End-stage liver disease score and future liver remnant volume predict post-hepatectomy liver failure in hepatocellular carcinoma
Fan-Hua Kong, Xiong-Ying Miao, Heng Zou, Li Xiong, Yu Wen, Bo Chen, Xi Liu, Jiang-Jiao Zhou
Fan-Hua Kong, Xiong-Ying Miao, Heng Zou, Li Xiong, Yu Wen, Bo Chen, Xi Liu, Jiang-Jiao Zhou,Department of General Surgery, The Second Xiangya Hospital, Central South University,Changsha 410011, Hunan Province, China
Abstract
Key words: Post-hepatectomy liver failure; Hepatocellular carcinoma; Hepatectomy;Model for end-stage liver disease; Standardized future liver remnant; Hepatitis B virus
INTRODUCTION
Hepatocellular carcinoma (HCC) is the world’s sixth highest incidence and death rate third malignant tumor.In the past 10 years, there has been great progress in the treatment of HCC.There are many ways to treat HCC, such as hepatectomy, imageguided transcatheter tumor therapy, liver transplantation, and systemic therapy(drugs such as sorafenib were indicated to improve survival rates in patients with advanced liver cancer)[1-3].However, hepatectomy is still the first-line treatment for primary and secondary liver cancer and non-cirrhotic hepatocellular carcinoma, and the best method for long-term survival[4,5].The widespread use of large-area hepatectomy enhances the danger of post-hepatectomy liver failure (PHLF), which is related to the incidence of complications, mortality, and length of prolonged hospital stay[6].Despite improvements in surgical and postoperative management, the parameters determining the degree of hepatectomy remain largely uncertain.Many preoperative factors, intraoperative factors, and postoperative factors are the causes of PHLF[6].Preoperative evaluation, including the assessment of liver volume and residual liver function, is a prerequisite for major hepatectomy.At present, PHLF remains one of the worst complications in hepatectomy, and it is one of the main causes of death after hepatectomy[7,8].Therefore, accurate preoperative prediction of PHLF risk in patients with liver cancer is key for surgeons to evaluate the feasibility and safety of hepatectomy.
The quality and quantity of hepatocytes determine the liver function reserve.In 2000, Malinchocet al[9]used model for end-stage liver disease (MELD) score to predict the mortality of patients with end-stage liver disease after tranjugular intrahepatic portosystemic shunt, and the authors confirmed that MELD score could predict mortality and survival time in end-stage liver disease.MELD scores are used to prioritize patients most in need of organ transplantation according to objective criteria(creatinine level, international standardized ratio (INR), and bilirubin level)[10,11].However, MELD score can also predict the survival rate of patients with liver cirrhosis caused by infection, variceal bleeding, fulminant liver failure, and alcoholic hepatitis.Moreover, MELD score can also be used to select surgical patients other than liver transplantation patients and to determine the best treatment for HCC patients[12-14].It is reported that MELD score can predict the occurrence and death of PHLF after hepatectomy[13,15].
Standardized future liver remnant (sFLR) volume has been considered to be an important factor affecting the outcome of major hepatectomy[16].In recent years, liver computed tomography (CT) volumetry has been used to evaluate liver function reserve, especially in the selection of patients with HCC for major hepatectomy.Before the operation, the residual volume of the liver is measured by a 3D CT reconstruction method, which can accurately reflect the size of the residual liver.Patients with smaller FLR volumes have a higher risk of PHLF[17].Although MELD score and sFLR volume are two popular markers for evaluating liver function reserve in the clinic, no studies have been performed on the effect of the MELD score and sFLR volume to predict the incidence of PHLF after hepatectomy.
In the past, sFLR volume was used to measure the size of the residual liver[17].Although both measurements can predict the occurrence of PHLF after hepatectomy to a certain extent, the sensitivity and specificity do not sufficiently meet clinical needs; therefore, an urgent issue is the need for a new method to predict the risk of PHLF after hepatectomy in order to better reduce the incidence of PHLF.In view of this, we compared the roles of MELD score, sFLR volume, and sFLR/MELD ratio in predicting PHLF after hepatectomy.
