Improving patient satisfaction through improved telephone triage in a primary care practice
Rebecca Vitale, Samantha Smith, Benjamin R Doolittle
ABSTRACT Objective The objective of this study was to improve the telephone communication experience for patients in a primary care practice.Design An exploratory survey was conducted that revealed suboptimal patient satisfaction with clinic access due to the telephone triage system. Several interventions were designed: a monthly quality meeting was established among clinic staff, all phone interactions were recorded in the electronic medical record (EMR) and clinic appointments were made available several months in advance. A follow- up survey was conducted to evaluate these interventions.Setting The study was conducted in a multispecialty,urban- based, resident- faculty practice from November 2016 to November 2017.Participants Subjects were recruited in a convenience sample from the waiting room. 200 subjects participated in the initial survey and 215 in the second survey.Results After the interventions, patients felt that their questions were answered more frequently than before(p<0.01). They also felt that appointments were easier to make (p=0.03). A similar number of patients reported seeking emergency care because they were unable to reach a provider (33.8% vs 31.9%, p=0.68). The percentage of patients who received a call back within 24 hours increased, but it was not statistically significant(38.6% vs 44%, p=0.13).Conclusion Improving telephone triage through implementing a monthly quality improvement meeting,optimising use of the EMR and opening schedules several months in advance resulted in several improvements in the patient experience, but did not change use of emergency services. Further interventions, including increased resource allocation, are needed to optimise patient experience.
Key points
INTRODUCTION
Telephone communication with patients is a key component of any outpatient medical practice. Patients depend on reaching clinic staff by phone to schedule appointments,obtain test results, ask questions about medi—cations or symptoms and request medica—tion refills. The quality of a practice's phone system has an important impact in overall quality and access to care. A systematic review by McLeanet alrevealed that up to 50% of patient concerns may be handled by tele—phone advice alone.1Another study by Staceyet alshowed that appropriate telephone triage has been shown to improve patient satisfac—tion and reduce costs.2However, the data on reducing emergency department visits with improved telephone access are equivocal.3A study by Vedsted and Olesen did show that the implementation of a telephone triage system reduced the number of visits by ‘frequent attenders' to after— hours appointments at an outpatient family practice office, but this study did not extend to independent urgent cares or emergency departments.4
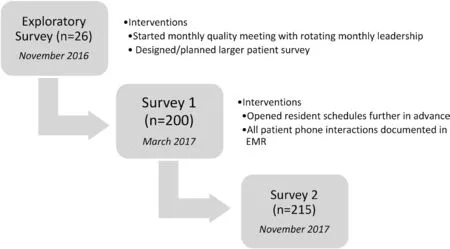
Figure 1 PDSA cycles. PDSA, plan, do, study, act.
Quality improvement projects in the outpa—tient setting are often difficult to implement and sustain. Successful quality improvement projects usually have buy— in among stake—holders as well as support from upper manage—ment.5A well— functioning team with mutual respect and an understanding of one another's strengths and weaknesses is more likely to be successful than one without such qualities.6A strong leader of quality improve—ment projects who engages in top— down planning, rather than strategising with those individuals most affected by the issue that is being addressed, is less likely to be successful.7These issues are particularly challenging in low— resource settings. Also, while there are many quality improvement curricula among residency training programme, there are very little data that show sustained clinical efficacy. One comprehensive review only identified five articles which linked patient outcomes with quality improvement projects that had resident participation.8
This project was designed as a quality improvement effort to improve patient satisfaction and decrease emer—gency department use by improving telephone access and triage in a multispecialty resident— faculty practice based in a community hospital that serves an urban, multi— ethnic community.
METHODS
The study was conducted in a clinic setting that houses three separate practices: an internal medicine resident clinic, an internal medicine— paediatrics resident and faculty clinic, and an obstetrics— gynaecology clinic staffed by midlevel practitioners. The clinic serves a multiethnic community mostly insured through state— sponsored programme. The clinics share a clerical staff that consists of eight individuals. Each clinic has its own nursing staff.There are five medical assistants who are assigned to a single clinic but occasionally rotate between the clinics.There is a single phone number to reach the front desk of all of the clinics, and patient phone calls are directed to the appropriate clinic's staff if there are medical questions or concerns. To refine our challenges further, an explor—atory small— scale patient satisfaction survey (n=26) within the clinic in November 2016 revealed that patient satis—faction with their clinician was generally high but patients were dissatisfied with their interactions with the clinic by phone. Based on this feedback, our quality work focused on optimising the telephone triage system. In particular,our measurements included (1) if patients felt their ques—tions were answered more frequently than prior, (2) if patients felt that appointments were easier to make than prior, (3) if questions were answered in <24 hours and (4)if these interventions resulted in decreased use of emer—gency services.
