Comparison of ultrasound-measured properties of the common carotid artery to tobacco smoke exposure in a cohort of Indonesian patients
Allen R. Yu, Bima Hasjim, Luke E. Yu, Christopher Gabriel, Alexander Anshus, Jonathan B. Lee, Michael J.Louthan, Esther C. Kim, Katrina Lee, Christina Tse, Thomas Keown, Shadi Lahham, Maili Alvarado, Steven Bunch, Abdulatif Gari, J. Christian Fox, School of Medicine, University of California, Irvine, USA
2 Department of Emergency Medicine, University of California, Irvine, USA
Comparison of ultrasound-measured properties of the common carotid artery to tobacco smoke exposure in a cohort of Indonesian patients
Allen R. Yu1, Bima Hasjim1, Luke E. Yu1, Christopher Gabriel1, Alexander Anshus1, Jonathan B. Lee1, Michael J.Louthan1, Esther C. Kim1, Katrina Lee1, Christina Tse1, Thomas Keown1, Shadi Lahham2, Maili Alvarado2, Steven Bunch2, Abdulatif Gari2, J. Christian Fox1,21School of Medicine, University of California, Irvine, USA
2Department of Emergency Medicine, University of California, Irvine, USA
BACKGROUND: The purpose of this study was to use point-of-care ultrasound (POCUS) to investigate the relationship between tobacco smoke exposure and the characteristics of the common carotid artery (CCA). The effect of both primary and secondary smoking on CCA properties was evaluated.
METHODS: We performed a prospective cross-sectional study across 20 primary care clinics in Bandung, West Java, Indonesia in July 2016. Point of care ultrasound was performed on a convenience sample of Indonesian patients presenting to clinic. The CCA wall stiffness and carotid intima-media thickness (CIMT) were measured during diastole and systole. These measurements were correlated with smoke exposure and cardiovascular disease.
RESULTS: We enrolled 663 patients in the study, with 426 patients enrolled in the smoking category and 237 patients enrolled in the second-hand smoke category. There was an overall positive correlation with the measured lifestyle factors and the ultrasound-measured variables in the group of individuals who smoked. For all variables, age seemed to contribute the most out of all of the lifestyle factors for the positive changes in CIMT and CCA wall stiffness.
CONCLUSION: Our data yielded correlations between CCA properties and cardiovascular risk,as well as between CIMT and arterial stiffness. We were also able to demonstrate an increase in thickness of the CIMT in patients who have been exposed by tobacco through the use of ultrasound.Further large scale studies comparing patients with multiple cardiac risk factors need to be performed to conf i rm the utility of ultrasound fi ndings of cardiovascular disease and stroke.
Carotid artery thickness; Point of care ultrasound; Indonesia; Intimal thickness
INTRODUCTION
Indonesia has one of the highest incidences of smoking in the world, with 72% of the male population over 15 years of age using tobacco products.[1]Worldwide,smoking is known to be a significant lifestyle factor that contributes to the development of stroke and coronary artery disease.[2]According to the CDC, smoking is the leading cause of death in Indonesia, contributing to 8%of all deaths in the country.[3]
Smoking has been shown to cause inflammatory vascular changes that can alter the structural and functional properties of blood vessels such as carotid local stiffness and carotid intima-media thickness (CIMT),both of which correlate directly with future cardiovascular events.[1,2]Increased carotid arterial stiffness is a condition seen in patients with cardiovascular risk factors such as hypertension, diabetes, and atherosclerosis.[4,5]Studies investigating the associations between smoking and carotid arterial stiffness give heterogeneous results and are limited particularly regarding local stiffness.[6–9]Although increased CIMT has also been positively correlated with development of atherosclerosis and future cardiovascular events, its clinical significance and predictive value for future cardiovascular events is not clear.[10,11]When used in conjunction with current cardiovascular risk factors,CIMT was not shown to improve assessment of risk for future acute cardiovascular events.[12,13]Furthermore,attempts to correlate increased CIMT and increased stiffness are not always definitive.[14,15]
Exposure to second-hand smoke (SHS) has also been associated with development of cardiovascular risk factors.[16]SHS exposure, like primary smoking, has also been positively correlated with CIMT in both a dosedependent manner and based on experiences in early childhood.[17]There is currently a lack of research on the effects of SHS on arterial stiffness on adults. B-mode and M-mode ultrasound are relatively easy and portable methods to effectively measure measuring CIMT[18]and indices of stiffness.[4,19,20]Measurement of stiffness and CIMT in the common carotid artery (CCA) alone has been shown to be sufficient to evaluate properties of the entire carotid artery.[21,22]
The purpose of this study was to use point-of-care ultrasound (POCUS) to investigate the relationship between tobacco smoke exposure and the physical characteristics of the CCA which include CIMT and carotid stiffness. The effect of both primary and secondary smoking on CCA properties was evaluated.Furthermore, CCA properties were compared between patients with previous history of cardiovascular event(myocardial infarction, cerebrovascular accident) and patients with no such history.
