Separate lateral parametrial lymph node dissection improves detection rate of parametrial lymph node metastasis in early-stage cervical cancer:10-year clinical evaluation in a single center in China
Dan Zhao ,Bin Li ,Shan Zheng ,Zhengjie Ou ,Yanan Zhang ,Yating Wang ,Shuanghuan Liu,Gongyi Zhang,Guangwen Yuan
1Department of Gynecology Oncology,National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital,Chinese Academy of Medical Sciences and Peking Union Medical College,Beijing 100021,China;2 Department of Pathology,National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital,Chinese Academy of Medical Sciences and Peking Union Medical College,Beijing 100021,China
Abstract Objective:To investigate the clinical significance of separate lateral parametrial lymph node dissection(LPLND) in improving parametrial lymph node (PLN) and its metastasis detection rate during radical hysterectomy for early-stage cervical cancer.Methods:From July 2007 to August 2017,2,695 patients with cervical cancer in stage IB1-IIA2 underwent radical hysterectomy were included.Of these patients,368 underwent separate dissection of PLNs using the LPLND method,and 2,327 patients underwent conventional radical hysterectomy (CRH).We compared the surgical parameters,PLN detection rate and PLN metastasis rate between the two groups.Results:Compared with CRH group,the rate of laparoscopic surgery was higher (60.3% vs.15.9%,P<0.001),and the blood transfusion rate was lower (19.0% vs.29.0%,P<0.001) in the LPLND group.PLNs were detected in 356 cases (96.7%) in the LPLND group,and 270 cases (11.6%) in the CRH group (P<0.001),respectively.The number of PLNs detected in the LPLND group was higher than that in the CRH group (median 3 vs.1,P<0.001).The PLN metastases were detected in 25 cases (6.8%) in the LPLND group,and 18 cases (0.8%) in the CRH group (P<0.001),respectively.In multivariable analysis,LPLND is an independent factor not only for PLN detection [odds ratio (OR)=228.999,95% confidence interval (95% CI):124.661-420.664;P<0.001],but also for PLN metastasis identification (OR=10.867,95% CI:5.381-21.946;P<0.001).Conclusions:LPLND is feasible and safe.The surgical method significantly improves the detection rate of PLN and avoids omission of PLN metastasis during radical hysterectomy for early-stage cervical cancer.
Keywords:Cervical neoplasm;radical hysterectomy;parametrectomy;parametrial lymph nodes;lymph node excision;lymphatic metastasis
Introduction
Cervical cancer remains a major global health threat to females,especially in developing countries.The number of new cases in China each year is approximately 98,900,causing 30,500 deaths,the second highest in the world (1).Radical hysterectomy is presently the standard-of-care for International Federation of Gynecology and Obstetrics(FIGO) stage IB-IIA cervical cancer,with a cure rate of greater than 80% (2).Extensive resection of cardinal ligament is the key step of radical surgery and also a surgical procedure that is risky to complications.The main reason for complications of conventional radical hysterectomy (CRH) is that the cardinal ligament is not dissected meticulously,and the surrounding blood vessels and autonomic nerves are damaged due to the integrally clamping and cutting of the cardinal ligament.In addition,the conventional surgical step might result in the state of parametrial lymph nodes (PLNs) located in the cardinal ligament undetected.According to current anatomical concepts,the so-called “cardinal ligament” is a complex structure composed of supplying blood vessels,parametrial lymphatic tissue,and autonomic nerves of the uterus,rather than the actual supporting ligament.Regarding these contents,removal of PLNs is so closely related to surgical radicality (3-6).In 2008,Querleu and Morrow proposed a new classification for cervical cancer radical surgery (7),and after revision and update in 2017,it has become widely accepted (8).In Q-M classification,the concept of “cardinal ligament” is faded,and replaced by“l(fā)ateral parametrium” (7,8). Moreover, paracervical lymphadenectomy is added to the B2 subtype of Q-M classification,with the purpose of expanding the lateral radicality of surgery without increasing complications (7,8).The paracervical lymphadenectomy is described as the removal of the lymph node tissues below the obturator nerve and around the deep uterine vein (7).It has been purposed to avoid clamping of the parametrium at the pelvic wall,along with nerves and vessels during traditional radical hysterectomy.Thus,it can reduce hemorrhage and nerve injury.H?ckelet al.(9) and Querleuet al.(10) had introduced this method into nerve sparing radical hysterectomy,as an alternative to the traditional resection of cardinal ligament.But the paracervical lymphadenectomy was rarely reported after Q-M classification was proposed,and its clinical significance,especially for the efficacy on detection of PLN remains unclear.
