluded because of insuff i cient clinical data,adjuvant or neoadjuvant hormonal therapy,and radiotherapy.The remaining 301 cases were included in the study and divided into two groups based on age,with 161(53.5%)men aged?70 years and 140(46.5%)aged<70 years.
Two hundred and seventy-f i ve patients were diagnosed by ultrasound guided prostate biopsy,and 26 patients were diagnosed by Transurethral Resection of Prostate(TURP). Ultrasound and pelvic MRI or CT were performed before biopsy.The indications for prostate biopsy were prostate peripheral zone nodule detected by digital rectal examination(DRE),ultrasound,MRI or CT with any prostate specif i c antigen(PSA)level,or PSA Z 4e10 ng/mL and free PSA/total PSA<0.16 without detectable nodule,or PSA>10 ng/mL.In order to comparatively analyze the age related differences,we considered Gleason score,PSA and clinicalstage(Table1).Biochemicalrecurrencewas def i ned as two consecutive increasing PSA values of >0.2 ng/mL.
A Chi-square test and an independent test were used to perform a comparative analysis of clinical factors according to age.Univariate Cox regression model and KaplaneMeier analysis were used for examining the effect of age on the outcomes of biochemical recurrence-free survival(BCRFS). Mean overall follow-up for the analysis was 57 months.SPSS19.0 for Windows software(IBM,NY,USA)was used, and p<0.05 was considered statistically signif i cant.
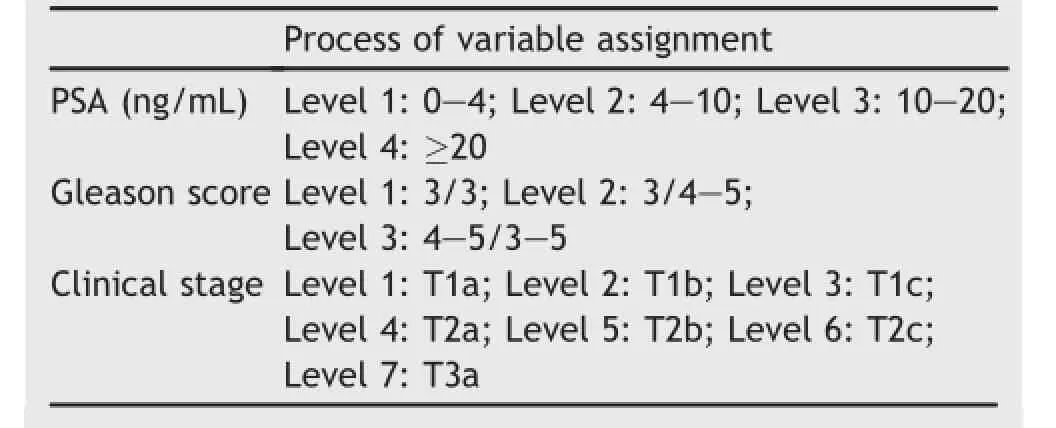
Table 1 Assignment of PSA,Gleason score and clinical stage.
3.Results
Demographics and clinical characteristics are described in Table 2.Except for PSA,there were no signif i cant differences in other parameters between the two groups.However,the low Gleason score(3/3)rate in older group (46.6%)was higher than that in younger group(41.4%).
Mean operation time was 200 min(range:150e300 min). Average blood loss was 230(100e1100)mL.Among the 301 patients,rectum injury rate was 1.0%(3 cases),and lymphatic leakage rate was 1.99%(6 cases).The 1 year, 2 years,3 years and 5 years BCRFS rate were 95.0%(286 cases),92.0%(277 cases),91.0%(274 cases)and 89.4%(269 cases).The 5 year BCRFS rate of the old group was 92.5% (149 in 161 cases),and it 85.7%(120 in 140 cases)in young group.
We analyzed the relationship between the four factors and 5 years BCRFS rate.The PSA and clinical stage were positive risk factors,and age was a negative risk factor. There was no relation between Gleason score and 5 years BCRFS rate(Table 3).The survival analysis of different age groups showed that the older patients had higher BCRFS rate than that of the younger patients(Fig.1).
4.Discussion
As radical prostatectomy is traditionally recommended for patients with longer than 10 years life expectancy,many surgeons intend to offer radical surgery to patients aged ?70 years[4].However,with the rapidly increasing elderly population and prolonged life expectancy,more and more old(?70 years)patients with localized prostate cancer will have longer than 10 years life expectancy[5,6].How to manage these patients become an important issue.It is important to know the outcomes of radical prostatectomy for those patients.
