Cystic low-grade collecting duct renal carcinoma with liver compression — A challenging diagnosis and therapy:A case report
Zsolt Zoltan Fulop,Tivadar Jr Bara,Department of Surgery,George Emil Palade University of Medicine,Pharmacy,Science and Technology,Targu Mures 540139,Romania
Simona Gurzu,loan Jung,Laura Banias,Department of Pathology,George Emil Palade University of Medicine,Pharmacy,Science and Technology,Targu Mures 540139,Romania
Simona Gurzu,Emoke Fulop,Department of Pathology,Clinical County Emergency Hospital,Targu Mures 540067,Romania
Patricia Simu,Department of Radiology,George Emil Palade University of Medicine,Pharmacy,Science and Technology,Targu Mures 540139,Romania
Emoke Dragus,Department of Urology,Clinical County Hospital,Targu Mures 540167,Romania
Abstract
Key words:Collecting duct renal carcinoma;Hydatid cyst;Immunohistochemistry;Case report;Kidney;Therapy
INTRODUCTION
Collecting duct carcinoma (CDC),also known as carcinoma of the collecting ducts of Bellini,comprises fewer than 1% of malignant renal tumors[1,2].It originates from the collecting duct epithelium,which is located in the renal medulla[3].CDC has distinct clinical and pathological characteristics,such as hematuria,weight loss,back or flank pain and a local mass,but also fatigue and fever[2-6].It mostly appears in middle-aged men (male-to-female ratio = 2:1),with a right-sided laterality predominance (>2:1)[2,6,7,8].At the time of diagnosis,approximately one third of patients present with metastases in supraclavicular or cervical lymph nodes or distant metastases in the lungs,bones,liver or adrenal glands[2,4,6,7,9].
The presumptive diagnosis is highlighted by computed tomography (CT)characteristics.CDC is characteristically described as having medullary localization,with renal sinus involvement,heterogeneous enhancement,infiltrative growth,and preserved renal curve[7].
Microscopically,it has a tubular or tubulopapillary architecture[1,4,10].The World Health Organization established major criteria for diagnosing CDC,which is a diagnosis of exclusion.They include location in the medullary pyramid,irregular tubular architecture,without a component of urothelial carcinoma,with high nuclear grade,inflammatory desmoplastic stroma,which is accompanied by numerous neutrophils,together with immunohistochemical (IHC) reactivity to antibodies against high molecular weight cytokeratin and Ulex europaeus I (UEA1),respectively[4,7].
In this study,we present a patient with a large cystic low-grade CDC.After surgical excision,without postoperative oncological treatment but a strict postoperative follow-up,the patient is still alive,without complications,21 mo after surgery.
CASE PRESENTATION
Chief complaints
A 42-year-old male patient,with a body mass index of 28.75,was transferred from a regional hospital,to our University Surgery Clinic,due to right hypochondria pain and suspicion of a hydatid cyst of the liver.
History of present illness
The patient confirmed a one-month history of right hypochondria pain,without any other significant symptoms.
History of past illness
The patient was known to have chronic cholecystitis and mild hepatic steatosis.He declared himself a social drinker.
Personal and family history
No significant diseases or other information were confirmed.
Physical examination upon admission
During physical examination a large abdominal mass was palpated in the right hypochondria and the inferior edge of the liver,located 2.5 cm below the rib cage.
Laboratory examinations
The serum lymphocyte level was 16.4%,with a neutrophil-to-lymphocyte ratio (NLR)of 4.42.The serum levels of tumor-specific markers such as α-fetoprotein,carcinoembryonic antigen,and human choriogonadotropin were not evaluated but their positivity was denied by IHC staining.
Imaging examinations
The primary imaging investigation included ultrasonography,which described a nonhomogeneous round mass 119.2 mm × 108.3 mm in size,with increased echogenicity.The encapsulated mass was located in the 8thsegment of the right liver.Based on the patient’s personal history,the presumptive diagnosis was a hepatic cyst,associated with hepatosplenomegaly and hepatic steatosis.A right renal malrotation,with the right kidney localized in the epigastrium,was also suspected.The ureteral jet from the right side of the bladder was not visible.