Since 2008,authors of this study have proposed a method,which is similar to the above mentioned paracervical lymphadenectomy,called “l(fā)ateral parametrial lymph node dissection (LPLND)”.In this study,we intend to investigate clinical significance of LPLND method in improving PLN and its metastasis detection rate during the radical hysterectomy for early-stage cervical cancer.
Materials and methods
Patients
From July 2007 to August 2017,2,695 patients with stage IB1-IIA2 (FIGO 2009) cervical cancer underwent radical hysterectomy (Piver type III or Q-M type C) in the Department of Gynecological Oncology,Cancer Hospital of the Chinese Academy of Medical Sciences.Among all patients,368 cases underwent separate PLN dissection using LPLND method in processing lateral parametrium resection,which was performed by Dr.Li Bin and other three senior gynecologists in the team (LPLND group).The remaining 2,327 patients underwent conventional radical hysterectomy by other surgeons from the same department (CRH group),and the two groups were compared retrospectively.During the study period,radical hysterectomy was carried out by laparotomy or laparoscopy.Since 2012,laparoscopic surgery has been widespread used in LPLND group.This study was approved by the local Ethics Committee of Cancer Hospital,Chinese Academy of Medical Sciences.
Evaluation and adjuvant treatment
Preoperative biopsy confirmed the pathologic diagnosis of cervical cancer,and two senior gynecologic oncologists performed pelvic examinations to determine the clinical stage.Enhanced computerized tomography (CT) scan and magnetic resonance imaging (MRI) were used to evaluate parametrial invasion and distant metastasis.Patients with high or intermediate pathologic risk factors (non-squamous histology,lymph node metastasis,parametrial infiltration,positive margins,lymph-vascular space invasion,deep stromal invasion, and bulky tumors) were received postoperative adjuvant treatments,including concurrent chemoradiotherapy,external radiotherapy,brachytherapy,and systemic chemotherapy. External radiotherapy combined with platinum-based concurrent chemotherapy was the primary regimen.
Procedures of CRH
Pelvic lymphadenectomy was performed initially and the resection range was the common iliac artery on the cephalic side,the deep circumflex vein on the caudal side,the psoas and internal obturator muscles on the lateral side,the internal iliac artery on the medial side,and the pelvic floor muscle surface on the dorsal side.All lymphatic adipose tissues surrounding the iliac vessels and in the obturator fossa were removed completely,including lymph nodes below the obturator nerve. Para-aortic lymphadenectomy was performed in patients with common iliac lymph node metastasis or locally advanced diseases.
CRH was performed according to Piver type III or Q-M type C standards.The procedures were as follows:the uterine artery was cut at its origin;the ureter was completely freed;the lateral parametrial tissue (cardinal ligament) was cut at pelvic sidewall;the dorsal parametrial tissue (uterosacral ligament) was cut at sacrum;the ventral parametrial tissue (vesicocervical ligament) was cut at the bladder wall,and the vagina was excised 2 cm away from the lesion.In CRH group,the lateral parametrial tissue was resecteden bloc,without meticulous dissection of the blood vessels and lymphatic adipose tissues.
Procedures of LPLND
LPLND and CRH group have different procedures in resecting the lateral parametrium,the rest of the surgical steps are the same.LPLND separates lateral parametrial uterine vessels and lymphatic tissues referring to the paracervical lymphadenectomy method described in Q-M classification (7).This method emphasizes the separate removal of paracervical lymph tissue around the deep uterine veins,as well as the lymph nodes to the medial and deep side of the obturator nerve (7).In our study,lymph nodes in the deep side of obturator nerve were resected together with the pelvic lymph nodes and were no longer treated as PLNs.LPLND highlighted resecting the PLNs not only around the deep uterine vein but also the small lymph nodes accompanied by the uterine artery (Figure 1).The specific surgical procedures were as follows:developing paravesical and pararectal spaces on the medial side of internal iliac artery to the pelvic floor,exposing the internal iliac vein and its branches.The parametrial lymphatic tissues were fully exposed between these two spaces.Along uterine artery,superficial uterine vein and deep uterine vein,all surrounding PLNs were separated and dissected.Then the resected PLNs were sent for pathological examination separately. Ultimately, the uterine vessels were fully skeletonized and divided at the origin,and the resection of the lateral parametrium was completed.
Pathologic examination
Details of pathological examinations were as follows:the bilateral parametrial tissue was completely removed,the thickness of the parametrial soft tissue was recorded,and was cut in the form of page turning at 0.5 cm intervals to carefully search PLNs.Palpated PLNs were separated and sent for routine pathological examination.If no suspected PLN was palpated,three discontinuous sections on each side of the parametrial tissue were paraffin-embedded and then sectioned at a thickness of 3-4 micrometers and performed hematoxylin &eosin staining (H&E) staining.PLNs were detected under microscopy and reviewed by at least two senior pathologists.