METHODS
Study design and population
We performed a prospective cross-sectional study across 20 different primary care clinics affiliated with the public health department of Bandung, West Java,Indonesia between July 1, 2016 and August 1, 2016.Data was collected from a convenience sample of Indonesian patients presenting to clinic for any chief complaint. In order to optimize homogeneity of the participants and decrease potential confounding factors,any family members of patients accompanying the patients and clinic employees were also approached for enrollment in the study. The study was approved by the site Institutional Review Board and complied with all guidelines of human subject research. All participants gave verbal and written consent for study enrollment.
Data collection and ultrasound measurements
Following consent, we gave participants a questionnaire to obtain self-reported demographic and health information including age, BMI, current smoking status, past medical history, and medications. After completion of the questionnaire, we placed participants in a supine position and allowed to rest for 5 minutes. The rest period was allotted to allow for equilibration of blood pressure and heart rate to baseline levels and to minimize white coat hypertension.
We measured blood pressure and heart rate twice from each arm of the participant via a manual sphygmomanometer.The average between these measurements was used. We did not obtain any localized carotid blood pressures. The participants underwent a point of care ultrasound using a Nanomaxx Ultrasound System (SonoSite, Bothell,Washington) connected to a linear 7.5 MHz probe. The right CCA was visualized with B-mode in a longitudinal view. With minimal pressure to avoid compression of the participant's vasculature, a 1-cm long segment of the CCA just proximal to the carotid bulb was captured and stored.Using this still image, we then manually measured CIMT of the far wall using internal software on the ultrasound machine. Finally, we utilized M-mode to capture the movement of both the near and far walls of the carotid as well as the carotid diameter measurements for each during diastole and systole. After scanning was complete, we again measured blood pressure and heart rate.
Statistical analysis
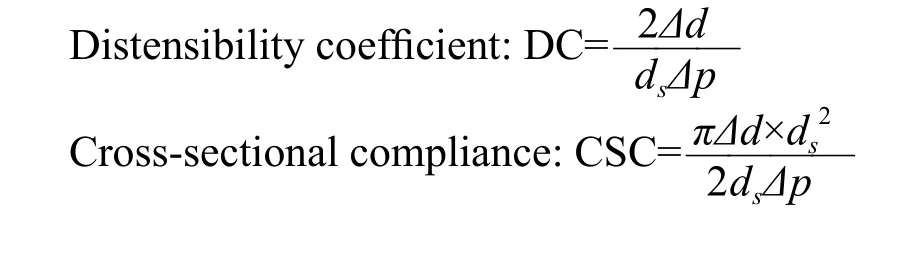
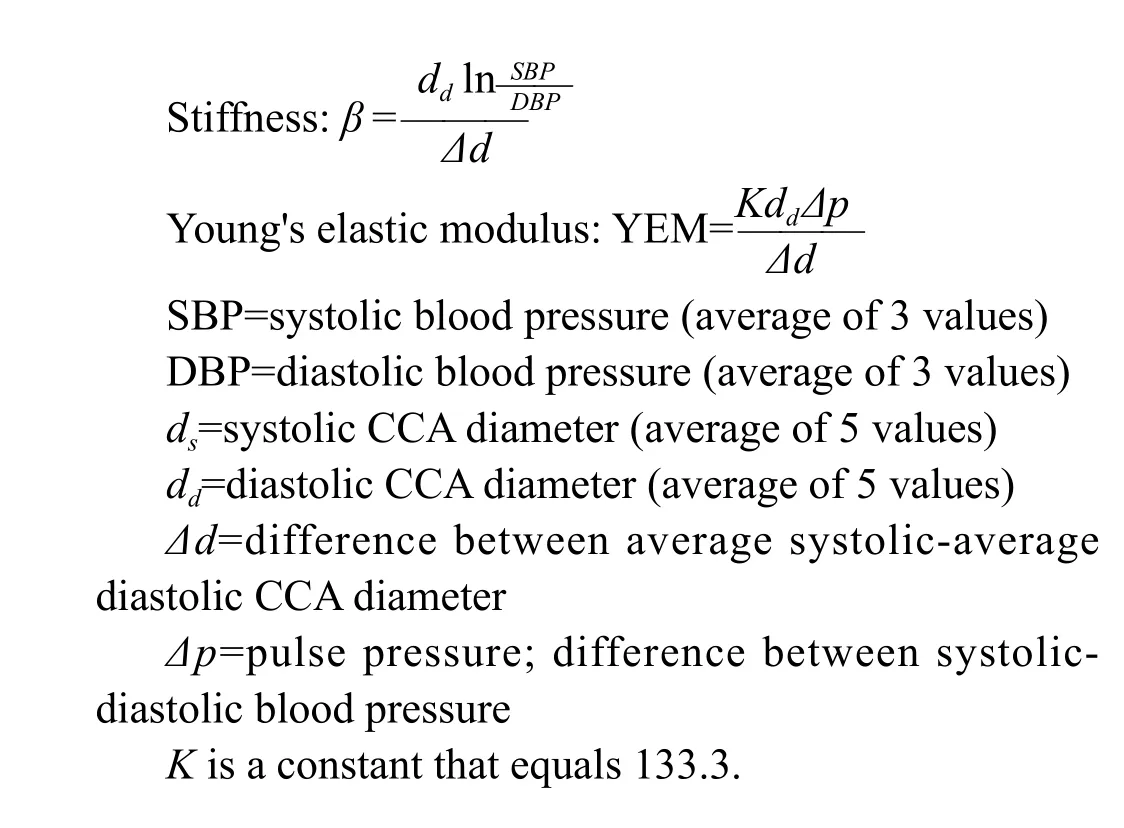
We performed data analysis using VassarStats website for statistical computation (Vassar College, Poughkeepsie,NY). Multiple regression was performed to compare the exposure of tobacco smoke to CIMT and values of arterial distensibility. We also incorporated other factors associated with increased CIMT and carotid arterial stiffness, including age, BMI, gender, and presence of cardiovascular risk factors in the analysis. Linear regression was performed to examine associations of CIMT with each measure of carotid arterial stiffness. We also performed a two-sided t-test to compare the CIMT and arterial distensibility of participants with positive history of acute cardiovascular events versus those of patients without such history. We averaged the blood pressure and the CCA diameter data to calculate the following indices of carotid stiffness: distensibility coefficient (DC), cross-sectional compliance, arterial stiffness, and Young's elastic modulus.
