Quality evaluation and content analysis of non-drug guidelines on risk factors of secondary prevention of myocardial infarction
Wen-Jiao Li,Meng-Zhu Zhao,Chang Rao,Xue-Chao Liu,Qi Liu,Chang-De Jin*,Yan Li*
1Graduate College,Tianjin University of Traditional Chinese Medicine,Tianjin,China.2First Teaching Hospital of Tianjin University of Traditional Chinese Medicine.3School of Nursing,Tianjin University of Traditional Chinese Medicine,Tianjin,China.
Abstract
Keywords: Myocardial infarction,Guideline,Quality evaluation,Appraisal of Guidelines for Research and Evaluation II,Secondary prevention
Introduction
Myocardial infarction (MI) is a chronic lifelong disease,and patients are often in a long-term disease state [1].Patients who have been diagnosed with MI have a high risk of developing cardiovascular events [2].After the first MI,survivors are still at increased risk of subsequent cardiovascular events,such as death,heart failure,recurrent myocardial infarction,arrhythmia,angina,and stroke[3].Traditional risk factors for MI include smoking,obesity,hypertension,dyslipidemia,diabetes,etc.,which are mostly intervention factors [4].Among them,hypertension,dyslipidemia and diabetes are risk factors for heart failure after MI,recurrent cerebral infarction and recurrent myocardial infarction after percutaneous coronary intervention [5-7].Therefore,it is particularly important to control and monitor the risk factors in the secondary prevention of patients with MI.However,related studies have shown that the relatively awareness about risk factors is low for secondary prevention in patients with MI [8],and the compliance rate is also low[9].Therefore,this study will systematically search for the risk factors and the non-drug guidelines related to risk factors in secondary prevention of MI by conducting strict quality evaluation of relevant recommendations.In recent years,non-drug therapy associated with MI produced a large number of researches,developing the guidelines of management and rehabilitation of MI.However,the methodological quality of these guidelines is unknown,and there are still barriers from researches to clinical practice.The wrong guidelines may cause a waste of medical resources,and even bring harm to patients.Thus,we use the international recognized evaluation tool to evaluate the quality of the relevant practice guidelines,including scope and purpose,stakeholder involvement,rigor of development,clarity of presentation,applicability and editorial independence dimensions,in order to provide reference for the non-drug care of patients with MI.
Materials and methods
Identification of guidelines
Guideline sources: (1) clinical practice guideline website:Guideline International Network,National Institute for Health and Clinical Excellence (NICE),Scottish Intercollegiate Guidelines Network,National Guideline Clearinghouse,World Health Organization,Australian Clinical Practice Guidelines,New Zealand Guidelines Group; (2) databases: PubMed,CNKI,WanFang,VIP; (3)references list.
Search strategy: the search strategy was based on the research team's expertise and combined with a medical librarian.PubMed were searched with MeSH terms and free words.The search terms were as follows:(myocardial infarction or AMI or heart infarction) and (acute coronary syndrome or ACS) and (coronary heart disease or CHD)and (STEMI or NSTEMI) and (practice guideline or guideline)and(risk factor or blood pressure or blood sugar or blood lipids).Chinese databases also were searched with the title,abstract,topic or full-text search.Professional guide websites were searched for the above search terms based on their respective search methods.
Literature screening
Inclusion criteria: (1) guidelines or expert consensus on secondary prevention of myocardial infarction or the recommendations of guidelines related to risk factors for myocardial infarction; (2) guidelines published or updated between January 1,2013 and March 31,2019;(3)the latest version was included,if there are multiple versions of the guideline; (4) full-text of guideline is available in English or Chinese.
Exclusion criteria: (1) guideline does not cover the risk factors for secondary prevention of MI; (2) drug-related guidelines;(3)repeated published guidelines or consensus;(4) interpretation of guidelines and consensus; (5) the Chinese translation of foreign guidelines; (6) the full-text guideline is not available.
The screening of the literature was carried out by two researchers with title,abstract,and the full-text back-to-back according to the inclusion and exclusion criteria.After the initial screening,cross-checking was carried out.All disagreements and uncertainties regarding eligibility were resolved through discussion and a third reviewer was consulted.