Several articles had focused on this question,however, the result seemed controversial.In 2008,an US study of 4035 patients demonstrate that even though the older patients had higher clinical stage,pathology Gleason sums and a lower frequency of organ-conf i ned disease,there was no difference in cancers specif i c survival or biochemical progression-free probability between the younger and older patents[7],and similar opinion appeared in another US study[8].With the advent of new robotic assisted RP technique,the result seemed to be conf i rmed.In a RARP study,Greco observed that except for a higher pathological Gleason grade and longer time to return to driving,outcomes of older patients are largely comparable to that in younger patients[9].However,Pf i tzenmaier et al.[10] analyzed 626 RP patients in Germany,and showed that the 10-year PSA-free survival was 51.8%for the younger and 57.4%for the older patients respectively.Another American and British study showed the similar result[11,12].In Asia, biochemical recurrence are more likely in older Korean and Japanese patients[13,14].Although these results are controversial,it appeares that older patients have no better outcome than the young patients.
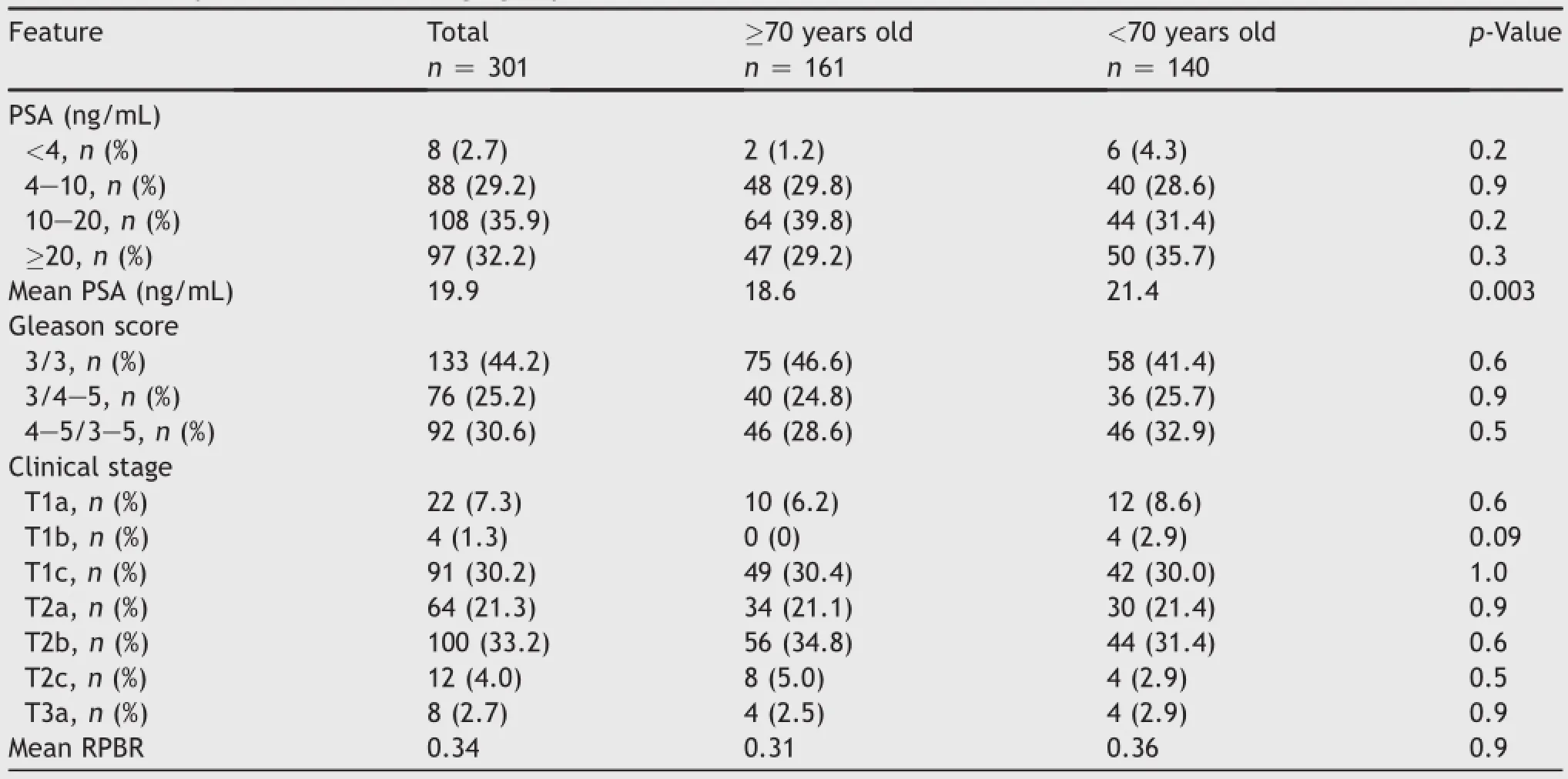
Table 2 Comparison of different age groups in clinical features.