Further investigation into clinic workflow regarding patient telephone calls was performed as part of a quality improvement initiative in December 2016 to February 2017 (figure 1). These investigations included mapping phone call transfer patterns, shadowing operators using a training headset to understand operator workflow and soliciting direct input from doctors and clinic staff. Inves—tigators learnt that the clinic has a live telephone system staffed by two bilingual (English/Spanish speaking)operators during business hours only. After an initial triage process, calls were transferred to other clinic staff as appropriate. Additionally, operators did most of the appointment scheduling, which was helpful for the work—flow of other staff at the clinic check— in and check— out desks, but led to a long queue of patient callers who had to wait before reaching an operator.
Following the initial data gathering stage, the main challenges of the phone system were determined. The largest part of delay for patients calling the clinic was the wait time before speaking with an operator, and there were often large queues of patients (>10) waiting to speak with an operator. There was a high volume of incoming calls with one call every 2 min and 40 s during the time observed. The operator time was often spent scheduling appointments. The information from patients who left voicemails was recorded in composition books rather than in the electronic medical record (EMR).
To better characterise the patient experience and provide a baseline, a more comprehensive patient satis—faction survey was administered in English and Spanish(n=200) in March 2017. Assuming an effect size of 0.3,alpha of 0.05, and a power of 0.80, a total sample size of 290 participants were needed (145 in each group).9
The front desk clerical staff handed the satisfaction survey to the patients while were waiting for their appointments.Patients were asked via Likert scale about their experiences leaving messages for clinic staff, and whether they got their question answered when they called. They were also queried about ease of making appointments and whether they were treated with respect. Finally, they were asked if they had gone to an urgent care or emergency room because they were unable to get in touch with a provider at the clinic. No personal information was gathered as part of the survey in order to preserve anonymity, so it is unknown if any of these patients had participated in the exploratory survey.
From these data as well as the clinic workflow eval—uation, a three— pronged intervention was developed:monthly quality and safety lunchtime meetings were initi—ated for the clinic staff, resident clinic schedules were‘opened up' further in advance to allow more appoint—ments to be scheduled before patients left the clinic and all voicemail messages were required to be entered into the EMR. These interventions were chosen because they were hypothesised to improve the focus on quality and safety in the clinic, reduce the call volume to reduce the strain on call operators and the queue of waiting patients and increase the likelihood that the patient's question would reach the appropriate person.
The design of the monthly quality and patient safety meetings had a unique feature: rotating monthly lead—ership. Clerical staff, medical assistants and nurses were encouraged to lead the meeting, share their perspectives and design solutions to concerns. The meetings were well—attended and staff members had significant pride in the shared achievements. The inclusion of all clerical staff,whose voices are not often heard in quality initiatives, engen—dered buy— in and ownership of the changes that were made from the meeting. This disrupted the traditional top— down management approach of many operational meetings.
A follow— up survey patient satisfaction survey was adminis—tered 1 year after the initial exploratory survey in November 2017, and ~6 months after the interventions were deployed.The survey included all questions from the baseline survey(n=215). The differences between responses between the two surveys were analysed using either Student's t— test or χ2test, depending on the number of possible responses. Statis—tical analyses were conducted using SAS V.9.4. The project was reviewed by the Yale Institutional Review Board and was granted an exemption.
RESULTS
The initial survey was administered to 200 patients; the follow— up survey was administered to 215 patients after implementation of the three— pronged intervention,which included monthly quality and safety meetings with the clinic staff, opening resident schedules up earlier in advance and requiring all phone call interactions to be documented in the EMR. Demographic information was not collected from the subjects in order to preserve anonymity; and it is unknown if the same subjects were surveyed at the different time points. As shown in table 1 and figure 2, after the interventions were implemented,patients felt that their questions were answered more frequently than prior (79.9% often or always after vs 67.4% prior, p<0.01). Patients also felt that they were more frequently treated with respect after the interven—tion (94.8% often or always after vs 89.4% prior, p=0.01)and that it was easier to make an appointment (75.8%often or always after vs 69% prior, p=0.03). There was no significant change in patients reporting urgent care or emergency department visits (33.8% before vs 31.9%after, p=0.68). Similar numbers of patients left a message for the clinic staff if they were unable to speak with a staff member directly (42.3% often or always after vs 42.4%prior, p=0.70). The percentage of patients who received a call back within 24 hours increased, but it was not statisti—cally significant (38.6% often or always after vs 44% prior,p=0.13). Post hoc power analysis, with an effect size of 0.3,alpha of 0.05, and a total sample size of 415 participants(n1=200, n2=215), the study was powered at 0.92.9
DISCUSSION
The challenges with telephone communication faced in our clinic are common among urban primary care settings, including a high— needs patient population,frequent staff turnover, limited financial resources and the inherent challenges of provider continuity related to a resident clinic. It is important for staff members, partic—ularly physicians, to understand how their phone triage systems work as telephone communication is a critical part of any outpatient clinic.