Methodological quality assessment of the guideline
The Appraisal of Guidelines for Research and Evaluation II(AGREE II) is one of the most widely used tools for the evaluation of methodological quality of guidelines[10,11].It consists of six dimensions including scope and purpose,stakeholder involvement,rigor of development,clarity of presentation,applicability and editorial independence,a total of 23 items and 2 items of overall guideline assessment [12].Four trained and qualified researchers independently evaluate the methodological quality of the included guideline using AGREE II.The standardized scores were calculated in each field with four researchers and,the recommended level was classified as:A for overall scores >60%,B for scores ≥30%at least in three fields,C for scores <30%at least in three fields.
Extraction,translation and summary of the guideline
Self-designed general data extraction sheet for included guidelines was performed,including guideline ID,publication time,country,guideline type,topic and the number of references.
The extraction,translation and summary of the literatures were carried out separately and independently by two researchers in the research team.After completion,cross-checking was carried out.All disagreements were checked with other members of the research team to ensure the integrity of the extracted content and the translation of related content.
Statistical methods
The consistency of the evaluator's evaluation results was tested by calculating the intra-correlation coefficient(ICC)to measure the reliability between the evaluators with SPSS:for Version 22.0.It is generally considered that ICC≥ 0.75 indicates the internal consistency between the evaluators higher[13].
Results
Guideline characteristics
A total of 2,099 articles were obtained in the initial examination,of which 1,991 were obtained through database search,108 were retrieved from each guideline website,and 6 were traced back to the reference.According to the inclusion and exclusion criteria,8 guides were finally included [14-21].The specific literature screening process is shown in Figure 1.
Among the 8 included guidelines,one was from the United States [14],two were from the United Kingdom[15,16],five were from China [17-21],and five were evidence-based guidelines [14-17,20],three were expert consensus [18,19,21].General information for include guideline is shown in Table 1.list)
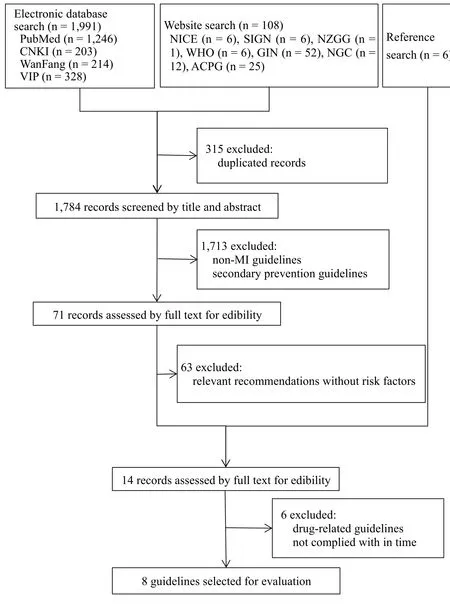
Figure 1 Study flow diagram.
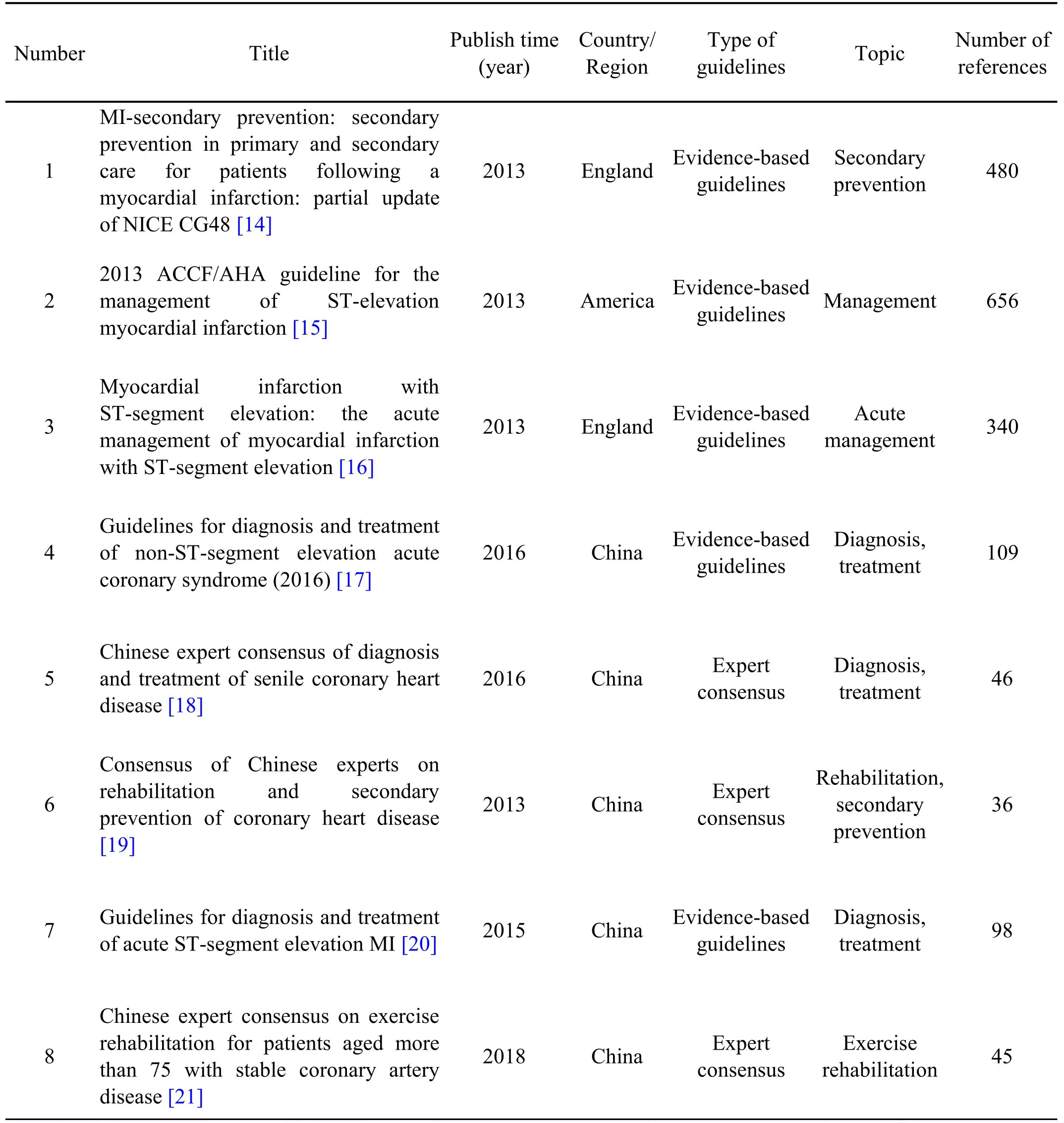
Table 1 Characteristics of included guidelines