RESULTS
We enrolled a total of 663 patients in the study.426 patients had a history of smoking and 237 patients had a history of second-hand smoke exposure, and 73 patients had neither smoked or been exposed to SHS.Full demographic data can be seen in Table 1. Compared to nonsmokers, the smoking group was older, had a higher proportion of males, exhibited increased CIMT,and exhibited decreased DC (Table 2). All 426 patients were included in the multiple regression between primary smoking and measured properties of the CCA. In a multivariate regression model with age and BMI, there was an overall positive association with the measured lifestyle factors (age, BMI, presence of cardiovascular risk factors)and the ultrasound-measured variables in the group of individuals who smoked. There was a positive association between all vascular health variables (with the exception of CSC), and the measured factors. With the exception of CSC, all of the adjusted R2values were statistically significant (Table 3). For all 4 statistically significant variables, age seemed to contribute the most out of all of the lifestyle factors for the variation between individuals. In the individuals exposed to SHS, YEM and CIMT was positively associated with measured lifestyle factors (Table 4). Multiple regression with CIMT showed an adjusted R2value of0.2741, the highest among the multiple regressions. BMI contributed the most out of all of the lifestyle factors for the variation between individuals in the stiffness analysis. Age contributed the most for variation between individuals in the CIMT analysis. In the smoking group, there was a very weak positive association between CIMT and distensibility (Table 5). The 243 patients that had not smoked previously were included in the multiple regression between SHS exposure and CCA properties (Table 5). In the SHS regression, there were very weak positive associations between CIMT and stiffness, as well as CIMT and YEM (Table 6). Patients with history of acute cardiovascular event had significantly decreased CCA distensibility relative to patients without history of cardiovascular event (Table 7, Figure 1). Patients with history of MI/CVA also trended towards having a higher CIMT than individuals without such history, but the comparison did not reach statistical significance (Table 8,Figure 2). Other CCA values showed no significance when compared to presence of MI/CVA in the history.
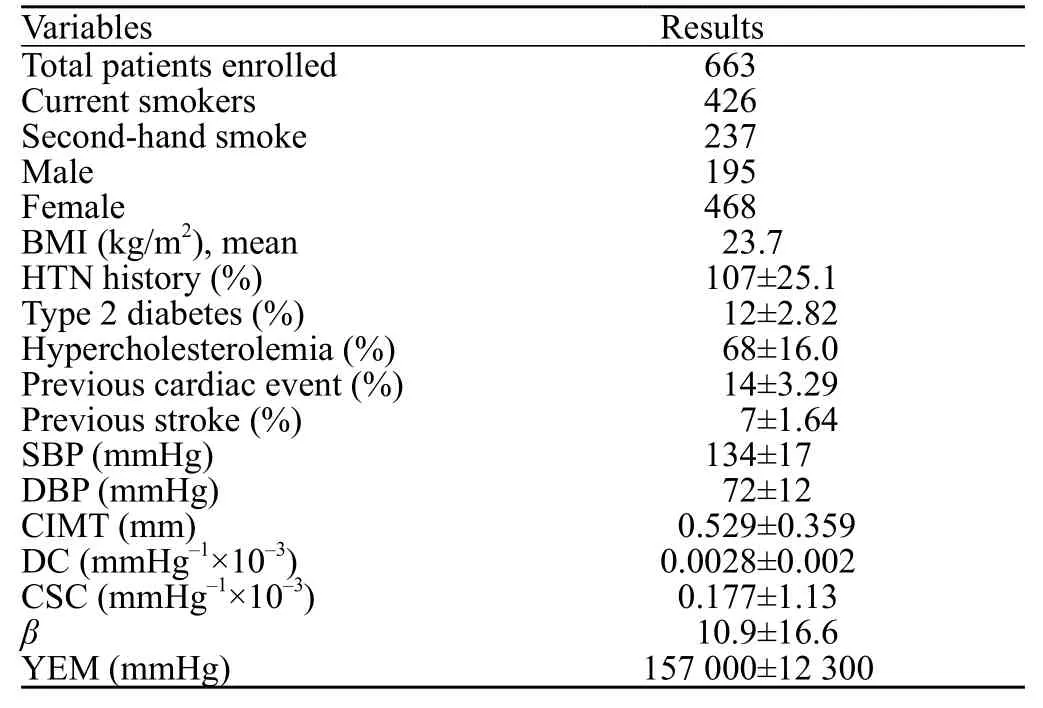
Table 1. Basic patient demographics, past medical history and ultrasound measured characteristics

Table 2. Comparison of patient characteristics between smokers and nonsmokers

Table 3. Multiple regression correlating smoking history with ultrasound fi ndings
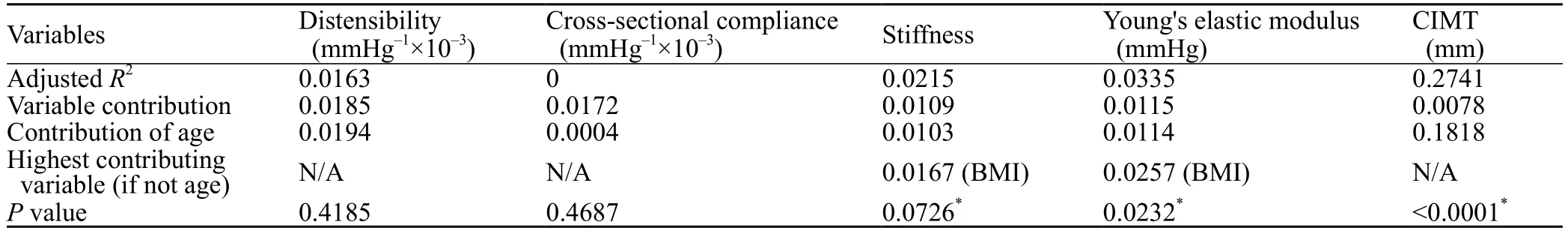
Table 4. Multiple regression correlating SHS exposure with ultrasound findings
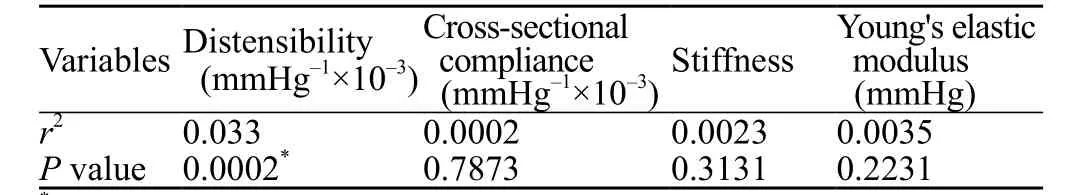
Table 5. CIMT vs. stiffness measure in patients with current smoking
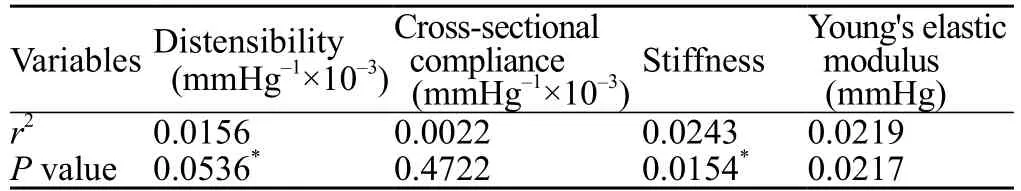
Table 6. CIMT vs. stiffness measure in patients with SHS exposure
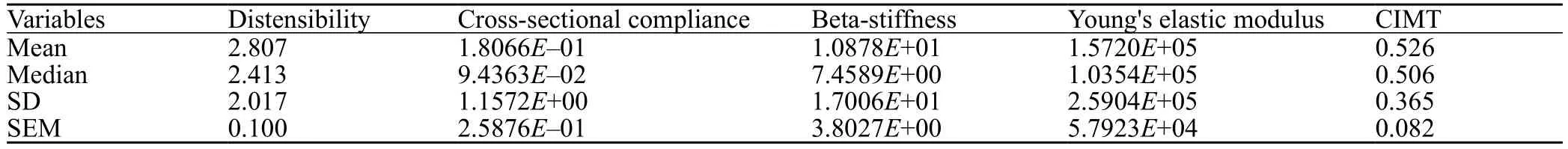
Table 7. CCA values in individuals without history of cardiovascular events
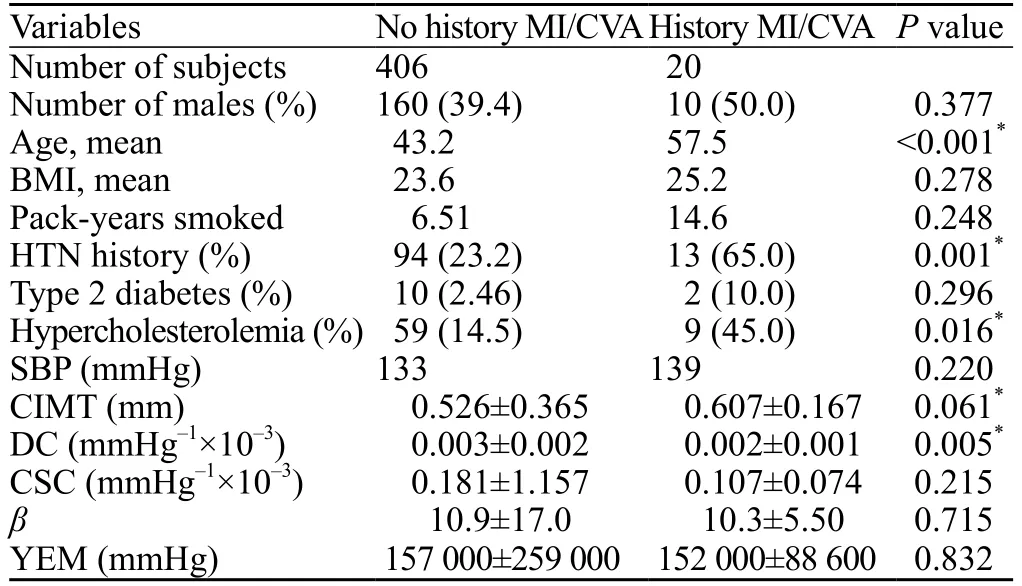
Table 8. CCA values in individuals with history of cardiovascular events

Figure 1. Distensibility coeff i cient vs. history of cardiovascular event(P=0.0050).