This study was initiated in response to survey data suggesting that patients were not satisfied with many aspects of their telephone interactions with the FHC clinic. In complex health systems, even simple daily processes involve multiple stakeholders and are impacted by electronic systems and specific patient factors. Iden—tifying appropriate metrics—such as ease of making an appointment—was critical for designing effective inter—ventions. Improving patient care is a noble venture. But where to begin? Our specific interventions were designed to impact discrete, measurable variables. After the initial planning period, three simple interventions were imple—mented: monthly quality and safety meetings, opening up resident schedules further in advance and entering all voicemail messages in the EMR. With these interventions,there were significant improvements in the proportion of patients who felt that their questions were answered and patients found it easier to make an appointment. These interventions were successful because they standardised clerical staff workflow without significantly increasing the workload of the staff members.
In addition to this standardisation, the intervention created a new culture of patient safety and quality within the clinic. Staff members have been thoughtful about ways to improve clinic outcomes and patient satisfaction beyond telephone communication, which shows promise for posi—tive impact beyond the initial goals of this intervention.Following the evaluation of these data, a quality and safety meeting was held that focused on the results of the interven—tions, both intended and unintended. The data on patient satisfaction were reported, and the staff members were also given an opportunity to discuss any unintended negative consequences of the changes that they had noticed.
Indeed, teams involved in quality improvement are more likely to be successful if individuals understand one another's strengths and weaknesses, express opinions freely and have mutual respect.6Our intervention incor—porated those principles and suggests that this structure may lead to success in future projects. There are little data regarding the success of quality improvement— focused projects with resident involvement,8and this study is rela—tively unique as an example of a successful resident— driven quality improvement intervention. The small setting and collegial workplace culture was a strength to effective implementation of these quality initiatives.
There are some limitations to this study which must be considered. While the survey was offered in both English and Spanish, the clinic serves a population speakingmultiple other languages. The experiences of patients speaking other languages may differ significantly from the English— speaking and Spanish— speaking patients, and this is an important experience to capture in future studies.The data collection was limited by the capabilities of the clinic's telephone system, which does not have the ability to track duration or volume of patient phone calls. These more objective data could have been very helpful in evalu—ating the impact of the interventions. Finally, the clinic has limited resources and funding to make changes in techno—logical factors that may contribute to the patient experi—ence with our telephone system, which limited the scope of interventions for this problem. Finally, the interventions we designed responded to the particular challenges our clinic faced, based on patients feedback and staff deliberation. It is unclear if these particular interventions could be gener—alisable to other settings. Yet, we believe the method of the team meeting is an efficient strategy for other clinics to generate their own particular solutions to vexing adminis—trative challenges, especially as it includes empowerment of the clerical staff with rotating leadership.