Statistical analysis
IBM SPSS Statistics (Version 24.0;IBM Corp.,New York,USA) was used for statistical analysis,and χ2test was used for counting data comparison.In the measurement data,those with normal distribution were expressed asand were compared byttest,while those without normal distribution were compared by mann-whitneyUtest.Besides,categorical variables were compared between the two groups using the Pearson Chi-squared test or Fisher’s exact test.Univariative and multivariative analysis were performed by logistic regression model.In all cases,odds ratio (OR) is presented with 95% confidence interval (95%CI),and a two-sided P-value of <0.05 indicates statistical significance.
Results
Comparison of clinical-pathological characteristics
There were 368 cases in LPLND group and 2,327 in CRH group.The two groups in age,body mass index (BMI),menopausal status,FIGO stage,histotype,grade,lymph vascular space invasion (LVSI),depth of stromal invasion,parametrial invasion,lymph node metastasis,percentage of receiving adjuvant radiotherapy and chemotherapy were not statistically different.The percentage of patients undergoing laparoscopic surgery in the LPLND group was significantly higher than that in the CRH group (60.3%vs.15.9%,respectively;P<0.001),while the blood transfusion rate was significantly lower in the LPLND group compared to the CRH group (19.0%vs. 29.0%,respectively;P<0.001).The operation time in the LPLND group was longer than that in the CRH group (254.23±59.88 minvs.247.69±56.97 min,respectively;P=0.042),while there was no difference in hospitalization between the two groups (Table 1).
Comparison of PLN detection and metastasis
In 356 patients (96.7%) of the LPLND group,PLNs were detected in separate dissected parametrial lymphatic tissue,of which 52 cases were detected by pathologists in the uterine gross specimen.In the CRH group,pathologists routinely examined the gross uterine specimens,and PLNs were detected only in 270 cases (11.6%).The PLN detection rate of the LPLND group was significantly higher than that of the CRH group (P<0.001);and the detection rate of bilateral PLNs in the LPLND group was also significantly higher than that in the CRH group(61.1%vs.1.4%,respectively;P<0.001).The median number of detected PLNs in the LPLND and CRH groups were 3 and 1 respectively, which differed significantly (P<0.001);the number of dissected pelvic lymph nodes was similar in two groups,with a median number of 28 and 29 respectively (P=0.083).PLN metastases were found in 25 cases (6.8%) in the LPLND group,and 18 cases (0.8%) in the CRH group.The difference of PLNs metastatic rate between the two groups was statistically significant (P<0.001) (Table 2).
Independent factors for PLN detection and its metastasis
In multivariate analysis,by incorporating age,year of diagnosis, BMI, menopausal status, FIGO staging,histotype, grade, LVSI, depth of stromal invasion,parametrial invasion,lymph node metastasis,surgical method,operative approach,and blood transfusion into univariate and multivariate analysis,it was demonstrated that year of diagnosis (P=0.017),grade (P=0.021) and surgical method (P<0.001) were independent factors for PLN detection, while LVSI (OR=2.980, 95% CI:1.536-5.783;P=0.001),parametrial invasion (OR=5.804,95% CI:1.111-30.312;P=0.037) were independent factors for PLN metastasis,and surgical method (P<0.001) was independently related to the detection of PLN metastasis(Table 3,4).
Distribution of lymph node metastasis in patients with detected PLNs
Lymph node metastasis occurred in 116 patients with detected PLNs in the LPLND and CRH groups.Of these,43 (37.1%) patients showed PLN metastasis.Among the 43 cases,15 (12.9%) cases had isolated PLN metastasis,14(12.1%) patients had lymph metastases of both the PLNs and ipsilateral pelvic lymph nodes,10 (8.6%) patients had lymph metastases of unilateral PLNs and bilateral pelvic lymph nodes,and 4 (3.4%) patients had metastases of unilateral PLNs and contralateral pelvic lymph nodes.Another 73 (62.9%) patients showed no PLN metastasis but had pelvic lymph node metastasis (Table 5).
Discussion
LPLND proposed by this study is the modification of paracervical lymphadenectomy described in Q-M classification.We performed LPLND in 368 patients with early-stage cervical cancer in ten years,which confirmed the feasibility and repeatability of this surgical method.For our best knowledge,our series has the largest number of cases in the studies related to the PLN resection.