A CT scan was also carried out.The scan confirmed the hepatomegaly and presence of a well-defined 126 mm × 121 mm × 146 mm macronodular encapsulated cystic lesion.The wall thickness was estimated to be approximately 6 mm.The fluid content was estimated to be clear,with a density of 10 HU.The cystic mass was thought to involve the convex side of the right kidney,with the upper limit at the visceral face of the liver,the lateral limit at the abdominal wall and the inferior limit at the bifurcation of the abdominal aorta.It displaced the right kidney in the anterior and medial direction (Figures 1-3).Hydronephrosis or signs of disorders of secretion or excretion of the right kidney were not described,neither were modified lymph nodes.Free abdominal fluid was observed.As the cystic lesion was classified as Bosniak type III,with a 50% potential of malignancy,surgical excision was planned.
Postoperative histopathological assessment
Macroscopic examination confirmed the presence of the encapsulated cystic mass,which involved the renal specimen.On the cut section,a blackish-brown appearance was evident.
The microscopic findings revealed the presence of tubular and papillary-like structures.The nuclei predominantly showed Fuhrman grade 2;the stroma did not show obvious desmoplastic areas,although it was infiltrated with neutrophils (Figure 4).Based on histological findings,a papillary carcinoma was initially diagnosed.As foamy macrophages were seen within the fibrovascular core,a variant of CDC was taken into account,for differential diagnosis.The tumor extended into both the cortical and medullary area,exceeded the renal capsule and infiltrated the perirenal adipose tissue (pT3 stage).No lymph nodes were identified in the surgical specimen.No clear cells or sarcomatoid dedifferentiation was identified.
Immunohistochemical profile
Tumor cells showed diffuse positivity for CD15 (clone:Carb-3,Dako) CTK AE1/AE3(clone AE1/AE3,ImmunoLogic),alpha-methylacyl-CoA racemase (AMACR clone 13H4,Dako),and vimentin (clone V9,Leica Biosystems),focal positivity for CTK7(clone OV-TL 12/30,A.Menarini Diagnostics) and CTK19 (clone RCK 108,Dako).No positivity was revealed for antibodies CD10 (clone Ab-2 56C6,Thermo Fisher Scientific),HER-2 (clone c-erbB-2,Dako),inhibin (clone Inhibin A,Leica),CD68 (clone KP1,ImmunoLogic;it marked the foamy macrophages within the fibrovascular core),Melan-A (clone A103,Cell Marque),Calretinin (clone Dak-Calret 1,Dako),human choriogonadotropin (polyclonal,Dako),carcinoembryonic antigen (polyclonal,Dako)or α-fetoprotein (polyclonal,Dako).The Ki67 (clone Mib-1,Dako) index was below 5% (Figure 5).

Figure1 Computed tomography images.
FINAL DIAGNOSIS
Based on the histological findings and immunoprofile of the tumor cells,the final diagnosis was established as pT3Nx-stage low-grade carcinoma of the collecting ducts of Bellini.
TREATMENT
After antibiotic prophylaxis,with second-generation cephalosporins,and thromboembolic prophylaxis with low molecular weight heparin,surgical intervention was carried out.The POSSUM predicted morbidity rate was estimated to be 29.3%,with a POSSUM predicted mortality rate of 5.3%.
Exploratory laparoscopy was initiated,followed by conversion to open surgery.Intraoperatively,involvement of the right kidney was observed and a histological examination confirmed the malignant potential.Based on this fact,a right nephrectomy,with tumorectomy,was performed.Due to diligent hemostasis,the surgical intervention lasted 150 min.
OUTCOME AND FOLLOW-UP
The patient was mobilized on the first postoperative day.Presenting favorable evolution,he was discharged 7 d after surgery.Postoperatively the patient’s health conditions were assessed by phone at 3 mo,6 mo,and 12 mo after discharge.