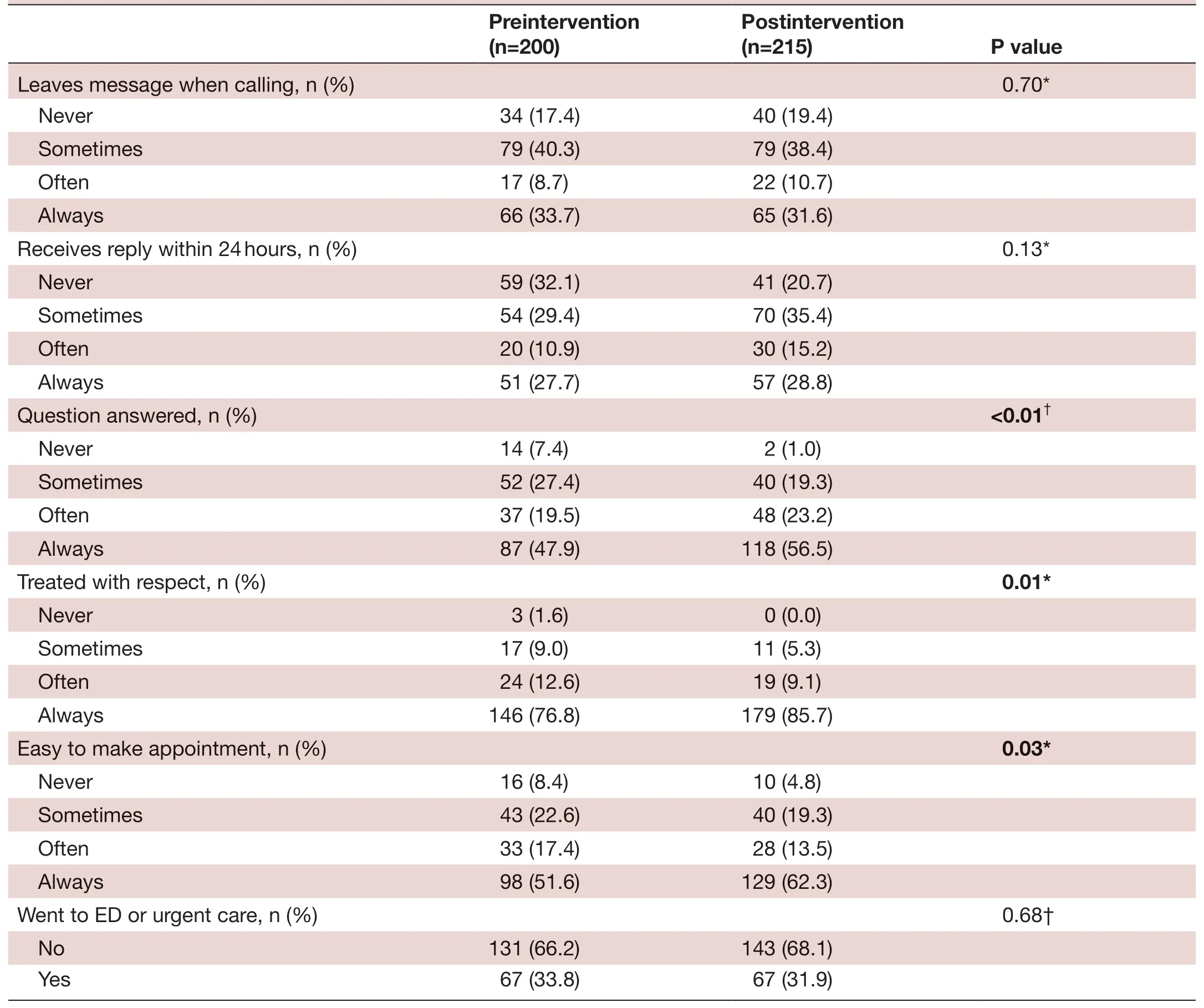
TabIe 1 Results of survey
While optimising the telephone triage system is important for the patient experience, other studies have revealed the need for improved resources. Enhancing mid— level providers or nurse triage lines show promise to increase access to resources and medical advice.4However,intervention studies tend to be small and applied only to a particular clinical context. Results have been equivocal regarding patient satisfaction and reduced emergency room care.1Nursing— driven communication models have been proposed as a means to reduce ER visits and improve patient satisfaction; however, the studies have been eqivocal.1011Although equivocal, these studies suggest that support staff can play a key role in improving tele—phone access for populations of psychosocial complexity in resource— limited settings. Such a system merits further exploration. In the absence of increased personnel, even implementing a telephone system with an electronic menu and touch— tone options to get to the appropriate department could reduce staff workload significantly.
