Review of possible psychological impacts of COVID-19 on frontline medical staff and reduction strategies
Xiao-Wei Fu, Li-Na Wu, Ling Shan
Xiao-Wei Fu, Ling Shan, Department of Nursing, Lianyungang Maternal and Child Health Hospital, Lianyungang 222000, Jiangsu Province, China
Li-Na Wu, Department of Cardiothoracic Surgery, Affiliated Hospital of Xuzhou Medical University, Xuzhou 221000, Jiangsu Province, China
Abstract
Key words:Frontline medical staff;Psychological impacts;Epidemic diseases;Posttraumatic stress disorder syndrome;Adequate protective gear
INTRODUCTION
According to statistics released by the National Health Protection Committee in China,as of March 12, 2020, the total number of individuals infected with coronavirus disease-2019 (COVID-19) in the country was 80986, and the total number of successfully treated patients was 62950.Increasing cumulative number of cured patients can be attributed to the meticulous treatment and care provided by the medical staff throughout Hubei, more generally, and specifically by the 426000 frontline medical support staff in this province.As of February 24,2020,3387 medical staff had been afflicted by pneumonia caused by COVID-19.More than 90% of the infected medical staff were from Hubei, and 22 medical workers succumbed to COVID-19 according to statistics provided by the National Health Commission.An effective new treatment method for the highly infectious COVID-19 is still lacking, and the number of infected medical and nursing staff has gradually increased.Consequently, frontline medical personnel are under tremendous psychological pressure.The intense war waged against the epidemic has been ongoing for over 5 mo.This situation raises the following critical questions.What kinds of psychological pressure are being experienced by frontline medical staff? What are the impacts of the considerable psychological pressure on frontline medical staff? How can psychological pressure on frontline medical personnel arising from the epidemic situation be mitigated or avoided? Currently, pneumonia infections caused by COVID-19 continue to occur, and there is a paucity of research on the psychological pressure on frontline medical staff.The purpose of this review is to provide guiding inputs for solving these problems.
A large number of studies have reported that infectious epidemic diseases, such as severe acute respiratory syndrome (SARS), induce considerable psychological pressure that continues to impact frontline medical personnel a full year after such incidences[1].Therefore, effective and timely psychological interventions are critical for reducing the psychological pressure inflicted by the epidemic on frontline medical staff, improving the work outcomes of these staff, and reducing the long-term impacts of the epidemic on them.At an early stage of the epidemic disease, there was a lack of comprehensive awareness of the disease and corresponding protective measures.Consequently,frontline medical staff experienced psychological conflicts, as being torn between their responsibilities and ensuring their own safety.The resulting psychological pressure on these individuals was extensive given the increasing numbers of infections among their colleagues.A positive development has been the government’s increasing awareness and attention to the psychological stress endured by medical staff under current conditions of the COVID-19 epidemic.On March 8, 2020, the National Health Commission dispatched 415 mental health professionals to Hubei to provide professional psychological consultations and crisis intervention services for patients and medical staff.However, these interventions are woefully inadequate.An understanding of the sources of the psychological pressure experienced by frontline medical staff is critically required to aid the formulation of targeted policies and efforts that fundamentally reduce this pressure.
In this paper, we present the findings of a review of studies that have investigated the psychological pressure and causes of stress associated with previous outbreaks of infectious diseases, such as SARS and influenza A (H1N1).The characteristics of studies that met our inclusion criteria are presented in Table 1.We further examine potential solutions for reducing the impacts of stress on frontline medical staff following the current outbreak of COVID-19 pneumonia so that they can resume their normal lives as soon as possible.These measures also provide the basis for
psychological interventions targeting frontline medical staff prior to the outbreak of epidemic infectious diseases in the future to reduce or avoid the pressures and impacts of these epidemics on them.