MATERIALS AND METHODS
Patients
Patients who accepted 3D CT reconstruction prior to hepatectomy for HCC from January 2015 to January 2018 at the Second Xiangya Hospital of Central South University were considered for this retrospective study.The inclusion criteria were:(1) HCC was not treated before operation, without cardiopulmonary dysfunction,renal insufficiency, or severe encephalopathy before hepatectomy; (2) Open hepatectomy with curative intent performed by a single team of surgeons; and (3)None of these patients had biliary obstruction prior to surgery or evidence of hepatitis C virus-specific antibodies or alcoholic cirrhosis.
Informed consent was waived for this retrospective research.This research was approved by the Central South University Agency Review Committee.
Methods
To overcome the limitation of MELD score in predicting postoperative prognosis, in recent years, the liver CT volume method has been used to estimate the liver function reserve, especially in selecting patients with HCC for major hepatectomy[18].The FLR volume of the liver was measured by 3D CT reconstruction, and the residual liver size could be truly reflected[19].sFLR volume, calculated as FLR/estimated total liver volume, was used to reflect the percentage of residual liver after resection[20].MELD score is calculated on the basis of INR, serum creatinine (Cre), and the total bilirubin(TBil):MELD = 9.57 × ln (Cre, mg/dL) + 3.78 × ln (TBil, mg/dL) + 11.2 × ln (INR) +6.43 × (etiology:0 if cholestatic or alcoholic, 1 otherwise)[21].A diagnosis of HCC was made according to the postoperative pathological examination.PHLF was accounted as the total bilirubin value was more than 50 μmol/L and the prothrombin time index was less than 50% (INR > 1.7) on or after the 5thd after operation[22,23].
Statistical analysis
Continuous variables are represented as intermediate values (ranges) and compared by the Mann-WhitneyUtest.Univariate analysis and multivariate Logistic regression analysis were used to determine the risk factors related to PHLF.Determination of the cut-off value of PHLF was performed by receiver operating characteristic (ROC) curve analysis.Comparison of discrete variables was performed by theχ2test.Statistical analyses were performed using SPSS 24.0 (IBM, United States).Pvalues < 0.05 were considered statistically significant.
RESULTS
Patient groups and characteristics
In this study, 238 patients were divided into two groups according to whether PHLF occurred after hepatectomy.The median age of PHLF (+) patients was 57 years(range, 26-66 years), and that of PHLF (-) patients was 51 years (range, 18-74 years).Comparisons showed that there was no difference in prothrombin time, age, sex ratio,INR, alanine aminotransferase, HBsAg positivity, maximum tumor size, or major hepatectomy(P> 0.05; Table 1) between the two groups.However, platelet count (P<0.05), total bilirubin level (P< 0.01), albumin level (P< 0.05), sFLR volume (P< 0.001),and MELD score (P< 0.01) were significantly different (Table 1).In China, many patients already have liver cirrhosis and poor liver function during outpatient visits.Of the patients included in the research, the percentage of patients with HBsAg positivity was as high as 90%, and many of the patients with HCC also had liver cirrhosis, which led to the high incidence of PHLF.
Univariable and multivariable analyses to identify predictors of PHLF
Univariate and multivariate analyses were used to determine the risk factors related to PHLF.The correlation between PHLF and the sFLR volume combined with MELD score was analyzed.Univariate logistic regression analysis showed that platelet count,albumin level, MELD score, and sFLR volume were risk factors for PHLF (P< 0.05;Table 2).Multivariate logistic regression analysis revealed that platelet count, albumin level, MELD score, and sFLR volume were independent risk factors for PHLF (P<0.05; Table 2).