Consistency
The ICC value of the four guideline evaluators was 0.817 in the review,and the consistency among the evaluators was better.
Quality evaluation of the guidelines
The methodological quality of the included guideline was rigorously evaluated by AGREE II,and the average standardized scores in scope and purpose,stakeholder involvement,rigour of development,clarity and presentation,applicability,and editorial independence were 74.65%,47.66%,40.56%,68.40%,33.99% and 31.51% respectively.The quality of one guideline was grade A,four guidelines were grade B,and three were C.Among them,the guidelines issued by the American Heart Association (AHA) and the American College of Cardiology Foundation scored >60% in all areas.The two guidelines from the National Institute of Health and Clinical Excellence (NICE) have high scores in the terms of scope and purpose,stakeholder involvement,the rigor of development,and clarity and presentation.Overall,the 8 included guidelines have lower average scores in the areas of applicability and editorial independence.The scores for each area of the specific guidelines are shown in Table 2.
Analysis of guidelines
This study summarized 24 recommendations for blood pressure,blood glucose,and blood lipid risk factors.The recommendations mainly refer to the target values in different populations,including patients with coronary heart disease (CHD) and ST-segment elevation myocardial infarction (STEMI),non-ST-segment elevation myocardial infarction,acute STEMI patients,elderly ( ≥80 years old) CHD patients,and 75-year-old stable CHD patients,etc.
Blood pressure.The goal of blood pressure for patients with CHD: blood pressure (BP) <130/80 mmHg[19].The goal of blood pressure for patients with acute coronary syndrome (ACS): diastolic blood pressure(DBP)<90 mmHg.The patients with diabetes:DBP<85 mmHg,systolic blood pressure (SBP) <140 mmHg [17].Recommended goal of blood pressure for older CHD patients aged ≥80 years: (1) If the health condition is good: BP <150/90 mmHg [18]; (2)If the patient is weak and the life expectancy is short: personalized treatment.Patients with STEMI should have effective blood pressure management after discharge: BP < 140/90 mmHg (SBP ≥110 mmHg) [20]; antihypertensive drug therapy should be provided to patients with hypertension identified as having cardiovascular disease [14].For people under 80 years with high blood pressure,the target blood pressure is lower than 140/90 mmHg; for those aged 80 years and older,the target blood pressure is lower than 150/90 mmHg[14].