Our present study showed that older patients have better outcomes than young patients.When we reviewed the previous studies,we found that those studies were based on the population of developed countries in which PSA screening is universal.Compared to these patients, Chinese patients have two unique characteristics.First, cancer in most of the Chinese patients was not detected by PSA screening.Because most patients with localized prostate cancers have few symptoms,the detection of prostate cancer is mostly depended on self medical awareness.As a result,poor medical awareness can delay the detection of prostate cancer in China.Because young Chinese patients are relatively healthier and busier than older patients who usually have more free time and more likely to go to hospital because of other diseases.Thus the prostate cancer diagnoses of older patients canbe conf i rmed timely due to better medical awareness.The detections of prostate cancer of young patients are relatively delayed because of the relatively poor medicalawareness.Second,environmental and genetic factors may also contribute to the differences.
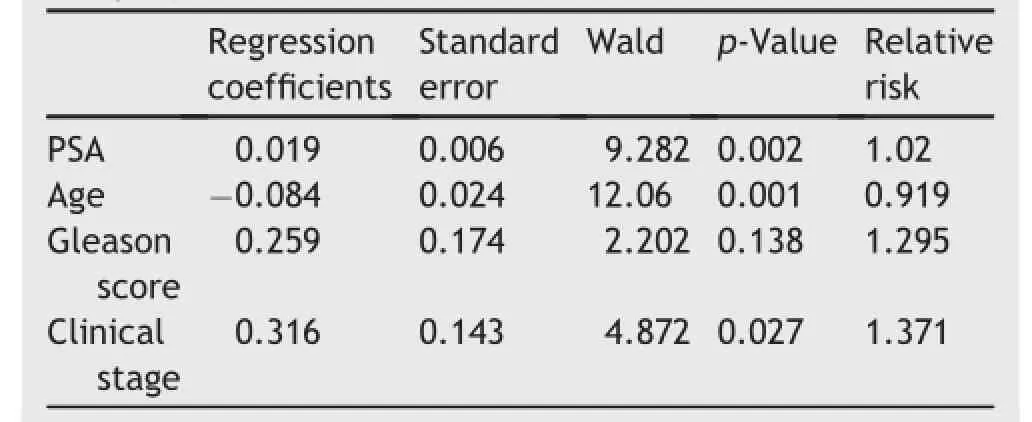
Table 3 The relationship between risk factors and 5 years biochemical recurrence survival(result of Cox regression analysis).
5.Conclusion
To conclude,the Chinese prostate cancer patients have unique characteristics compared with patients in developed countries’.Elderly patients(?70 years)have betteroutcome than younger patients(<70 years).If the physical condition permits,old age should not exclude patients from radical prostatectomy.
Conf l icts of interest
The authors declare no conf l ict of interest.
[1]Siegel R,Naishadham D,Jemal A.Cancer statistics,2013.CA Cancer J Clin 2013;63:11e30.
[2]Yu H,Harris RE,Gao YT,Gao R,Wynder EL.Comparative epidemiology of cancers of the colon,rectum,prostate and breast in Shanghai,China versus the United States.Int J Epidemiol 1991;20:76e81.
[3]Ren S,Peng Z,Mao JH,Yu Y,Yin C,Gao X,et al.RNA-seq analysis of prostate cancer in the Chinese population identif i es recurrent gene fusions,cancer-associated long noncoding RNAs and aberrant alternative splicings.Cell Res 2012; 22:806e21.
[4]Fowler Jr FJ,McNaughton CM,Albertsen PC,Zietman A, Elliott DB,Barry MJ.Comparison of recommendations by urologistsandradiationoncologistsfortreatmentof clinicallylocalizedprostatecancer.JAMA2000;283: 3217e22.
[5]Centers for Disease Control and Prevention(CDC).Trends in agingeUnited States and worldwide.MMWR Morb Mortal Wkly Rep 2003;52:101e4.106.