Value of sFLR volume, MELD score, and sFLR/MELD score for predicting PHLF
The ROC curve analysis revealed that the area under curve (AUC) of MELD score to predict PHLF was 0.715 (Figure 1), with a 55.0% sensitivity and 83.0% specificity, and the best MELD score cut-off value for the prediction of PHLF was 8.5 (P< 0.01, Table 3).Similarly, the AUC of sFLR volume for predicting PHLF was 0.782 (Figure 1), and the cut-off value was 0.544, with a 77.1% sensitivity and 75.0% specificity(P< 0.001,Table 3).Moreover, the AUC of the sFLR/MELD score for the prediction of PHLF was 0.845 (Figure 1), and the cut-off value was 0.078, with a 66.5% sensitivity and 95.0%specificity (P< 0.001, Table 3).
sFLR/MELD score is a more useful predictor of PHLF in HCC patients following hepatic resection
To validate the sFLR/MELD score, we used the sFLR/MELD ratio as the basis for dividing all patients into two groups.The incidence of PHLF was 13.01% (19/146) in patients with an sFLR/MELD score ≥ 0.078 and 1.09% (1/92) in patients with an sFLR/MELD score < 0.078 (χ2= 9.065,P= 0.001.Table 4).When sFLR/MELD ≥ 0.078,the incidence of PHLF was much higher than that in patients with an sFLR/MELD <0.078.The regression coefficients of the sFLR/MELD score were statistically significant.Therefore, 0.078 can be used as the favorable cut-off value to predict PHLF based on sFLR/MELD.Finally, our data showed that sFLR/MELD score, as a good indicator of PHLF, can predict PHLF better than MELD score or sFLR volume alone.
DISCUSSION
In this research, we evaluated the value of MELD score, sFLR volume, and their combination to predict the occurrence of PHLF after hepatectomy.Although both MELD score and sFLR volume can predict the occurrence of PHLF to some extent, we found that their combination could improve the accuracy, sensitivity, and specificity for predicting PHLF.Thus, this combination score has good guiding significance in the clinic.
For years, hepatectomy has remained one of the most complex surgical procedures.The mortality rate after hepatectomy ranges from 0 to 5%[24], while PHLF remains the main cause of high mortality after hepatectomy[25].PHLF refers to the failure of one or more synthetic and excretory functions, including hyperbilirubinemia, prolonged prothrombin time, hypoalbuminemia, elevated serum lactate, and different grades of hepatic encephalopathy[25-27].Although the incidences of both PHLF and mortality have improved considerably over the past 10 years as a result of improvements in surgical techniques and critical care, the incidence of PHLF is still 8% to 10%[25,28].However, the incidence of PHLF can be as low as 1% to 2% in some countries[29].This outcome may be associated with a low incidence of HBV infection and liver cirrhosis[29].Therefore, it is of great clinical significance to evaluate the risk for PHLF before surgery to reduce the incidence of PHLF after hepatectomy.
MELD score is commonly used as an objective criterion for evaluating the severity of end-stage liver disease and has also been applied in the treatment of patients with chronic liver disease without transplantation[30].Additionally, MELD score has also been indicated to have the ability to predict PHLF and mortality following hepatic resection in HCC[13,15].According to multivariate analysis in this study, MELD score is an independent predictor of PHLF after hepatectomy.However, in some other studies, MELD score was not a significant predictor of PHLF[10,31].To the best of our knowledge, MELD score is frequently used in patients with advanced cirrhosis[10]who are often not eligible for hepatic resection because of poor liver function reserve.It seems that MELD score exhibits low value in predicting postoperative liver function in HCC patients with no chronic liver diseases or cirrhosis[32].In China, most HCCpatients have a background of HBV infection with liver function impairment[33].It was found in our study that 92.4% of the patients had HBV infection.This might be one of the reasons that we obtained a relatively high rate of PHLF (8.4%).In addition, the AUC of the MELD score for prediction of PHLF was 0.715 (P< 0.01), showing a relatively good predictive performance.This finding may indicate that MELD score has good predictive value in HCC patients with chronic liver diseases.