He did not receive postoperative oncological treatment,but in the first year following the surgical intervention,he attended oncological control examinations once every 3 mo.During the course of the first 12 mo,two ultrasonographies and one CT scan were performed,which described normal kidney function on the left side,without any suspicion of relapse on the right side.From the second postoperative year,control examinations were performed every 6 mo.After 18 mo,the laboratory investigations showed normal values and ultrasonography excluded any sign of relapse.The patient presents regularly at the nephrology clinic for evaluation of leftsided renal activity,which shows normal function.The patient states that he is in good general health,without any complaints 21 mo after surgery.

Figure2 lmage of thin maximum intensity projection coronal view contrast-enhanced excretory phase.
DISCUSSION
CDC is a rare but threatening genitourinary malignancy[9,10].It usually presents as a locally advanced,high-grade carcinoma,with bone metastases[9].In rare cases,these tumors can be large with a cystic appearance,such as in this case[3,11].
Due to its histological rarity,the optimal postoperative therapy requires elucidation[10].It should be based on a correct estimation of malignancy grade.As CDC is considered to show highly malignant behavior,the identification of low-grade cases,as an exclusion diagnosis,might be crucial for a thorough follow-up.Recent studies proposed using inflammation-related parameters for estimation of prognosis[12,13].An NLR ≥ 4 is considered an indicator of poor prognosis[12,14-16].In this case,although the value of the NLR was 4.42,the patient had a favorable prognosis,21 mo after diagnosis.
Current relevant literature is dominated mostly by case reports from small institutional cohort studies (Table 1)[3,11,17-27].The reported survival rate is controversial,being mostly reported as a median survival of 13-22 mo after diagnosis[5,9].The overall survival rate at 1 year and 3 years,for all stages,is reported to be 69% and 45%,respectively[2,5].A survival benefit of 4-5 mo only,is predicted with chemoradiotherapy[9].To date,there is no standardized treatment for metastatic CDC[8].In locally advanced cases,no chemotherapy is indicated after standard nephrectomy.It is recommended that the evolution of patients is followed,and if metastases appear,the histological examination and immunoprofile of the metastasis are necessary for individualized therapy[2].As HER-2 may be overexpressed[10],HER-2/neu amplifications can be indicators of anti-HER-2 medications.In metastatic CDCs,tumor regression was reported after targeted therapy with sunitinib or sorafenib[2,8].
Although there is a tendency for a detailed imaging diagnosis,in this particular case,a hepatic cyst was suspected on ultrasonography.CDC usually presents as a central medullary renal mass,showing minimal contrast capture;in rare cases,cortically situated satellite nodes are also described[2].Cystic renal masses are easily diagnosed on CT scans,if they belong to Bosniak type I or type IV.Bosniak type II and III cysts[3]may present a diagnostic challenge.
The diagnosis in our patient was difficult based on histological assessment,and supplementary IHC staining was carried out.As CDC is an exclusion diagnosis,the differential diagnosis should include papillary carcinoma,renal medullary carcinoma,and gland-forming urothelial carcinoma[3].Suspicion of CDC should be confirmed by Hematoxylin-Eosin staining and positivity for UEA I and a large spectrum of keratins,such CKHMW,CK AE1/AE3,CK7,and CK19,associated with positivity for CD15.CDC is negative for CD10,CK20 and villin and might display vimentin and HER-2 expression[1,3,5,6].HER-2 positivity,which was not identified in this case,is considered an indicator of poor prognosis[10].CDC also presents loss of heterozygosity and deletion of 1q32.1-32.2 and monosomy of chromosomes 1q,6p,8p,14,18,and 22[1,2].
Multicenter studies and clinical trials,based on the genetic profile of the tumor cells,need to be conducted to establish an effective adjuvant therapy.