In the LPLND procedure,the excision of lateral parametrium met the standard of type C surgery in Q-M classification,which ensured the radicality.The LPLND method was safe and easy to perform.Moreover,due to the separate resection of PLNs and blood vessels,it was performed in a more meticulous and less bleeding way,comparing with the conventionalen blocparametrial resection.In addition,LPLND also differed from the paracervical lymphadenectomy described in Q-M classification,which highlighted the removal of the lymph nodes below to the obturator nerve and around the deep uterine vein (7).In our study,the removal of deep obturator lymph nodes was no longer included into the LPLND procedure,because this group of lymph nodes had already been removed by pelvic lymphadenectomy previously.During LPLND procedure,we dissected PLNs from the uterine vessels,including not only paracervical lymph nodes around the deep uterine veins,but also PLNs distributed along the uterine artery.We believe that LPLND should be more effective in harvesting PLNs,since the extent of LPLND was consistent with the actual distribution of PLNs described by several studies (11-15).In our study,the PLN detection rate in LPLND group was 96.7%,higher than 60.5% which was reported by Sunet al(16).The study had adopted separate PLN dissection similar to LPLND,but operative approaches were not exactly the same.All the surgeries in Sun’s study were performed by laparotomy,while most in our study completed by laparoscopy.In this study,laparoscopic surgery was commonly used in LPLND group since 2012,which significantly improved the detection rate of PLN.Querleuet al.(10) pointed out that the magnification effects on the surgical field and precise surgical operation under laparoscopy can facilitate the recognition of PLNs.Hence,laparoscopic surgery might increase the removal of PLNs,especially to the identification and dissection of small PLNs along the uterine artery.Recently,two studies found that laparoscopy had worse impact on prognosis.Then the studies recommend laparotomy as the standard approach for early-stage cervical cancer (17,18).Nevertheless,LPLND could be performed with the aid of surgical loupe during laparotomy.
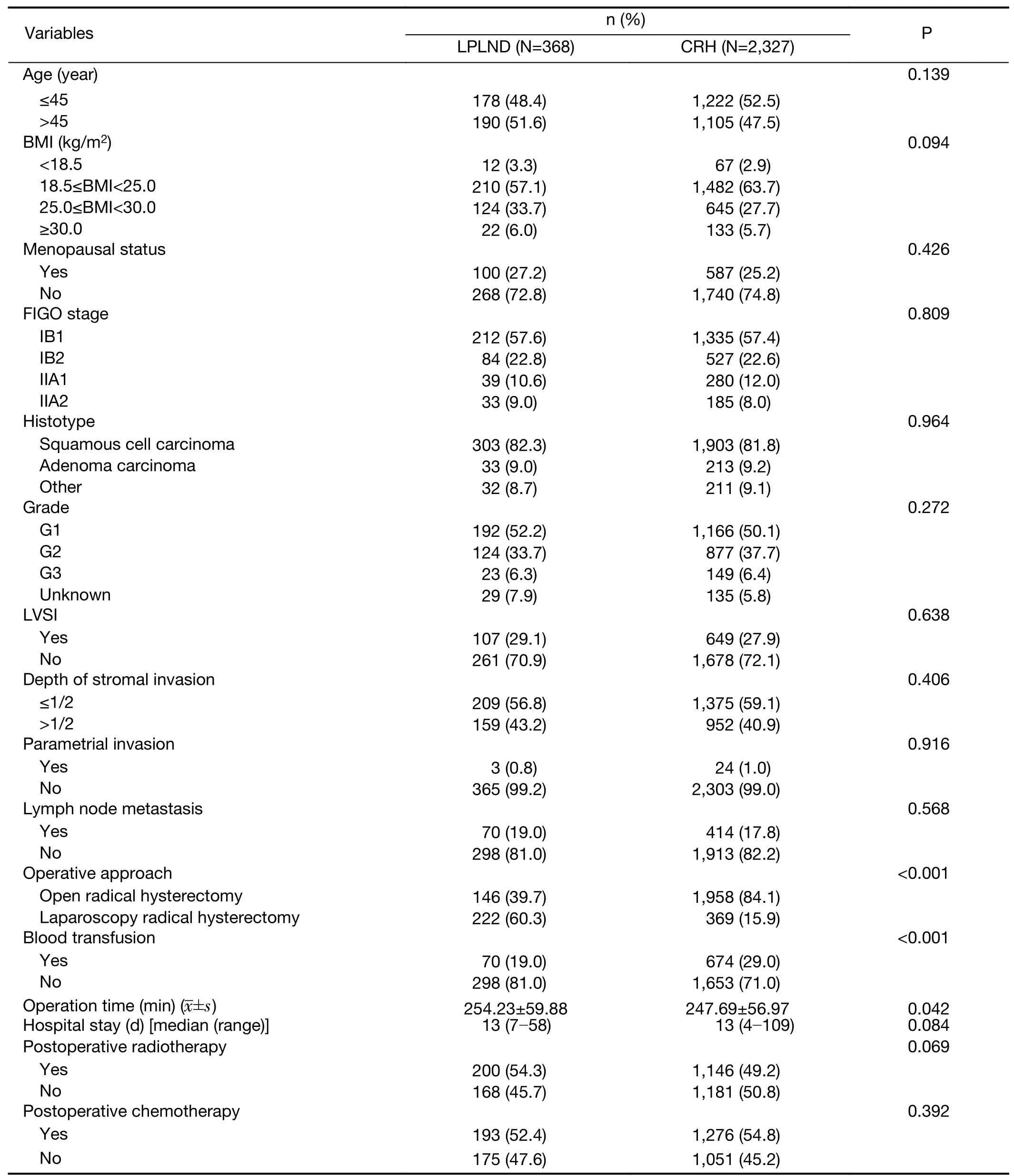
Table 1 Clinical and pathological characteristics of enrolled patients (N=2,695)
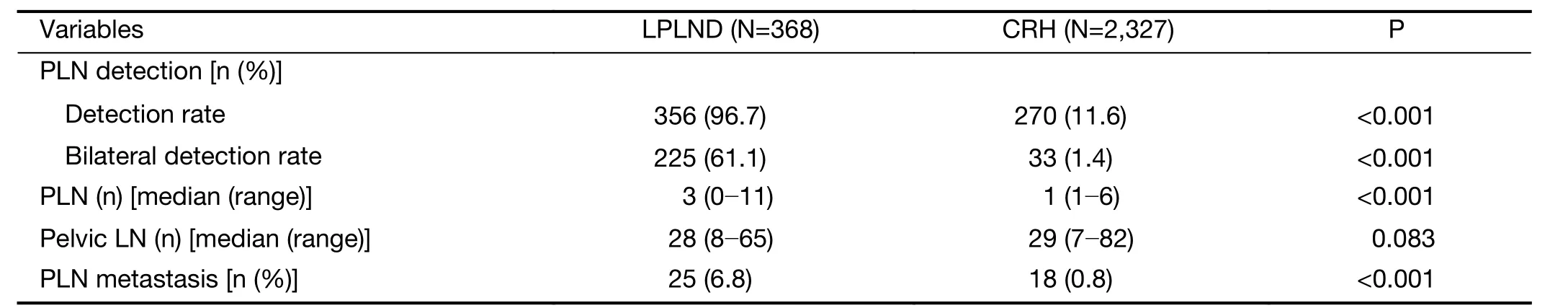
Table 2 Comparison of PLN detection between LPLND and CRH groups