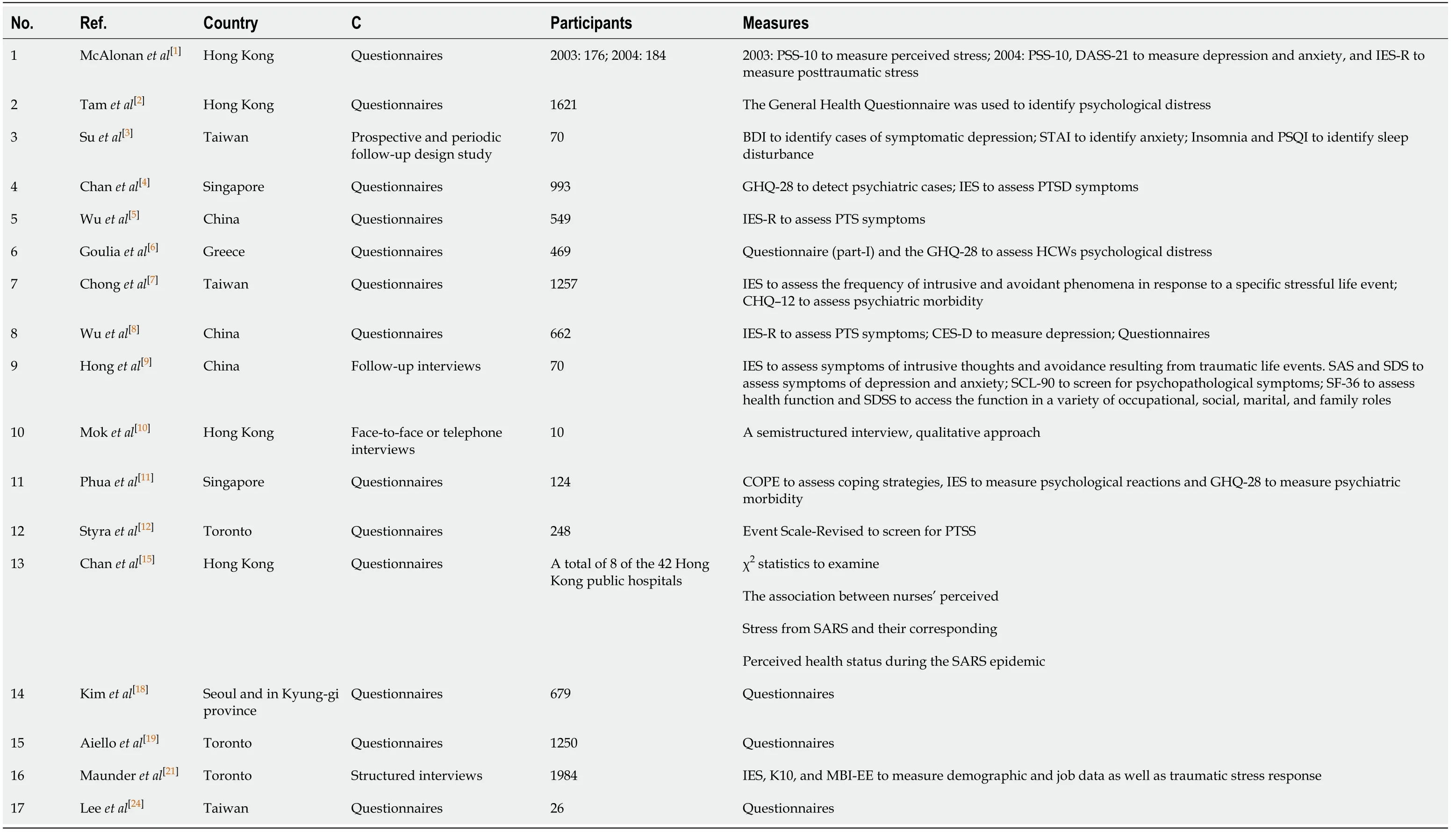
Table 1 Study characteristics
PSYCHOLOGICAL INFLUENCES OF EPIDEMIC DISEASES ON FRONTLINE MEDICAL STAFF
According to findings reported in the literature, the psychological impacts of epidemic diseases on frontline medical staff are universal.Different researchers working in diverse regions on different diseases have all reached the same conclusion:epidemic diseases extensively impact frontline medical staff, with typical symptoms and a long duration.One such study entailed an investigation of 652 frontline medical workers combatting SARS in three hospitals in Hong Kong.A total of 68% of these medical workers reported that they were under great pressure, with about 57% of them experiencing psychological pain[2].The findings of a second study conducted on nurses in SARS hospital wards in Taiwan in 2003 found that 33% of the nurses suffered from post-traumatic stress disorder (PTSD)[3].In a third study, 661 frontline medical staff at a Singapore middle hospital were interviewed.Approximately 20% of the respondents had PTSD[4].A fourth study conducted in China revealed that since the outbreak of SARS in this country, about 10% of the medical staff have experienced symptoms indicating high levels of post-traumatic stress (PTS)[5].Moreover, more than half(56.7%) of the researchers investigated in another study suffered from high levels of anxiety during the outbreak of H1N1[6].