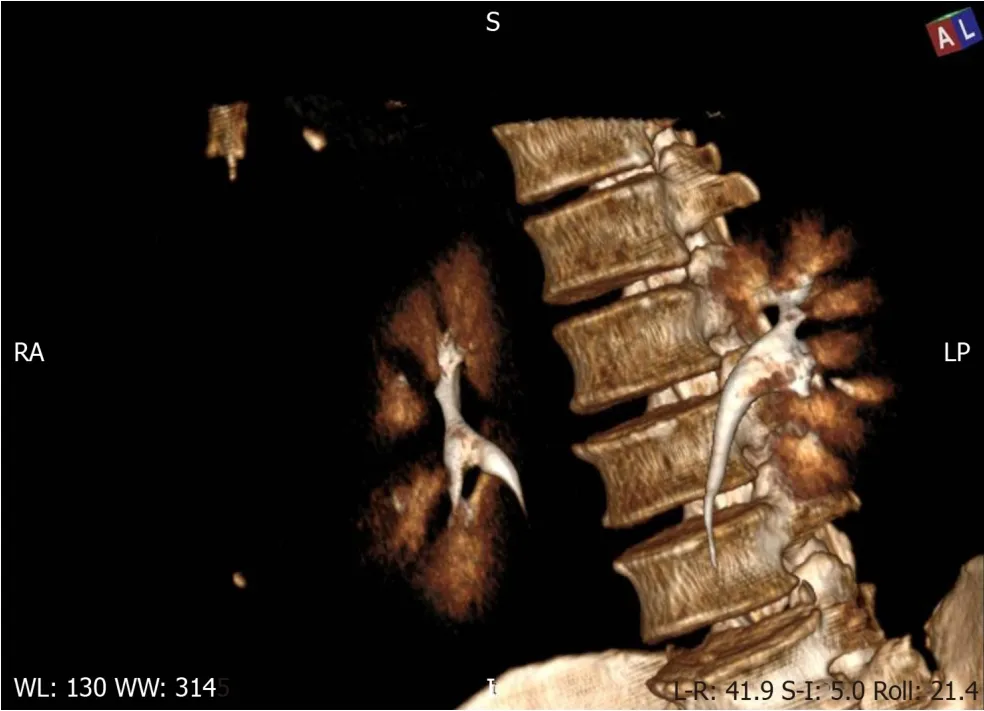
Figure3 Three-dimensional volume rendering technique of the contrast-enhanced excretory phase.
CONCLUSION
In patients with rare variants of renal carcinomas,such as CDC,an estimation of tumor grade is mandatory for an appropriate follow-up.The LNR cannot be used as a prognostic parameter.In metastatic cases,targeted therapy should focus on the genetic profile of tumor cells.
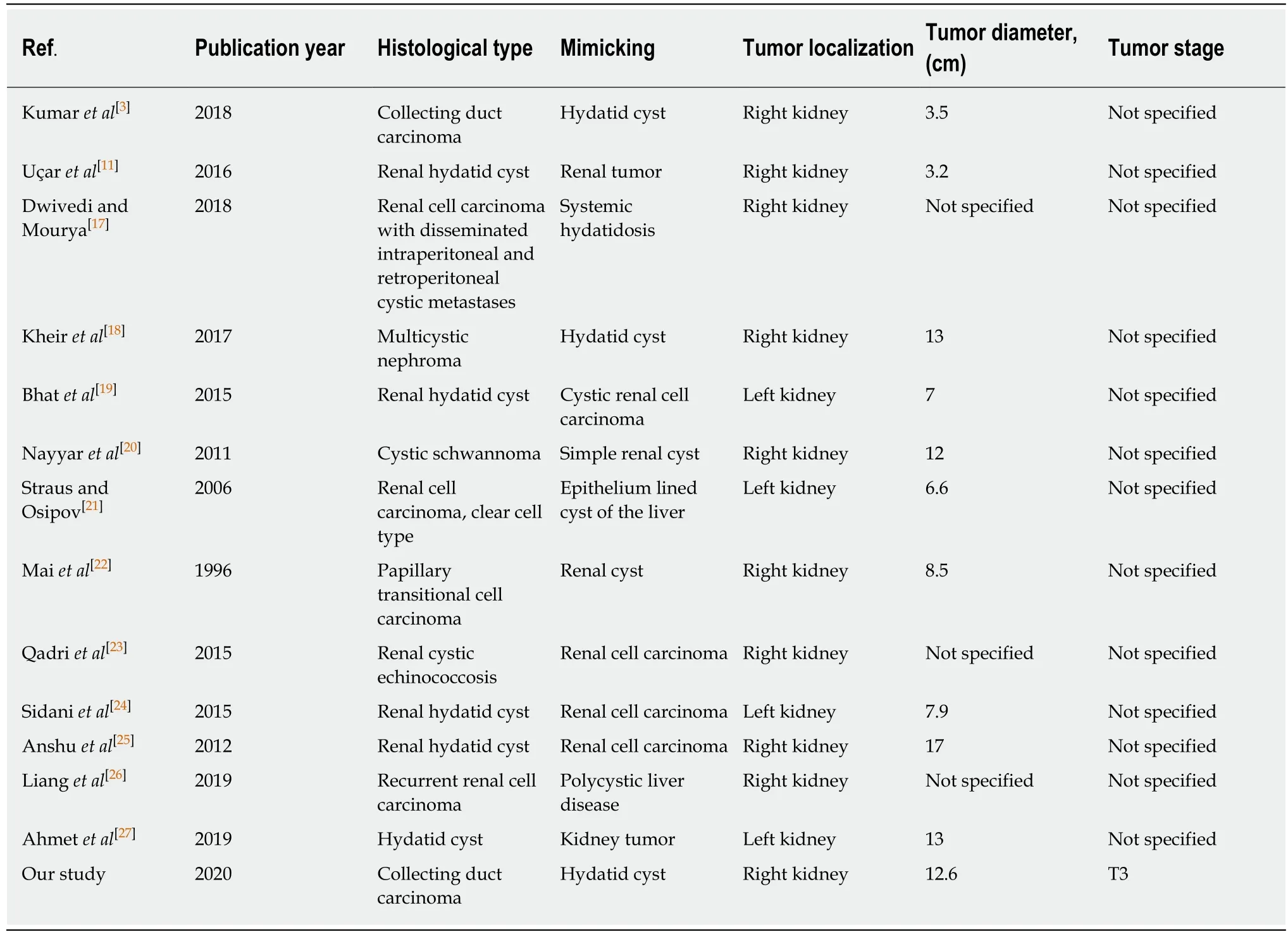
Table1 Clinicopathological characteristics of cystic renal lesions previously reported in the English literature
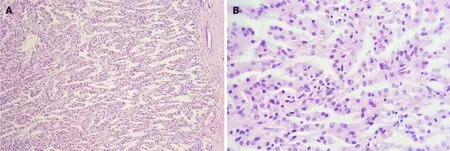
Figure4 Histological features of the collecting duct carcinoma.