In present study,all the slices were cross-validated by two pathologists.Even so,the detection rate of PLN in CRH group was 11.6%,which was significantly lower than that in the LPLND group.The result indicated that if PLNs were not resected separately,the detection rate of PLNs would be significantly decreased.Lanowskaet al.(19) reported that the detection rate of PLN for cervical cancer was only 7.1%.The PLNs diameter found in this study was between 1-3 mm.PLNs have a small volume and are typically removed along with parametrial tissues during extensive resection of uterus in the CRH.These nodes are also easily overlooked by pathologist palpation in routine pathological examination.Therefore,the PLNs detection rate is lower in some reported studies (12,13,20).
Several studies have effectively improved the detection rate of PLNs to 59%-93%,using the “giant section”pathological technique (12-14).The surgical specimens including the cervix and adjacent parametrial tissues were processed in whole and made into giant sections for pathologic evaluation.Giant sections provided the“panoramic” information regarding not only the distribution of PLNs,but also the lymphatic metastasis within parametrium.Girardiet al.(12) firstly introduced the “giant section” technique and reported that PLNs were present in 78% patients in their study.The study also described the PLNs scattered in the lateral parametrium from cervix to the pelvic wall.In the LPLND group of our study,we dissected all the PLNs above motioned.The median number of removed PLNs was 3,which was consistent with the report by Girardiet al(21).In another“giant section” study,Benedetti-Paniciet al.(14)performed a thorough three-dimensional assessment of parametrial tissues from surgical specimens.The result showed that PLNs were detected in 93% of patients,with a median number of 5,suggesting that these PLNs are present in nearly all females.Benedetti-Paniciet al.also demonstrated that most of PLNs locate in the lateral parametrium (cardinal ligament),and a small portion ofPLNs are distributed in vesicocervical ligament and uteroesacral ligament.In our study,the main PLNs in the lateral parametrium were completely resected by LPLND,but it was technically impossible to remove the rest of PLNs in vesicocervical ligament and uteroesacral ligament.Thus,these PLNs left on the surgical specimen of uterus still need to be carefully detected by pathologists,when“giant section” technique is not available as routine.In the LPLND group of this study,52 cases had PLNs detected from surgical specimens by pathologists.