[6]Minino AM,Smith BL.Deaths:preliminary data for 2000.Natl Vital Stat Rep 2001;49:1e40.
[7]Richstone L,Bianco FJ,Shah HH,Kattan MW,Eastham JA, Scardino PT,et al.Radical prostatectomy in men aged>or Z70 years:effect of age on upgrading,upstaging,and the accuracy of a preoperative nomogram.BJU Int 2008;101: 541e6.
[8]SiddiquiSA,SenguptaS,SlezakJM,BergstralhEJ, Leibovich BC,Myers RP,et al.Impact of patient age at treatment on outcome following radical retropubic prostatectomy for prostate cancer.J Urol 2006;175:952e7.
[9]Greco KA,Meeks JJ,Wu S,Nadler RB.Robot-assisted radical prostatectomy in men aged>or Z70 years.BJU Int 2009;104: 1492e5.
[10]Pf i tzenmaier J,Pahernik S,Buse S,Haferkamp A,Djakovic N, Hohenfellner M.Survival in prostate cancer patients>or Z70 years after radical prostatectomy and comparison to younger patients.World J Urol 2009;27:637e42.
[11]Brassell SA,Rice KR,Parker PM,Chen Y,Farrell JS,Cullen J, et al.Prostate cancer in men 70 years old or older,indolent or aggressive:clinicopathological analysis and outcomes.J Urol 2011;185:132e7.
[12]Xu DD,Sun SD,Wang F,Sun L,Stackhouse D,Polascik T,et al. Effect of age and pathologic Gleason score on PSA recurrence: analysis of 2911 patients undergoing radical prostatectomy. Urology 2009;74:654e8.
[13]Kim JK,Cho SY,Jeong CW,Lee SB,Ku JH,Hong SK,et al. Patients aged more than 70 had higher risk of locally advanced prostate cancers and biochemical recurrence in Korea.BJU Int 2012;110:505e9.
[14]Masuda H,Fukushima H,Kawakami S,Numao N,Fujii Y, Saito K,et al.Impact of advanced age on biochemical recurrence after radical prostatectomy in Japanese men according to pathological stage.Jpn J Clin Oncol 2013;43:410e6.
Received 25 June 2015;received in revised form 3 July 2015;accepted 6 July 2015 Available online 14 July 2015
*Corresponding author.
E-mail address:sunyh@medmail.com.cn(Y.Sun).
Peer review under responsibility of Shanghai Medical Association and SMMU.
1These authors contributed equally to this study.
http://dx.doi.org/10.1016/j.ajur.2015.07.001
2214-3882/a2015 Editorial Off i ce of Asian Journal of Urology.Production and hosting by Elsevier(Singapore)Pte Ltd.This is an open access article under the CC BY-NC-ND license(http://creativecommons.org/licenses/by-nc-nd/4.0/).
Methods:From January 2001 to February 2010,390 patients receive dretropubic radical prostatectomy.After excluding 89 patients with adjuvant or neoadjuvant hormonal therapy or radiotherapy,a total of 301 patients were included in this study.We arbitrarily divided these patients into younger age group(<70 years,140 cases,46.5%)and older age group(?70 years, 161 cases,53.5%).The differences in serum prostate specif i c antigen(PSA),Gleason score, clinical tumor stage,and biochemical-free survival were analyzed between the two groups. Results:There were not signif i cant differences between the two groups in high Gleason score rate and clinical tumor stage.However,older patients had signif i cantly lower biochemical recurrence rate than those of younger patients,and had signif i cantly higher PSA levels.Multivariate analysis showed that older age,PSA level and clinical tumor stage were signif i cantly associated with biochemical recurrence free survival.
Conclusion:In Chinese men,older age(?70 years)is associated with better outcome.If the physical condition permits,older age alone should not exclude patients from radical prostatectomy.
 Asian Journal of Urology2015年3期
Asian Journal of Urology2015年3期
- Asian Journal of Urology的其它文章
- Evaluation of kidney allograft status using novel ultrasonic technologies
- Pygopus 2 promotes kidney cancer OS-RC-2 cells proliferation and invasion in vitro and in vivo
- The likelihood of having serum level of PSA of?4.0 ng/mL and?10.0 ng/mL in non-obese and obese Nigerian men with LUTS
- Does varicocele grade predict the postoperative changes of semen parameters following left inguinal micro-varicocelectomy?
- Serum cystatin C can be used as a marker of renal function even in patients with intestinal urinary diversion
- Isolated penile urethral injury:A rare case following male coital trauma
