Persistent papules with adult?onset Still’s disease:a case report
Na-Na Zheng,Xiao-Xiao Yang,Jing-Xi Zhang,Lian-Sheng Zhong*
Department of Dermatology,Affiliated Hospital of Xuzhou Medical University,Xuzhou,Jiangsu 221002,China.
Introduction
Adult-onset Still’s disease(AOSD)is a systemic in fl ammatory disease with unknown etiology.It is classically characterized by a high spiking fever,evanescent rash,liver dysfunction,leukocytosis with neutrophilia, generalized lymphadenopathy, and splenomegaly.The typical skin rash of AOSD is evanescent,appearing and disappearing along with the rise and fall of the fever.However,recent reports have highlighted atypical rashes associated with AOSD,such as persistent pruritic plaques and papules.We herein report a case of AOSD with persistent pruritic papules on the chest in a 47-year-old woman,who was suspected of septicemia and lymphoma for more than 3 weeks before diagnosis confirmed.
Case report
A 47-year-old woman presented with a 3-week history of an intermittent high fever,throat pain,and pruritic papules on the chest in Affiliated Hospital of Xuzhou Medical University.Before hospitalization,she had been repeatedly treated with antibiotics and antipyretics with unsatisfactory curative effects at a local hospital.Her personal and family medical histories were unremarkable.
Physical examination revealed confluent erythematous papules with slight scales on the chest(Figure 1).Her fauces had a congestive appearance,and her lymph nodes were palpable on both sides of the neck.Polyarthralgia was obvious in her left wrist and right knee.Abnormal laboratory examination findings were leukocytosis(17.5×109/L)with 91.0%neutrophils,an elevated C-reactive protein level(76.9 mg/L),an elevated erythrocyte sedimentation rate(78 mm/h),and a high ferritin level(1,688 ng/ml).Her aspartate aminotransferase and alanine aminotransferase levels were118and57U/L,respectively.An infectious workup and extensive rheumatologic panel were otherwise negative.Awhole-body positron emission tomographycomputed tomography study showed enlarged lymph nodes in the bilateral neck and axillary and inguinal areas without involvement of other organs.Histopathologic examination of the pruritic papules showed hyperkeratosis with patchy parakeratosis,multiple areas of dyskeratosis confined to the upper layers of the epidermis,mild acanthosis,subtle vacuolar interface alteration,and a sparse dermal mixed infiltrate consisting of lymphocytes admixed with neutrophils and eosinophils(Figure 2).
The patient was therefore diagnosed with AOSD,and given intravenous methylprednisolone at a dosage of 60 mg daily and methotrexate at a dosage of 10 mg weekly.Her symptoms,including the fever and skin lesions,gradually improved and eventually disappeared.
Discussion
Still’s disease is divided into juvenile-onset Still’s disease(JOSD)and AOSD.The former includes JOSD involving one or a few joints,JOSD involving multiple joints,enthesitis-related JOSD,and psoriasis-related JOSD.AOSD is a systemic inflammatory disease classically characterized by intermittent high fevers,an evanescent eruption,polyarthralgia or arthritis,splenomegaly,and laboratory findings of leukocytosis together with negative antinuclear antibody[1].The diagnosis of AOSD can be very difficult and is of exclusion with no specific unified standard.In the present case,the patient developed a high spiking fever,sore throat,leukocytosis,lymphadenopathy,polyarthralgia,and atypical persistent erythematous papules.We performed examinations to exclude infectious diseases,malignancies,and other rheumatic immune diseases.The typical skin presentation of AOSD is an evanescent salmon pink or dark red rash that appears along with the rising of the fever;this presentation has been observed in up to 87%of patients[2]. Recently, several case reports have described a few atypical lesions of AOSD,especially a persistent skin rash consisting of pruritic plaques and papules with distinct histopathologic manifestations:single or aggregated areas of dyskeratosis in the upper layers of the epidermis associated with a perivascular inflammatory infiltrate in the upper and mid-dermis,without vasculitis[3-4].Other types of atypical rash have been reported,including urticarial erythema,prurigo pigmentosa-like lesions,diffuse cutaneous mucinosis,and linear hyperpigmen-tation with increased dermal mucin.In most cases,the atypical skin eruption presents at the time of disease onset concurrently with or shortly after the development of systemic symptoms.These atypical rashes often present together with the typical rash,but they are the only skin manifestation in about 43%of affected patients,leading to high rates of misdiagnosis and missed diagnosis because of under-recognition[5].
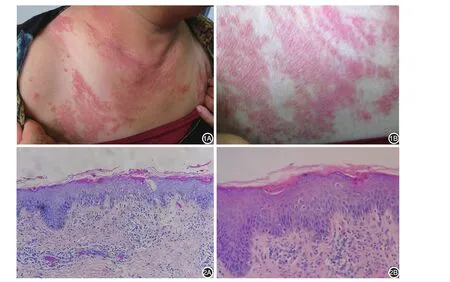
Figure 1 Erythematous papules with slight scales were present on the chest(A)with closer view(B).Figure 2 Histopathologic examination of the pruritic papules showed hyperkeratosis with patchy parakeratosis,multiple areas of dyskeratosis confined to the upper layers of the epidermis,mild acanthosis,subtle vacuolar interface alteration,and a sparse superficial and mid-dermal mixed infiltrate consisting of lymphocytes admixed with neutrophils and eosinophils.A:Hematoxylin-eosin staining,×100.B:Hematoxylin-eosin staining,×200.
At present,the treatment of AOSD remains empirical.Glucocorticoid(GC)is considered the first-line of AOSD treatment,can induce a clinical response in about 60% of patients.Disease-modifying antirheumatic drugs(DMARDs),including methotrexate(MTX),azathioprine(AZA)or leflunomide(LEF),are commonly used as second line therapy[6-7].Recently,multiple lines of evidence have suggested the role of biologics in refractory cases,such as anti-IL-1,anti-IL-6 and anti-IL-18 receptor agents,which have proved to be effective to control disease activity and its complications[8-9].Our patient was treated with methylprednisolone in combination with methotrexate,and achieved good clinical remission.
In conclusion,the appearance of a persistent atypical rash in patients with AOSD seems to be more frequent than expected,and persistent pruritic papules pathologically characterized by dyskeratotic keratinocytes may be significantly referable to the diagnosis of AOSD.It is important for dermatologists to recognize these clinical variants to make early diagnosis of AOSD.
- 國(guó)際皮膚性病學(xué)雜志的其它文章
- Paraneoplastic pemphigus comorbid with cardiac cancer and duodenal gastrointestinal stromal tumors:a rare case report
- Reactive perforating collagenosis
- Sun?protection knowledge and strategies of Chinese dermatologists:a nation?wide,questionnaire?based survey
- Initial presentation of acute myeloid leukemia in a patient with cutaneous myeloid sarcoma
- Primary vulvar melanoma in a 27?year?old pregnant woman:a case report and literature review
- Cutaneous plexiform schwannoma in the right thigh after trauma