Most of the specific psychological symptoms experienced by frontline medical staff in relation to epidemic diseases are relatively common and include anxiety, insomnia,depression, interpersonal difficulties, and PTSD.In addition, they experienced physical problems caused directly or indirectly by these psychological problems.During the early stages of an outbreak of an infectious disease when its spread is rampant, frontline medical staff perceive it as life threatening and experience feelings of extreme vulnerability and uncertainty, which mainly manifest as physical and cognitive anxiety symptoms.During the recovery period after the infection has been brought under control, symptoms of depression and a desire to escape are evident[7].McAlonanet al[1]investigated the psychological stress experienced by frontline medical staff during the SARS outbreaks in 2003 and 2004, respectively, using the perceived stress scale, the depression anxiety stress scale, and a revised version of the events scale.The results of the study revealed that frontline medical personnel evidenced mental problems, such as fatigue, poor sleep quality, worry about health status, and fear of social interactions in 2003.Moreover, in 2004, the stress had been transformed into chronic depression, anxiety, PTS, and other symptoms[1].The findings of another study showed that exposure to severe infectious diseases could not only lead to PTSD but it could also lead to other mental diseases, such as alcoholism or alcohol dependence[8].Chronic stress can weaken the immune system and increase the risk of disease;in addition, stress can adversely impact cognitive functions and task performance.Further research is, however, needed to determine whether this kind of psychological pressure will affect the work of frontline medical staff in future outbreaks of epidemic diseases.Therefore, it is very important for hospital managers to reduce or avoid the short-term and long-term psychological impacts of an epidemic on frontline medical staff.
The impacts of epidemic diseases on frontline medical personnel are not limited to the duration of their outbreak, and they may last a long time.The results of a survey indicated that about 40% of the respondents still experienced high-level PTS symptoms 3 years after the SARS outbreak during the interview[5].Moreover, another study found that 44.1% of SARS patients still had PTSD 4 years after the epidemic[9].These findings raise the following question:How long do the impacts of an epidemic endure among frontline medical staff? Currently, there are no reported research results.Therefore, continued investigations are required to obtain solid scientific research data and to make comprehensive preparations for future outbreaks of epidemic diseases.
Although sudden outbreaks of epidemic diseases have significant physiological and psychological impacts on medical personnel, they also have certain positive effects[2,10].According to the investigated medical staff, sudden outbreaks of epidemic diseases induce a new understanding of life and interpersonal relationships, leading to positive changes relating to the setting of priorities, such as greater relaxation and having more fun in life.We hope that more frontline medical staff will experience such positive impacts of the epidemic through our efforts.
STRESSORS DURING EPIDEMIC DISEASE OUTBREAKS
The findings of our review revealed that during the outbreak of an epidemic disease,frontline medical staff experience considerable pressure emanating from different sources.To reduce the psychological pressure on frontline medical staff, it is necessary to know the sources of this pressure.The following main sources of pressure were derived from the literature.
Individual
A number of studies have reported that the most disturbing aspect of disease outbreaks that creates psychological pressure is the infection of medical personnel[2,11].Such infections raise concerns among individual staff members about their vulnerability, as they share similar personal characteristics and are emotionally identified with their sick colleagues.The findings of a survey revealed that the personal risk level of frontline medical staff was an undeniable source of stress.In addition to worrying about themselves, some of the interviewees expressed more concern about the health of their relatives[12].They deliberately avoided close social contact to reduce the risk of transmission to relatives.Consequently, their family lives and social relations were seriously damaged.In addition, the repeated emphasis on disease incidence and mortality rates during this period within the media may have been an added source of trauma for many medical personnel, either directly or indirectly[4].
Roles
Role-related pressure mainly stems from the conflict between professional responsibility and the helplessness of medical personnel.Members of the public place high hopes on medical personnel and highly value their professionalism.The public perception is that professionals should be selfless and brave in battle.However, many staff members experience doubts relating to their self-efficacy and even their medical knowledge.Any delay or misdiagnosis incurs a risk of becoming infected and of infecting colleagues, other medical staff, and family members, and such individuals will also be admonished by their superiors[4].Maintaining this state of high alert over a long stretch of time leads to extreme stress for frontline medical staff resulting in a high incidence rate of anxiety disorders.
Work
Most respondents in studies that examined work-related factors complained about unclear policies, inadequate information dissemination, and a lack of feedback mechanisms.During the SARS outbreak, heavy personal protective equipment (PPE),strict infection control measures, and the news of colleagues' illness or death caused tension and strained atmosphere in emergency rooms and hospitals[4,11].