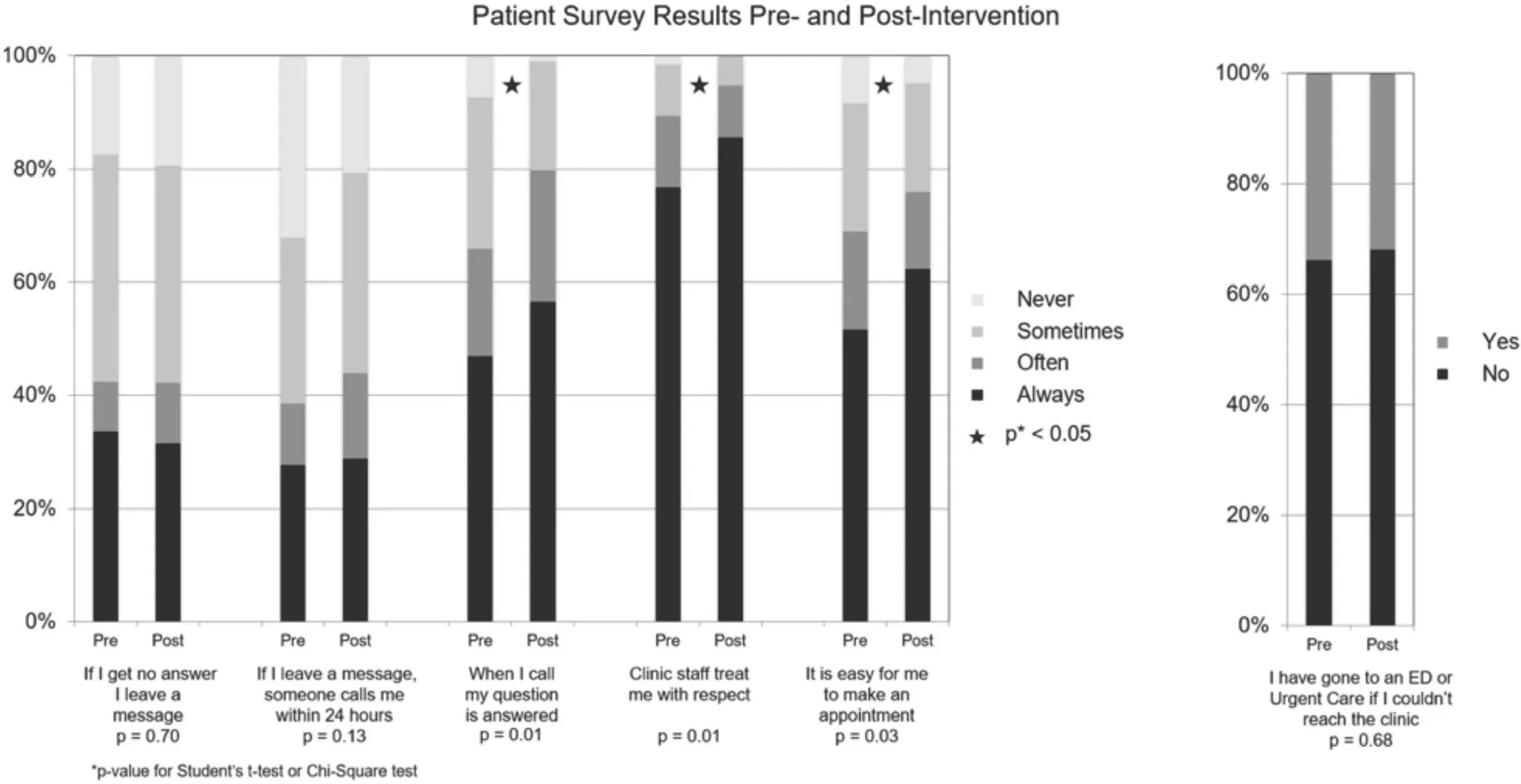
Figure 2 Patient survey results preintervention and postintervention.
CONCLUSION
While increased staffing would be ideal, our project demonstrates that a collaborative project which focuses on allowing input from all involved stakeholders was able to achieve significant improvements. Importantly,we believe the monthly quality meeting with input and rotating leadership by all staff members, as well as opening clinical dates further in advance and documenting phone interactions are effective processes that are likely general—isable across clinical settings.
Contributors RV, SS and BRD all participated in the design and implementation of the study, review and analysis of the data, and writing of the manuscript.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not- for- profit sectors.
Competing interests None declared.
Patient consent for publication Not required.
Provenance and peer review Not commissioned; externally peer reviewed.
Data availability statement Data are available upon reasonable request. All data relevant to the study are included in the article or uploaded as supplementary information.
Open access This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY- NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non- commercially,and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non- commercial. See: http:// creativecommons. org/ licenses/ by- nc/ 4. 0/.
ORCID iD
Benjamin R Doolittle http:// orcid. org/ 0000- 0002- 6922- 6556
 Family Medicine and Community Health2019年4期
Family Medicine and Community Health2019年4期
- Family Medicine and Community Health的其它文章
- From potential to practice: how accelerating access to HPV tests and screen and treat programmes can help eliminate cervical cancer
- Care and social support from family and community in patients with pulmonary tuberculosis in Pakistan
- How French general practitioners adapt their care to patients with social difficulties?
- Factors for self- assessment score of interprofessional team collaboration in community hospitals in Japan
- Improving sexual and reproductive health knowledge and practice in Mozambican families with media campaign and volunteer family health champions
- Exploring the influencing factors for non- utilisation of healthcare facilities during childbirth: a special mixedmethod study of Bangladesh and 13 other low- and middle- income countries based on Demographic and Health Survey data