Blood glucose.The goal of glycosylated hemoglobin for patient with coronary heart disease: hemoglobin Alc(HbAlc) ≤7.0% [19].Recommended goal for glycated hemoglobin for patients aged 80 years and older who are generally in good health with CHD: HbAlc ≤8.0% [18].It is recommended that all patients with non-ST-segment elevation acute coronary syndrome to carry out screening on diabetes,and patients with hyperglycemia who are known to have diabetes or who are on admission should be monitored for frequent blood glucose levels [17].Patients with non-ST-segment elevation acute coronary syndrome and hypoglycemic are advised to be actively treated to make HbAlc <7% [17].Patients with STEMI should be tested for fasting blood glucose after stable disease,and oral glucose tolerance test should be performed if necessary [20].Patients whose blood glucose >10 mmol/L with ACS should be treated with hypoglycemic therapy.The goal of blood glucose should be determined in consideration of the patient's comorbidities,and hypoglycemia should be avoided [17].Patients with STEMI and diabetes should be treated with hypoglycemic agents while actively controlling diet and improving lifestyle[20].
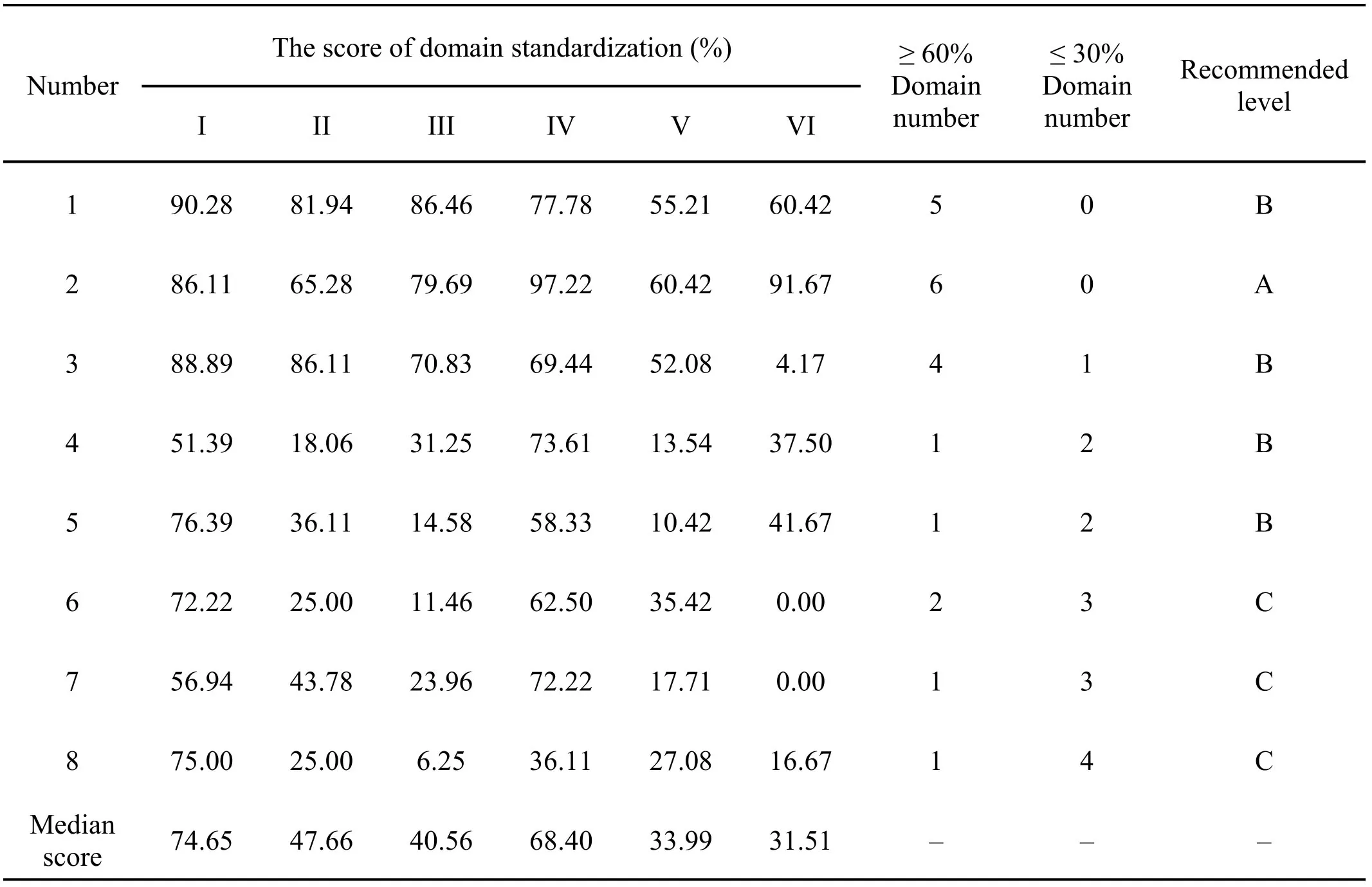
Table 2 The domains score of included guidelines
General principles of glycemic control in diabetic patients: patients with very advanced cardiovascular disease,advanced age,long history of diabetes,and more comorbidities should have more loose glycemic control during the acute phase and follow-up period [17].The general principle of drug treatment in secondary prevention: the more serious the cardiovascular disease,the older the age,the longer the duration of diabetes and the more comorbidities,the stricter the blood sugar control[17].
Patients with STEMI can control HbAlc below 7% if they have better general health status,shorter diabetes history,and younger age [20].Relatively loose HbAlc target goals (eg <8.0%)are more suitable for a history of severe hypoglycemia,shorter life expectancy,significant microvascular or macrovascular complications,or severe comorbidities,long duration of diabetes,oral hypoglycemic agents or insulin patients with difficult blood glucose control after treatment[20].