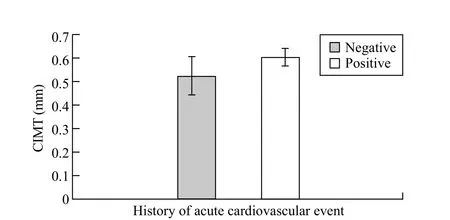
Figure 2. CIMT vs. history of cardiovascular event (P=0.0608).
DISCUSSION
We found that our primary dependent variable, carotid distensibility, exhibited a weakly positive association with the measures of cardiovascular risk that we measured. Age seemed to be the greatest contributing factor to increased arterial distensibility, which is consistent with previous studies.[23]The effect of smoking seemed to be negligible.This finding of increasing distensibility, especially in older age, was unexpected. Traditionally, increasing age has been tied with increased stiffness,[24]and this relationship has been shown prospectively as well.[25]
Associations between tobacco smoke exposure and CIMT were more consistent across both smokers and individuals exposed to second-hand smoke, although the association was surprisingly much stronger for individuals exposed to SHS than for smokers. The strength of the associations may have been diminished because we did not account for the number of smoke-free years in former smokers. We also did not assess whether participants were currently or formerly exposed to SHS.Rather, all participants were placed into the regression model as if everyone were currently smoking or exposed to SHS. Smoking cessation has been associated with a significant decrease in cardiovascular disease-related mortality.[26]However, the limited research on smoking cessation and properties of the carotid artery are conflicting.[26,27]The abrupt decrease in mortality may likely be multifactorial.
While abundant evidence supports the positive association between exposure to tobacco smoke and increased CIMT, the associations for carotid arterial stiffness are much less clear. Previous attempts to make associations between smoking and measures of carotid arterial stiffness have not shown clear results.[11,28]Interestingly, Sharrett et al[28]and Meyer et al[29]both found that tobacco smoke exposure was actually associated with decreased arterial stiffness, which is consistent with our findings. Decreased arterial stiffness could explain how individuals who smoke exhibit increased risk of mortality from abdominal aortic aneurysm (AAA). Indeed, smoking has been described as the largest modifiable risk factor for AAA.[30–32]The exact mechanism of development of AAA from smoking is not well understood currently.[33]
When it came to history of cardiovascular and cerebrovascular disease, our data was much more consistent with the literature. In patients with previous history of MI or CVA, there was a significant decrease in DC relative to patients who did not report any such conditions. Patients with previous MI or CVA also tended to have increased CIMT relative to patients without, although this value did not quite reach statistical significance. The lack of significance can be attributed to the relatively small sample size of individuals who had suffered these previous episodes.Our findings are consistent with findings in the literature that increased stiffness and CIMT are associated with greater risk of cardiovascular disease and stroke.[13,34]
One possible reason for the weak associations between tobacco smoke exposure and CCA properties may have been that cardiovascular risk factors were selfreported. We did not have access to subject medical records and therefore could not provide specif i c values for parameters such as their cholesterol levels. Additionally,it was not possible to confirm the subject's past medical history (including smoking history), medications that they were taking, and their compliance with their medications.We could only assess CV risk using the presence of risk factors such as hypertension, hypercholesterolemia and diabetes, but we may have seen higher correlation with CV risk and measures of stiffness and CIMT had we had access to more specif i c information.[35]
Variation in the scanning protocol may have additionally decreased the effect sizes that we were hoping to observe.Many of the patients had not previously encountered foreigners, and having the measurements and scans performed by foreigners may have caused or exacerbated white coat hypertension in these individuals. These factors may have falsely elevated the blood pressure, leading to inaccurate calculations of stiffness indices. Elevated heart rates have also been shown to negatively correlate with carotid artery .[36]Anatomical differences may also have played a role. While performing M-modistensibilityde measurements, it was occasionally impossible to display the CCA in a completely horizontal plane. As a result, alignment of both near and far walls of the CCA to measure systolic and diastolic diameter could not be performed perfectly,which may have resulted in deviations in measurements.