Interpersonal relationships
One study reported that frontline medical staff feared being isolated from members of their families, their spouses, children, and society during an outbreak[13].During the SARS outbreak, some families refused to support nurses, and some spouses of medical staff were forced to take temporary leave, while their children were asked to stay away from school.These social phenomena have significant impacts on frontline medical staff.Some nurses feel very depressed because they have no place to go except the hospital, which is their workplace[14,15].This issue raises the question of what can be done to mitigate the impact of the epidemic on medical staff.
Evidently, effective measures are required that target the source of the pressure,with the aim of effectively reducing the psychological pressure experienced by frontline medical personnel as much as possible.Below, we present psychological measures targeting frontline medical personnel reported in the literature.
MEASURES FOR REDUCING PRESSURE ON FRONTLINE MEDICAL STAFF
Full protection measures of frontline medical staff
Practical measures for ensuring that frontline medical staff are free from infection during the epidemic are a primary concern.Controlled case studies conducted in five hospitals in Hong Kong revealed that medical staff wearing PPE (masks, goggles,gloves, and robes) and practicing hand washing were less likely to develop SARS than those who did not take such measures[16].Ideally, full protection for frontline medical staff can be provided, preventing their exposure to the risk of infection.Hospitals should therefore provide frontline medical staff with the best and most effective protective gear, such as protective clothing, N95 masks, goggles, boots, and surgical gloves.To meet the safety needs of medical staff more effectively, PPE of different types and sizes can be provided that cater to the needs of different people[17].Adequate protective measures can greatly alleviate the anxiety and worry of frontline medical staff regarding the possibility of infection.In addition, taking a bath after each shift in the hospital minimizes the possibility of transmission of the SARS-coronavirus-2 from the hospital to the families and communities of medical staff, thereby reducing the worry of medical personnel about infecting their families and friends with the virus.
Timely and clear guidelines
Many medical staff were infected with COVID-19 because the characteristic features of human transmission of COVID-19 during the outbreak were unknown.This knowledge gap undoubtedly increased the panic and anxiety of frontline medical staff.It was impossible to provide appropriate guidelines and policies for infection management because of the lack of understanding regarding the pathogen during the early stage of the outbreak.Nurses have been instructed to use PPE every hour,leading to their confusion and depression[15].When individuals are constantly exposed to uncontrollable events, they feel helpless, experiencing a reduced sense of control over outcomes along with depression and a lack of motivation to solve new problems[10].Uncertainty is reduced through the possession of knowledge.During the period of the epidemic, medical personnel on the front line should be regularly provided with the latest available information on the disease.Access to such information not only promotes their timely responses but it also contributes to patients’ education and a reduction of their psychological problems and worries.Clearly, it takes time to develop an understanding of the pathogen during the early stages of an outbreak.However, valuable experiences elicited from previous outbreaks can be compiled to form a set of centralized and integrated mechanisms for effectively disseminating information to frontline medical staff.With a gradual deepening of understanding of the disease, the corresponding process for dealing with it will also gradually improve.Hospitals should apply state guidelines on the epidemic in a timely manner to impart immediate learning to frontline medical staff.Accordingly,they will grasp the latest information and treatment methods so as to formulate possible treatment plans, infection control policies, and personal protection measures.Consequently,the confidence of frontline medical staff in the face of the epidemic will be enhanced and their concerns will be reduced.
Social support
Having the support of their family members, friends, colleagues, and society greatly influences the willingness of medical staff to care for patients during the outbreak of an epidemic[2,4,13].A study found that Korean nurses were reluctant to take care of SARS patients due to lack of support from family and friends[18].Frontline medical staff are afraid to tell others what they do because they are afraid that they and their family members will become outcasts.Medical staff were not allowed to go home because they were engaged in frontline work during the COVID-19 outbreak, which undoubtedly added to the heavy psychological pressure that they were already experiencing.On the one hand, societal resonance and support for frontline medical staff can be strengthened through advocacy and publicizing of their achievements,thereby enhancing their psychological well-being.On the other hand, the professional beliefs of frontline medical staff can be enhanced to strengthen their conviction that taking care of patients is the right choice and to convince people around them that as medical staff, they know how to protect themselves and their families from infection.