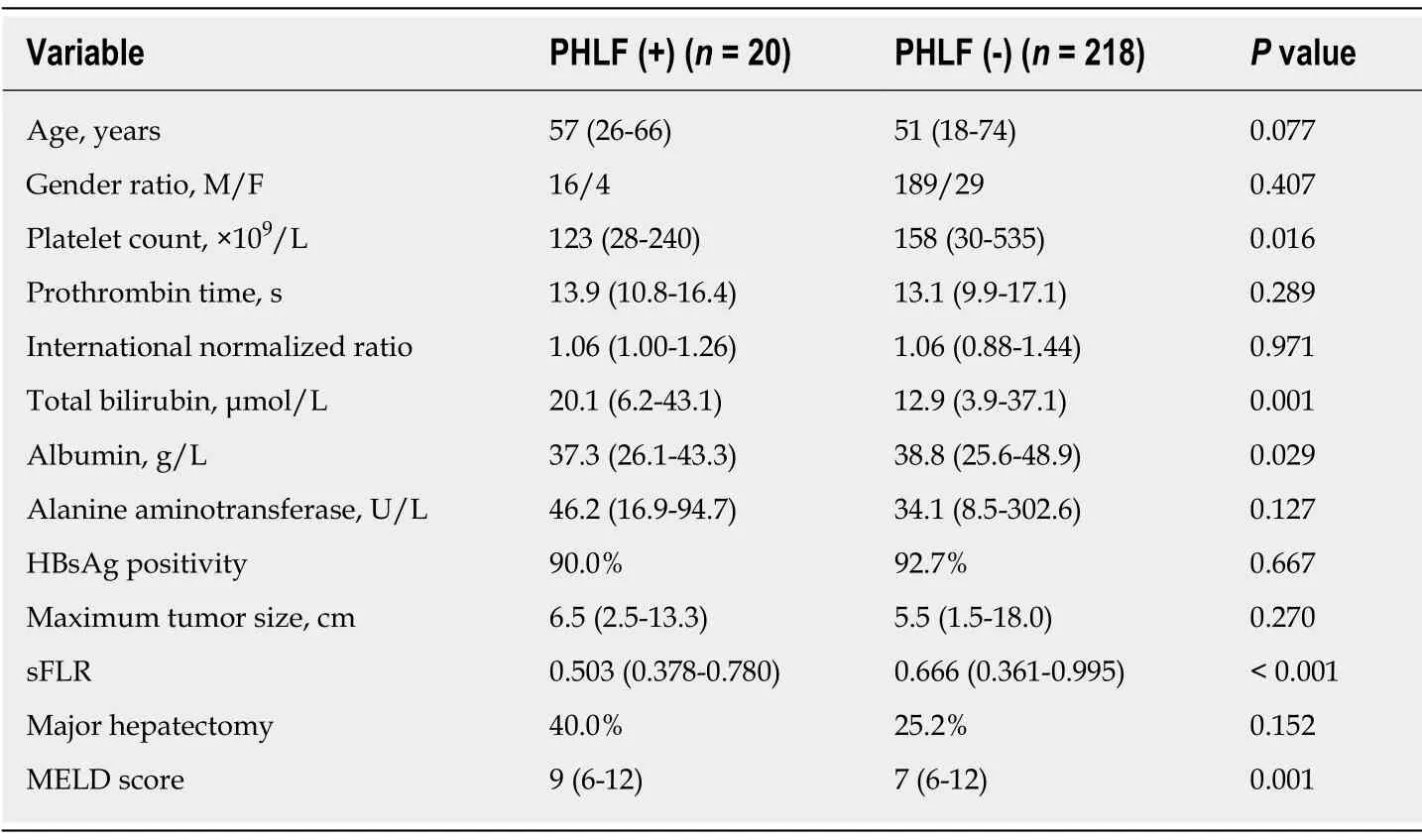
Table 1 Patient characteristics in the two groups
In addition, we also found that platelet count, albumin level, and sFLR volume were independent risk factors for PHLF.It is interesting that in our previous study,albumin level, bilirubin level, and sFLR volume were also significant predictors of PHLF, and their combination was more effective in predicting PHLF after hepatectomy[2].Given this finding and to improve the predictive value, we combined MELD score with sFLR volume to develop a new model.ROC curve analysis showed that sFLR/MELD score had a larger AUC in predicting PHLF than sFLR volume or MELD score alone.This result demonstrated that the combination of MELD score and sFLR volume could gain a better predictive performance for PHLF.Patients with an sFLR/MELD score ≥ 0.078 had a significantly higher incidence of PHLF than those with an sFLR/MELD score < 0.078 (13.01%vs1.09%).Therefore, patients with an sFLR/MELD score ≥ 0.078 are at a high risk of developing PHLF, and prompt clinical intervention is needed for these patients in order to reduce postoperative complications and PHLF.