Overall associations between CIMT and indices of carotid stiffness were almost negligible. Measures of CIMT have been shown to be highly variable based on the protocol.[12]Though we tried to minimize variation by using the software within the Nanomaxx, anatomical variation may have affected measurements. There were occasionally patients for whom we could not easily visualize the tunica intima in B-mode. When compared, values of stiffness and CIMT have not been shown to correlate well with each other in previous studies, nor are they equally capable of predicting future cardiovascular risk.[37–39]
A factor which we did not take into consideration when performing our analysis was ambient pollution.The literature on pollution and its effect on vascular properties remains conflicted. Some studies have demonstrated effects of pollution on atherosclerosis and cardiovascular mortality,[40,41]especially in Asians versus other races.[42]Pollution has been shown to increase both stiffness and CIMT.[40,43]However, other studies have found no significant changes in these measures.[44–46]As with cigarette smoke itself, the sheer number of diverse chemicals in air pollution make it difficult to study its exact effect on a specif i c vascular parameter.
Limitations
There are several limitations to our study. First, the study was performed at a single site in rural primary care clinics in Bandung, West Java, Indonesia. It is possible that patients from different geographic regions or backgrounds may have different ultrasound findings.Next, the convenience sampling of patients may have the potential for selection bias although this was limited by the fact that every patient present was approached for enrollment. Several aspects of data were self-reported from patients. This included height, weight and past medical history. Another limitation of our study is that carotid distensibility was calculated using peripheral blood pressure measurements instead of central blood pressure. This factor must be taken into account when comparing our studies to previous work. Our most significant limitation is that we did not quantify the length of smoking history. It is possible that patients with a longer smoking history could have more identifiable findings on ultrasound. Future large scale, multi-centered studies are needed to validate our promising findings.
CONCLUSION
Our data yielded weak associations between carotid distensibility and cardiovascular risk, as well as between CIMT and carotid arterial stiffness. However, we were able to demonstrate an increase in thickness of the CIMT in patients who have been exposed by tobacco through the use of ultrasound. Interestingly, patients who had been exposed to SHS had thicker CIMTs compared to those who smoke directly. Our study also displayed the promise of using ultrasound to confirm the relationship between a lower DC and thicker CIMT with risk of cardiovascular disease and stroke. To further support this claim, further large scale studies comparing patients with multiple cardiac risk factors need to be performed to confirm the utility of ultrasound findings for cardiovascular disease and stroke.
ACKNOWLEDGMENTS
UC Irvine Health Department of Emergency Medicine, UC Irvine School of Medicine.
Funding: None.
Ethical approval: The study was approved by the site Institutional Review Board and complied with all guidelines of human subject research.
Conflicts of interest: Dr. J Christian Fox receives stock options from Sonosim for consulting. However, no Sonosim products were used in this research project. No other authors have any disclosures.Contributors: Yu AR proposed the study, analyzed the data and wrote the first drafts. All authors contributed to the design and interpretation of the study and to further drafts.
1 The World Bank Group. Smoking prevalence, males (%of adults). http://databank.worldbank.org/data/reports.aspx?source=2&series=SH.PRV.SMOK.MA&country=.Published 2016. Accessed January 15, 2016.
2 Wolf PA, D'Agostino RB, Kannel WB, Bonita R, Belanger A. Cigarette smoking as a risk factor for stroke. JAMA.1988;259(7):1025.
3 The Centers for Disease Control and Prevention (CDC). CDC in Indonesia Factsheet. Centers Dis Control Prev. 2013;(CDC):1-2. http://www.cdc.gov/globalhealth/countries/indonesia/pdf/indonesia.pdf www.cdc.gov/globalhealth/countries/indonesia/pdf/indonesia.pdf.
4 Kohn JC, Lampi MC, Reinhart-King CA. Age-related vascular stiffening: Causes and consequences. Front Genet.2015;6(MAR):1–17.
5 van Popele NM, Grobbee DE, Bots ML, Asmar R, Topouchian J, Reneman RS, et al. Association between arterial stiffness and atherosclerosis: the Rotterdam Study. Stroke. 2001;32(2):454–60.
6 Failla M, Effects of cigarette smoking on carotid and radial artery distensibility. J Hypertens. 1997;15(12 Pt 2):1659–64.
7. Camplain R, Meyer ML, Tanaka H, Palta P, Agarwal SK, Aguilar D, et al. Smoking behaviors and arterial stiffness measured by pulse wave velocity in older adults: The Atherosclerosis Risk in Communities (ARIC) Study. Am J Hypertens. 2015 Dec 10. pii:hpv189.
8. Maloberti A. Structural and functional abnormalities of carotid artery and their relation with EVA phenomenon. High Blood Press Cardiovasc Prev. 2015;22(4):373–9.
9. Gaibazzi N. Differential incremental value of ultrasound carotid intima-media thickness, carotid plaque, and cardiac calcium to predict angiographic coronary artery disease across Framingham risk score strata in the APRES multicentre study. Eur Heart J Cardiovasc Imaging. 2016;17(9):991–1000.