Treatment of hypoglycemia during exercise: conduct relevant education to inform the emergency treatment of hypoglycemia.The hypoglycemia is related to pre-exercise blood glucose.If blood glucose before exercise is less than 5.6 mmol/L,exercise after eating sugar.In the exercise,patients with hypoglycemia and delayed hypoglycemia should immediately eat food containing 10-15g sugar.After 15 minutes,if the blood glucose is still <3.9 mmol/L,give the same amount of food.Severe hypoglycemia that cannot be corrected after eating should be sent to a medical center for rescue.
Blood lipid.Long-term adherence to lipid-lowering standard treatment is the cornerstone of secondary prevention [17].Blood lipid profiles should be established for all patients.For hospitalized patients,lipid-lowering therapy should be initiated before discharge [15].High-risk CHD patients with dyslipidemia: low density lipoprotein cholesterol(LDL-C) <2.59 mmol/L (100 mg/dL),very high risk patients(patients with ACS/CHD and diabetes):LDL-C <2.07 mmol/L (80 mg/dL); if the triglyceride ≥ 2.26 mmol/L (200 mg/dL),non-high-density lipoprotein cholesterol in high-risk patients high density liptein cholesterol (HDL-C) < 3.37 mmol/L (130 mg/dL),non-HDL-C in very high risk patients <2.59 mmol/L(100 mg/dL) [19].Low-density lipoprotein recommended value for elderly aged CHD patients aged 80 years and older who are in good general condition: <1.8 mmol/L[18].Patients are strongly advised to change their lifestyles,including daily physical activity and sports to regulate lipids [15].It is recommended that patients with high-risk or cardiovascular disease are advised to eat a total fat intake of 30 percent or less of their total energy intake,saturated fat intake accounts for 7%or less of total energy,dietary cholesterol intake is less than 300 mg/dL,and if possible,monounsaturated fat and polyunsaturated fat are used in place of saturated fat[16].