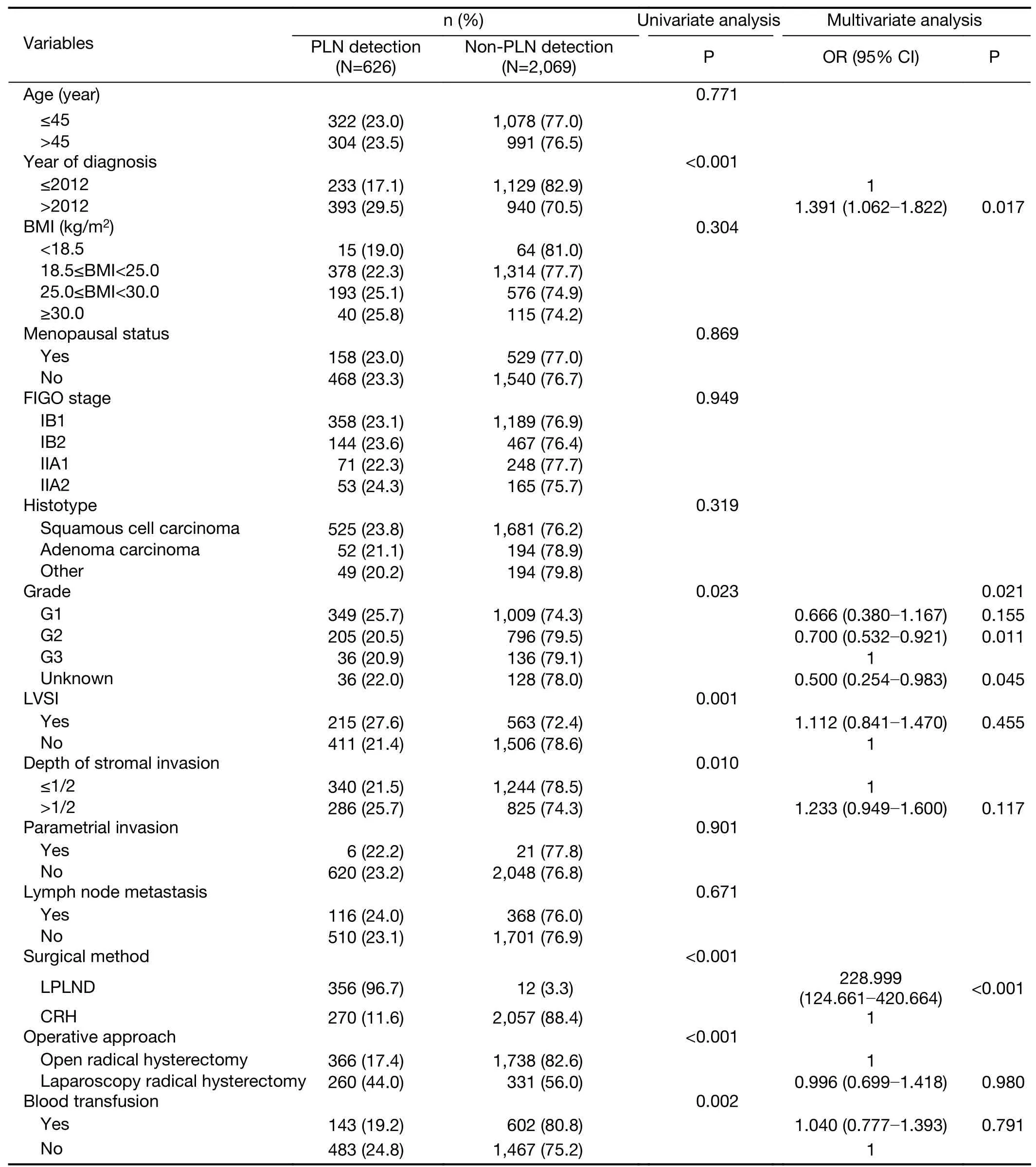
Table 3 Independent factors of PLN detection according to univariate and multivariate analysis
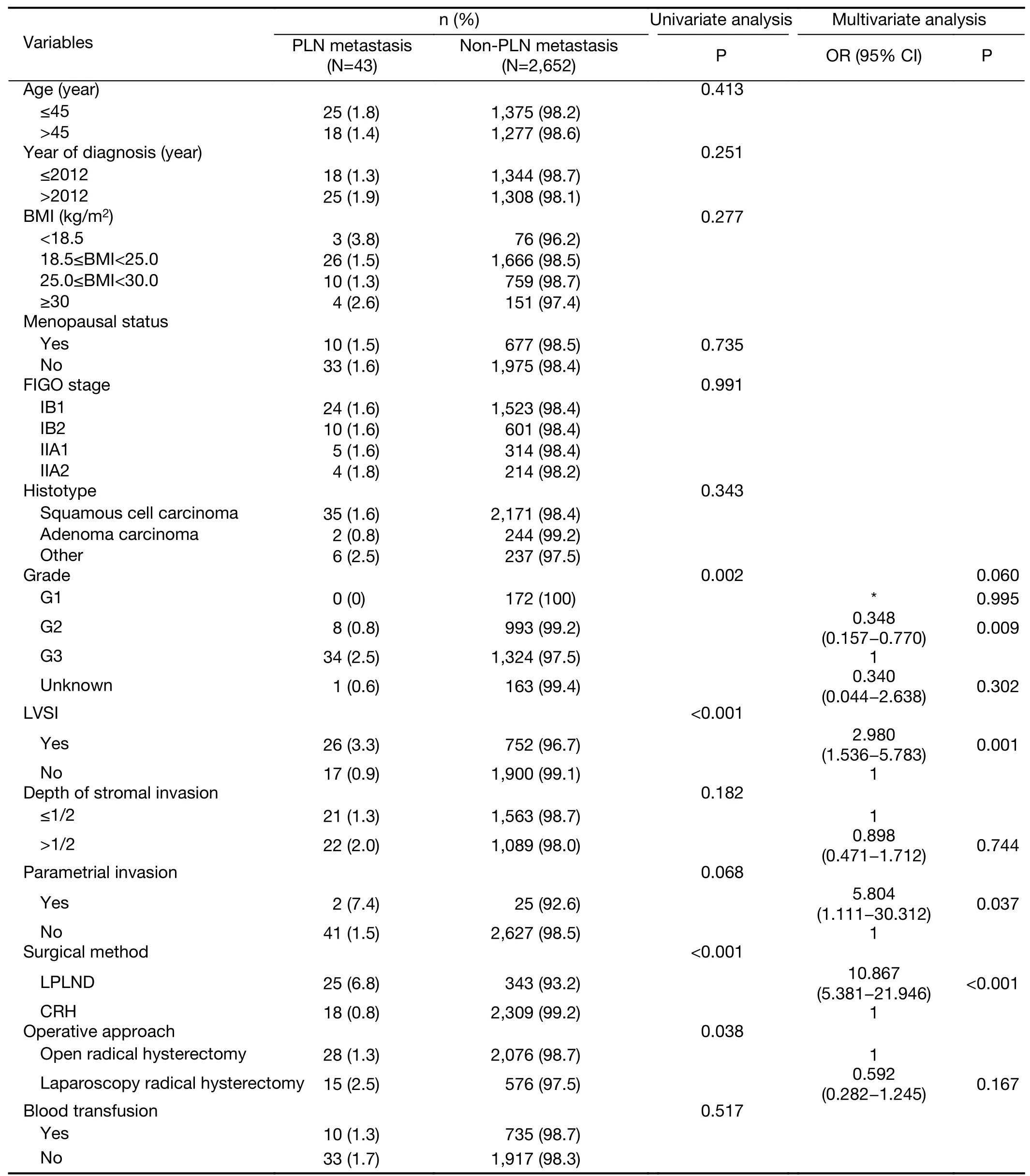
Table 4 Independent factors of PLN metastasis according to univariate and multivariate analysis
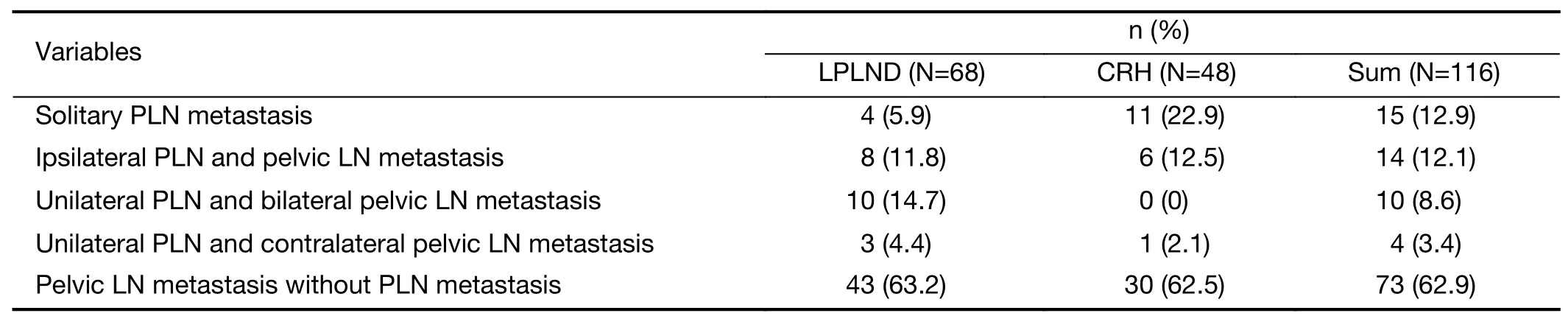
Table 5 Distribution of lymph node metastasis in patients with detected PLNs
Parametrial involvement is an independent prognostic factor for patients with early stage cervical cancer.Two patterns of the parametrial involvement have been stated in the literatures,which are direct tumor invasion and PLN metastasis (14,20).Our study also confirmed that direct tumor invasion was closely related to PLN metastasis by multivariate analysis.Van den Tillaartet al.(20)demonstrated that PLN metastasis was dominant,which accounted for 79% of all parametrial invasion.Therefore,accurate detection of PLN metastasis is crucial for prognostic evaluation.In two “giant section” studies,Girardiet al.(12) and Benedetti-Paniciet al.(14) reported that PLN metastasis rates in early-cervical cancer were 11.4 % and 12%,respectively,and more than 80% of metastatic PLNs were less than 10 mm in diameter (12,13).This truly reflects the characteristics of PLN metastasis.Using routine pathological examination,Steedet al.(22)and Vraneset al.(23) found that metastasis rates of PLNs of early-stage cervical cancer were only 0.97% and 1.3%,respectively.Similarly,only 0.8% of patients in our CRH group were found PLNs metastases.But,PLN metastasis rate was significantly improved to 6.8% in our LPLND group.Moreover,multivariate analysis showed that LPLND method was the critical independent factor for the detection of PLN metastasis.The results confirmed that PLNs metastases can be effectively identified by isolated resection of PLNs.