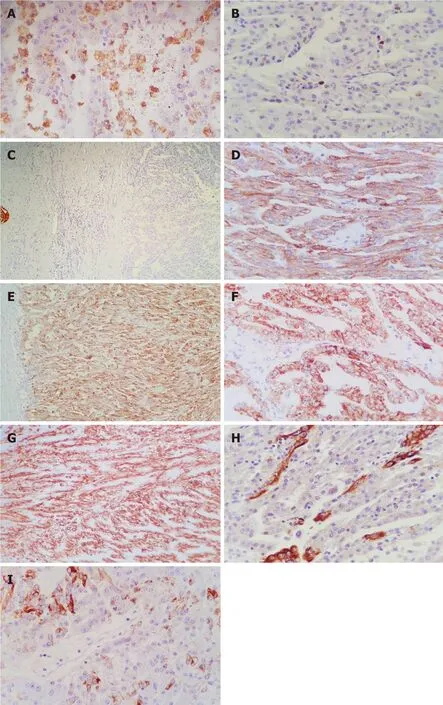
Figure5 lmmunohistochemical profile of the collecting duct carcinoma.
 World Journal of Gastrointestinal Surgery2020年6期
World Journal of Gastrointestinal Surgery2020年6期
- World Journal of Gastrointestinal Surgery的其它文章
- Robotic vs laparoscopic right colectomy - the burden of age and comorbidity in perioperative outcomes:An observational study
- Efficacy of the fat-dissociation method for nodal harvesting in gastric cancer
- Role of micronutrients in staging of nonalcoholic fatty liver disease:A retrospective cross-sectional study
- COVlD-19 outbreak and surgical practice:The rationale for suspending non-urgent surgeries and role of testing modalities