Discussion
In this study,the methodological quality of the included guidelines was evaluated from six fields with AGREE II,and the recommended level of the guidelines was determined in combination with the standardized scores.Finally,a total of 8 guidelines were included,of which only one guide recommended level A,which was issued by AHA and ACCF,two guidelines from NICE with recommended level B.We found that the guidelines from NICE scored poorly in the application field(<60%).And the information for the beneficial or potential disadvantages of the guidelines such as potential related resources was not clear in the implementation process and suggested application,may not fully consider the feasibility and promotion of the guideline in the clinical application in the guideline development process,or the report was not standardized.In addition,the five guidelines were derived from the Chinese Medical Association Cardiovascular Branch,the Chinese Medical Association Geriatrics Branch and other professional medical associations,2 of which were evidence-based guidelines,3 were expert consensus.Three guidelines were recommended level C.We found that several dimensions' scores were relatively low,such as stakeholder involvement,rigor of development,applicability and editorial independence.In some of the guidelines,only the members and their names of the guideline development team were described without other details of institutional information or the role of members in the guideline development team.Most of the guidelines did not describe the willingness of target group,including patients,the public,etc.The two guidelines did not state the statement of interest used in the development of the guideline or the description of the conflict of interest of the members of the guideline development team.Considering the reasons,on the one hand,it may be a methodological reason,limited by the publication of the journal; on the other hand,AGREE II may not be the most appropriate evaluation tool for the expert consensuses [22].Therefore,the overall quality of the included guidelines was moderate,which recommended that guideline developers should further standardize the development of the guideline and pay attention to the guideline reporting process.
The review included a wide range of guidelines covering secondary prevention guidelines for myocardial infarction,acute management guidelines,diagnostic and treatment guidelines,and rehabilitation guidelines.However,there was no targeted guideline for risk factors of secondary prevention of myocardial infarction.At the same time,the majority of guidelines were in the medical field and no guidelines were found in the field of nursing.In risk-related recommendations,the included guidelines mostly referred to the target values of blood pressure,blood sugar or blood lipids,and did not further refine the practical recommendations for non-drug control,such as how to control or improve the values of blood pressure,blood sugar and blood lipid through non-drugs,how patients conduct self-monitoring,etc.There were certain limitations in recommendations for the guiding significance of clinical practice.Therefore,basic research should be further implemented and explored on the prevention and improvement of secondary prevention risk factors in patients with myocardial infarction and lay the foundation of the development of guidelines related to targeted risk factors.
Guideline developers should also pay attention to the relevant evidence of traditional Chinese medicine on non-drug to the develop non-drug clinical practice guidelines with characteristics of traditional Chinese medicine.Non-drug interventions include good living lifestyles,healthy eating habits,physical activity,and so on.Studies have shown that myocardial infarction can be prevented and controlled by improving lifestyle and adjusting diet [23].As an important part of secondary prevention of myocardial infarction,healthy lifestyles can effectively reduce the risk of myocardial infarction,improve the prognosis,and determine the quality of life.Cardiac rehabilitation has been recommended in several guidelines,such as MI-secondary prevention from NICE,whose ultimate goal was to control the risk factors of coronary heart disease by improving lifestyle,slow down the progress of the disease,so as to achieve the goal of reducing morbidity and mortality and reversing atherosclerosis [24].It was recommend starting cardiac rehabilitation as soon as possible after admission and before discharge,and about 30 minutes of physical exercise every day,gradually increase the amount of activity,and increase the duration and intensity of activity.As the only country in the world that develops both western medicine and traditional Chinese medicine,traditional medicine occupies an important position in its entire medical system,such as in secondary prevention of myocardial infarction [25].Exercise rehabilitation of traditional Chinese medicine,such as Tai Chi and Baduanjin exercise,can improve emotional management and their sleep quality [26].At present,there was no clinical practice guideline for secondary prevention with the characteristics of traditional Chinese medicine.Therefore,it is suggested that guideline developers attach importance to the positive role of traditional medicine and alternative medicine in secondary prevention of myocardial infarction,fully explore high-quality evidence based on traditional Chinese medicine in secondary prevention of myocardial infarction to formulate clinical practice guidelines to meet the local community with the principles and methods of the international guidelines.
Conclusion
In summary,the overall quality of the eight guidelines included in this study is moderate.The rigor of development,applicability and editorial independence both need to be further standardized.For self-monitoring of patients' risk factors and professionals for patients'health education,the recommended values extracted from the guidelines have certain guiding significance.But targeted interventions for risk factors need to be further explored in clinical research.Practice based on best-evidence and individualized care plans can ensure to improve the quality of care and achieve patient-centered care.
- TMR Non-Drug Therapy的其它文章
- Hidden in the hands-the special inner Bagua acupoints for pediatric massage
- Non-drug therapies for acute gouty arthritis treatment
- The impact of inspiratory muscle training on exercise capacity and inspiratory muscle strength in heart failure patients: a meta-analysis
- Mirror therapy:a potential rehabilitation treatment
- Mirror therapy,an important but underappreciated rehabilitation treatment