According to the classic theory proposed by Plentl and Friedman (11),the lymphatic drainage of cervical cancer runs through three channels from the cervix to pelvic lymph nodes.The anterior channel runs through the vesicocervical ligament,the lateral channel runs the lateral parametrium,and the posterior channel runs through the uterosacral ligament.Benedetti-Paniciet al.(14) found PLNs distributing on all three pathways above mentioned in their “giant section” study,and those patients with pelvic lymph node metastasis all had PLN metastasis.Accordingly,Benedetti-Paniciet al.believed that the path of tumor metastasis is first passing through the PLNs closest to the cervix before reaching the pelvic lymph nodes.Some studies supported this viewpoint by finding that patients have isolated PLN metastasis alone (24-27).Although there were 15 cases with isolated PLN metastasis in the current study,pelvic lymph node metastasis without PLN metastasis was more common.It was reported that obturator is the most common region of lymphatic metastasis in early cervical cancer (28).Those “giant section” studies also confirmed the metastasis rate of obturator lymph nodes is significantly higher than that of PLNs (13,25).In addition,as a midline organ,the uterus has bilateral lymphatic drainage.But the detection rate of bilateral PLNs in LPLND group of our study was 61.1%,suggesting that PLNs may be omitted due to the detection failure.It was reported that tiny PLNs with micrometastasis could only be detected though serial sectioning pathological examination,rather than conventional pathological methods (26).It was also argued