Training
The research findings indicate that the contents of training programs conducted during the epidemic entail many aspects.The imparting of different themes has varying but significant effects on frontline medical staff.For example, to increase frontline medical staff’s knowledge of epidemic diseases and infection control, the speaker, who understood the needs of the trainees, designed an education plan and training program.The main content of the training program comprises information on epidemic diseases, the correct use of PPE, risks for medical staff and their families, and infection control policies and procedures.One study found that the proportion of participants who felt confident about coping with influenza after participating in the training program (76%) was significantly higher than the proportion of those with such confidence before the training session (35%)[19].
Another study emphasized the importance of providing training and education to all hospital staff members on all aspects of SARS during the outbreak period to enable them to cope better with future outbreaks of infectious diseases[20].For example,frontline medical staff could receive training in which stress management is the core component to guide them toward mobilizing their self-efficacy.Such training can be helpful for the early detection of high-risk groups that cannot effectively adjust themselves during the epidemic.There is evidence that mental health resilience, which is the ability of individuals to adjust and optimize their psychological and physical needs, is particularly important during the outbreak of epidemic diseases[21].In addition, training is required that focuses on strengthening the professional dignity of frontline nursing staff and alleviating job burnout.During the outbreak of epidemic diseases, job burnout is considered to be one of the most serious health-related problems faced by nurses[22].Enhanced support and training can reduce burnout and PTS.One study found that a pilot training workshop held for primary healthcare workers to manage acquired immunodeficiency syndrome patients greatly improved the participants’ attitudes[23].Such training programs lead to the development of skills and confidence among medical staff that enable them to improve their personal efficiency, enhance their professional dignity, and reduce job burnout.
Selection of frontline medical staff
The selection of frontline medical staff should be done cautiously to minimize the impacts of epidemic diseases on them in the face of heightened tensions relating to future biological disasters.One study found that when working in a high-risk ward,frontline medical staff who had more contact with SARS patients experienced less pain[12].This finding suggests that if conditions permit, medical staff who have previous experience relating to the treatment and care of patients afflicted by epidemic diseases should be selected preferentially in the future.This is because choosing such individuals would contribute to reducing the impacts of the epidemic on the frontline medical staff.A history of mood disorders and an age below 30 years may be risk factors predicting depression, PTS symptoms, and sleep disorders[3].In addition to the above described measures, professional psychological consultants should be included in crisis working groups at an early stage of the outbreak in view of the long-term and deep impacts of the epidemic on frontline medical staff[24].Their inclusion would enable frontline medical workers to get timely and effective psychological consultations, thereby reducing the impacts of the epidemic on them.
Other measures
Some studies have also suggested other ways of relieving the psychological stress experienced by frontline medical staff, such as humor[11].One such study showed that nurses and emergency workers used humor to deal with crises[25].Other studies have found that humor has a positive meaning because it can shift perspectives, disperse tension, improve energy levels, and build cohesion within the team, in addition to strengthening an individual’s physical, psychological, and spiritual abilities[26,27].Some studies have found that SARS patients can also alleviate the trauma caused by the epidemic through tai chi[28].However, further studies are needed to assess whether tai chi can relieve psychological pressure experienced by frontline medical staff.During the initial outbreak of COVID-19, it was reported that frontline medical staff and patients in some hospitals in Wuhan danced rhythmically in the square to relieve their inner tension and discomfort.
CONCLUSION
When faced with another epidemic brought about by COVID-19, there was a sudden realization of how valuable the experience of beating SARS was.The valuable experiences brought by each epidemic disease outbreak should be applied in planning for future pandemics.With the gradual increase of relevant research, people are becoming increasingly aware of the psychological problems endured by frontline personnel during an epidemic.Therefore, one of the main goals for improving the ability of medical staff to deal with future outbreaks must be to improve their capacities to deal with psychological stress.This paper has presented the findings of a review of studies that assessed the impacts of the SARS epidemic on frontline medical staff and potentially effective solutions, with the aim of reducing the impacts of future epidemic diseases on frontline medical staff and providing guiding inputs for comprehensive preparatory work.
 World Journal of Clinical Cases2020年15期
World Journal of Clinical Cases2020年15期
- World Journal of Clinical Cases的其它文章
- Impacts and challenges of United States medical students during the COVID-19 pandemic
- Recent advances in the management of gastrointestinal stromal tumor
- Medical research during the COVID-19 pandemic
- Progress of intravoxel incoherent motion diffusion-weighted imaging in liver diseases
- Typical and atypical COVID-19 computed tomography findings
- Overexpression of AMPD2 indicates poor prognosis in colorectal cancer patients via the Notch3 signaling pathway