The current research still has some limitations.First, all patients in the study came from a single research center, and selective bias may be exhibited.In addition, the number of patients in this study was low, so there is a need to recruit more patients from more research centers in future studies.Furthermore, as some patients did not undergo CT scanning at our hospital, three-dimensional CT reconstruction was not available for those patients.Therefore, the patients were not included.Finally,because of the short follow-up time, it was impossible to analyze the relationship between the sFLR/MELD score and patient survival, which is needed in the future.
In conclusion, sFLR volume combined with MELD score is a reliable and effective predictor to predict PHLF after hepatectomy.This measurement can effectively guide the early management after hepatectomy, improve the prognosis, and reduce the mortality.This tool also provides a new strategy for preoperative evaluation of hepatectomy.

Table 2 Univariable and multivariable analyses to identify predictors of post-hepatectomy liver failure
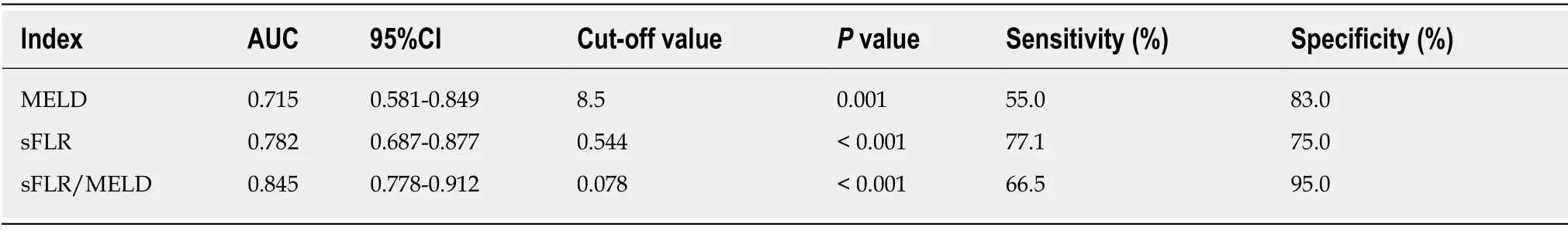
Table 3 Prognostic value of various indexes to predict post-hepatectomy liver failure
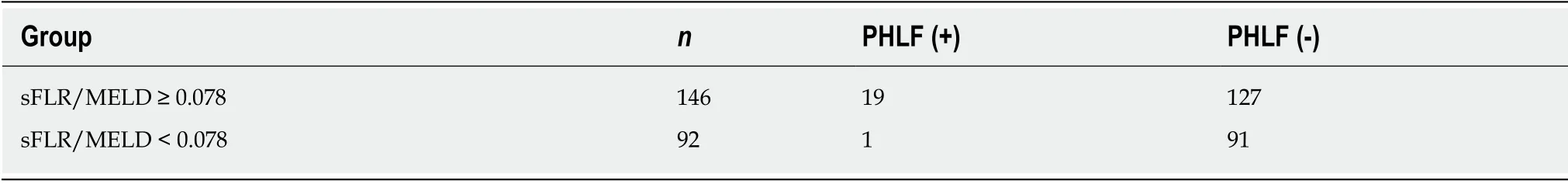
Table 4 Comparison of post-hepatectomy liver failure based on the cut-off value of standardized future liver remnant /model for endstage liver disease
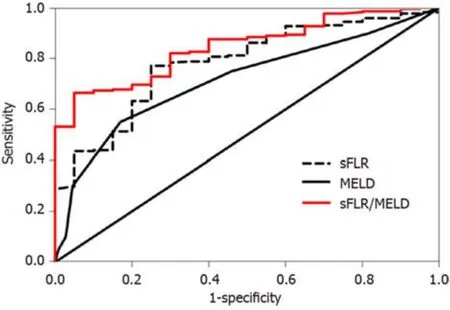
Figure 1 Receiver operating characteristic curve analysis of standardized future liver remnant volume, model for end-stage liver disease score, and standardized future liver remnant /model for end-stage liver disease score for predicting post-hepatectomy liver failure.