that PLNs did not exist symmetrically,and tumors could directly metastasize to the pelvis through “bypass” lymph vessels without stepwise passing certain PLNs (29,30).A novel technique,sentinel lymph node mapping,might provide a more accurate method for detection of PLN metastasis,which can be used as supplement to LPLND in the future.
Conclusions
LPLND is easy to practice and could significantly improve the detection of PLN,thereby avoids omission of PLN metastasis in patients with operable early-stage cervical cancer.The limitation of the study is the retrospective nature which could produce bias.Even so,it is worth to conduct prospective study in the future to assess the efficacy of LPLND.
Acknowledgements
This study was supported by special fund for “Capital City Clinical Specific Application Study” (No.Z1711000010 17115).
Footnote
Conflicts of Interest:The authors have no conflicts of interest to declare.
 Chinese Journal of Cancer Research2020年6期
Chinese Journal of Cancer Research2020年6期
- Chinese Journal of Cancer Research的其它文章
- Hyperthermic intraperitoneal chemotherapy for gastric cancer with peritoneal metastasis:A multicenter propensity scorematched cohort study
- Development and validation of prognostic nomogram based on log odds of positive lymph nodes for patients with gastric signet ring cell carcinoma
- Prognostic factors affecting long-term outcomes in patients with brain metastasis from esophageal carcinoma
- Signatures within esophageal microbiota with progression of esophageal squamous cell carcinoma
- Oral microbiome and risk of malignant esophageal lesions in a high-risk area of China:A nested case-control study
- Current epidemiology of pancreatic cancer:Challenges and opportunities