10 O'Leary D, Polak J, Kronmal R, Manolio TA, Burke GL,Wolfson SK Jr. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. N Engl J Med. 1999;340(1):14–22.
11 McEvoy JW, Blaha MJ, DeFilippis AP, Lima JA, Bluemke DA, Hundley WG, et al. Cigarette smoking and cardiovascular events: role of inf l ammation and subclinical atherosclerosis from the MultiEthnic Study of Atherosclerosis. Arterioscler Thromb Vasc Biol. 2015;35(3):700–9.
12 Lorenz MW, Polak JF, Kavousi M, Mathiesen EB, V?lzke H,Tuomainen TP, et al. Carotid intima-media thickness progression to predict cardiovascular events in the general population (the PROG-IMT collaborative project): a meta-analysis of individual participant data. Lancet. 2012;379(9831):2053–62.
13 Zhang L, Yin JK, Duan YY, Liu X, Xu L, Wang J, et al.Evaluation of carotid artery elasticity changes in patients with type 2 diabetes. Cardiovasc Diabetol. 2014;13(10):39. .
14 Weberru? H, Pirzer R, B?hm B, Elmenhorst J, Pozza RD, Netz H, et al. Increased intima-media thickness is not associated with stiffer arteries in children. Atherosclerosis. 2015;242(1):48–55.
15 Doyon A, Kracht D, Bayazit AK, Deveci M, Duzova A, Krmar RT, et al. Carotid artery intima-media thickness and distensibility in children and adolescents: Reference values and role of body dimensions. Hypertension. 2013;62(3):550–6.
16 Carmona R. The 2006 Report of the Surgeon General. The Health Consequences of Involuntary Exposure to Tobacco Smoke. Am J Prev Med. 2007;32:542–543.
17 Chen W, Yun M, Fernandez C, Li S, Sun D, Lai CC, et al.Secondhand smoke exposure is associated with increased carotid artery intima-media thickness: The Bogalusa Heart Study.Atherosclerosis. 2015;240(2):374–9.
18 Lane HA, Smith JC, Davies JS. Noninvasive assessment of preclinical atherosclerosis. Vasc Health Risk Manag.2006;2(1):19–30.
19 Gamble G, Zorn J, Sanders G, MacMahon S, Sharpe N.Estimation of arterial stiffness, compliance, and distensibility from M-mode ultrasound measurements of the common carotid artery. Stroke. 1994;25(1):11–6.
20 Godia EC, Madhok R, Pittman J, Trocio S, Ramas R, Cabral D,et al. Carotid artery distensibility: a reliability study. J ultrasound Med. 2007;26(9):1157–65.
21 Law Y, Chan YC, Cheng SW. Endovascular repair of giant traumatic pseudo-aneurysm of the common carotid artery. World J Emerg Med. 2015;6(3):229–32.
22 Nambi V, Chambless L, He M, Folsom AR, Mosley T,Boerwinkle E, et al. Common carotid artery intimamedia thickness is as good as carotid intimamedia thickness of all carotid artery segments in improving prediction of coronary heart disease risk in the Atherosclerosis Risk in Communities(ARIC) study. Eur Heart J. 2012;33(2):183–90.
23 Benetos A, Waeber B, Izzo J, Mitchell G, Resnick L, Asmar R, et al. Influence of age, risk factors, and cardiovascular and renal disease on arterial stiffness: clinical applications. Am J Hypertens. 2002;15(12):1101–8.
24 Kawasaki T, Sasayama S, Yagi S, Asakawa T, Hirai T. Noninvasive assessment of the age related changes in stiffness of major branches of the human arteries. Cardiovasc Res.1987;21(9):678–87.
25 Gepner AD, Korcarz CE, Colangelo LA, Hom EK, Tattersall MC, Astor BC, et al. Longitudinal effects of a decade of aging on carotid artery stiffness: The multiethnic study of atherosclerosis.Stroke. 2014;45(1):48–53.
26 Johnson HM, Piper ME, Baker TB, Fiore MC, Stein JH.Effects of smoking and cessation on subclinical arterial disease:A substudy of a randomized controlled trial. PLoS One.2012;7(4):1–6.
27 Kweon S, Lee Y, Shin M, Choi JS, Rhee JA, Choi SW, et al.Effects of cumulative smoking exposure and duration of smoking cessation on carotid artery structure. Circ J. 2012;76(8):2041–7.
28 Sharrett AR, Ding J, Criqui MH, Saad MF, Liu K, Polak JF, et al. Smoking, diabetes, and blood cholesterol differ in their associations with subclinical atherosclerosis: the Multiethnic Study of Atherosclerosis (MESA). Atherosclerosis.2006;186(2):441–7.
29 Meyer ML, Tanaka H, Palta P, Cheng S, Gouskova N, Aguilar D,et al. Correlates of segmental pulse wave velocity in older adults:The Atherosclerosis Risk in Communities (ARIC) Study. Am J Hypertens. 2016;29(1):114–22.
30 Norman PE, Curci JA. Understanding the effects of tobacco smoke on the pathogenesis of aortic aneurysm. Arterioscler Thromb Vasc Biol. 2013;33(7):1473–7.