ARTICLE HIGHLIGHTS
Research background
Hepatocellular carcinoma (HCC) is the most frequent primary liver cancer.HCC predominantly develops in patients with liver cirrhosis.At present, hepatectomy is still the main treatment for HCC.However, post-hepatectomy liver failure (PHLF) is one of the most serious complications following hepatic resection, despite improvements in surgical and post-operative management.Thus, it is of great clinical significance to evaluate the risk of PHLF before operation to reduce its incidence after hepatectomy.
Research motivation
At present, the models of predicting the occurrence of PHLF after hepatectomy do not meet the clinical needs.We need to have new forecasting indicators to further improve the models for predicting the occurrence of PHLF.The purpose of our study was to evaluate the value of model for end-stage liver disease (MELD) score combined with standardized future liver remnant(sFLR) volume in predicting PHLF in patients undergoing hepatectomy for liver cancer.
Research objectives
To study the value of MELD score combined with sFLR volume in predicting PHLF in patients undergoing hepatectomy for HCC, and explore the application of sFLR/MELD score in the hepatectomy and treatment of HCC, so as to provide reference for clinical treatment of this malignancy.
Research methods
A total of 238 patients with HCC treated at our hospital from January 2015 to January 2018 were selected as a study group.Discrimination of sFLR volume, MELD score, and sFLR/MELD ratio to predict PHLF was evaluated according to the univariable and multivariable analyses,χ2test,and receiver operating characteristic curve analysis.
Research results
The incidence of PHLF increased with the decrease of sFLR volume and the increase of MELD score.Moreover, both sFLR volume and MELD score were independent risk factors for PHLF.The cut-off value of the sFLR/MELD score to predict PHLF was 0.078, with an AUC of 0.845,which was superior to MELD score or sFLR volume alone.
Research conclusions
sFLR volume combined with MELD score can effectively guide early treatment after hepatectomy, so as to improve prognosis and reduce mortality.The model also provides a new strategy for preoperative evaluation of hepatectomy.
Research perspectives
Future studies are needed to further confirm the relationship between sFLR/MELD score and patient survival rate so that it can be better used in clinical practice.What’s more, to further consummate the follow-up time of patients and improve the accuracy of sFLR/MELD score is the next step for further analysis.
 World Journal of Clinical Cases2019年22期
World Journal of Clinical Cases2019年22期
- World Journal of Clinical Cases的其它文章
- Colorectal cancer:The epigenetic role of microbiome
- Human podocyte injury in the early course of hypertensive renal injury
- Relationship between acute hypercarbia and hyperkalaemia during surgery
- Surgical treatment ofpatients with severe non-flail chest rib fractures
- Super-selective arterial embolization in the control of acute lower gastrointestinal hemorrhage
- Treatment of hemorrhoids:A survey of surgical practice in Australia and New Zealand