31 Chang CM, Corey CG, Rostron BL, Apelberg BJ. Systematic review of cigar smoking and all cause and smoking related mortality. BMC Public Health. 2015;15(1):390.
32 Kent KC, Zwolak RM, Egorova NN, Riles TS, Manganaro A,Moskowitz AJ, et al. Analysis of risk factors for abdominal aortic aneurysm in a cohort of more than 3 million individuals. J Vasc Surg. 2010;52(3):539–48.
33 Kuivaniemi H, Ryer EJ, Elmore JR, Tromp G. Understanding the pathogenesis of abdominal aortic aneurysms. Expert Rev Cardiovasc Ther. 2015;13(9):975–87.
34 Sutton-Tyrrell K, Najjar SS, Boudreau RM, Venkitachalam L,Kupelian V, Simonsick EM, et al. Elevated aortic pulse wave velocity, a marker of arterial stiffness, predicts cardiovascular events in well-functioning older adults. Circulation.2005;111(25):3384–90.
35 Goff DC, Lloyd-Jones DM, Bennett G, Coady S, D'Agostino RB, Gibbons R, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: A report of the American college of cardiology/American heart association task force on practice guidelines. Circulation. 2014;129(25 Suppl 2):S49–73.
36 Whelton SP, Blankstein R, Al-Mallah MH, Lima JA, Bluemke DA, Hundley WG, et al. Association of resting heart rate with carotid and aortic arterial stiffness: Multi-ethnic study of atherosclerosis. Hypertension. 2013;62(3):477–84.
37 Lunder M, Janic M, Kejzar N, Sabovic M. Associations among different functional and structural arterial wall properties and their relations to traditional cardiovascular risk factors in healthy subjects: a cross-sectional study. BMC Cardiovasc Disord.2012;12:29.
38 Zoungas S, Cameron JD, Kerr PG, Wolfe R, Muske C, McNeil JJ, et al. Association of carotid intima-medial thickness and indices of arterial stiffness with cardiovascular disease outcomes in CKD. Am J Kidney Dis. 2007;50(4):622–30.
39 Zureik M, Temmar M, Adamopoulos C, Bureau JM, Courbon D, Thomas F, et al. Carotid plaques, but not common carotid intima-media thickness, are independently associated with aortic stiffness. J Hypertens. 2002;20(1):85–93.
40 Su TC, Hwang JJ, Shen YC, Chan CC. Carotid intima-media thickness and long-term exposure to traffic-related air pollution in middle-aged residents of Taiwan: A cross-sectional study.Environ Health Perspect. 2015;123(8):773–8.
41 Brook RD, Rajagopalan S, Pope CA, Brook JR, Bhatnagar A, Diez-Roux AV, et al. Particulate matter air pollution and cardiovascular disease: An update to the scientif i c statement from the american heart association. Circulation. 2010;121(21):2331–78.
42 Jones MR, Diez-Roux A V, O'Neill MS, Guallar E, Sharrett AR,Post W, et al. Ambient air pollution and racial/ethnic differences in carotid intima-media thickness in the Multi-Ethnic Study of Atherosclerosis (MESA). J Epidemiol Community Health.2015;69(12):1191–8.
43 Provost EB, Louwies T, Cox B, Op't Roodt J, Solmi F, Dons E,et al. Short-term fluctuations in personal black carbon exposure are associated with rapid changes in carotid arterial stiffening.Environ Int. 2016;88:228–34.
44 O'Neill MS, Diez-Roux AV, Auchincloss AH, Shen M, Lima JA, Polak JF, et al. Long-term exposure to airborne particles and arterial stiffness: The multi-ethnic study of atherosclerosis(MESA). Environ Health Perspect. 2011;119(6):844–51.
45 Lenters V, Uiterwaal CS, Beelen R, Bots ML, Fischer P, Brunekreef B, et al. Long-term exposure to air pollution and vascular damage in young adults. Epidemiology. 2010;21(4):512–20.
46 Gan WQ, Allen RW, Brauer M, Davies HW, Mancini GBJ,Lear SA. Long-term exposure to traff i c-related air pollution and progression of carotid artery atherosclerosis: a prospective cohort study. BMJ Open. 2014;4(4):e004743.
Accepted after revision May 6, 2017
Shadi Lahham, Email: slahham@uci.edu
World J Emerg Med 2017;8(3):177–183
10.5847/wjem.j.1920–8642.2017.03.003
December 22, 2016
 World journal of emergency medicine2017年3期
World journal of emergency medicine2017年3期
- World journal of emergency medicine的其它文章
- Emergency department procedural sedation for primary electrical cardioversion — a comparison with procedural sedations for other reasons
- The presenting and prescribing patterns of migraine in an Australian emergency department: A descriptive exploratory study
- Validating a point of care lactate meter in adult patients with sepsis presenting to the emergency department of a tertiary care hospital of a low- to middle-income country
- Can patients with non-convulsive seizure be identif i ed in the emergency department?
- Study on the development and usage of a cardiopulmonary resuscitation time point recorder
- Out of hospital cardiac arrest resuscitation outcome in North India — CARO study
