Thoracic imaging outcomes in COVID-19 survivors
Jaber S Alqahtani, Saeed M Alghamdi, Abdulelah M Aldhahir, Malik Althobiani, Reynie Purnama Raya, Tope Oyelade
Jaber S Alqahtani, Department of Respiratory Care, Prince Sultan Military College of Health Sciences, Dammam 3431, Saudi Arabia
Jaber S Alqahtani, Malik Althobiani, Department of Respiratory Medicine, Division of Medicine,University College London, London NW3 2PF, United Kingdom
Saeed M Alghamdi, Faculty of Applied Medical Sciences, Umm Al-Qura University, Makkah 21990, Saudi Arabia
Abdulelah M Aldhahir, Respiratory Care Department, Faculty of Applied Medical Sciences,Jazan University, Jazan 4514, Saudi Arabia
Malik Althobiani, Department of Respiratory Therapy, King Abdulaziz University, Jeddah 21589, Saudi Arabia
Reynie Purnama Raya, Faculty of Science, Universitas 'Aisyiyah Bandung, Bandung 40264,Indonesia
Reynie Purnama Raya, Institute for Global Health, Division of Medicine, University College London, London NW3 2PF, United Kingdom
Tope Oyelade, Institute for Liver and Digestive Health, Division of Medicine, University College London, London NW3 2PF, United Kingdom
Abstract The coronavirus disease 2019 (COVID-19) pandemic presents a significant global public health challenge. One in five individuals with COVID-19 presents with symptoms that last for weeks after hospital discharge, a condition termed “l(fā)ong COVID”. Thus, efficient follow-up of patients is needed to assess the resolution of lung pathologies and systemic involvement. Thoracic imaging is multimodal and involves using different forms of waves to produce images of the organs within the thorax. In general, it includes chest X-ray, computed tomography, lung ultrasound and magnetic resonance imaging techniques. Such modalities have been useful in the diagnosis and prognosis of COVID-19. These tools have also allowed for the follow-up and assessment of long COVID. This review provides insights on the effectiveness of thoracic imaging techniques in the follow-up of COVID-19 survivors who had long COVID.
Key Words: Long COVID; COVID-19; SARS-CoV-2; Thoracic imaging; Computed tomography; Survivors; Chest X-ray; Lung ultrasound
INTRODUCTION
The global coronavirus disease 2019 (COVID-19) pandemic continues to cause significant morbidity and mortality worldwide[1-3]. To date, the focus of research communication has been on the management of acute respiratory complications,particularly in critically ill patients[4,5]. However, since June 2020 increased attention has been paid to the experiences of COVID-19 survivors whose symptoms continue for four or more weeks[6]. According to the Office for National Statistics, one in five individuals has symptoms that continue after five weeks, and one in ten has symptoms for 12 wk or longer after acute infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)[7]. This is called “l(fā)ong COVID” and is defined as a condition in which infected people do not fully recover for several weeks or months after signs indicative of SARS-CoV-2 infection[8]. Studies on long COVID exploring the underlying pathology and sequelae, as well as rehabilitation for patients,are increasing. Data shows that many patients with long COVID develop serious clinical complications[9-11] and require follow-up to confirm full resolution of symptoms.
An imaging test refers to the generation of image results that are clinically relevant for clinical diagnosis, guiding management, triage, and therapy. Chest radiography,computed tomography (CT), lung ultrasound (LUS), and magnetic resonance imaging(MRI) provide additional clinical insights on COVID-19 patients to better understand long COVID complications. Early and accurate diagnosis, as well as guided management of COVID-19-related complications, is important[12]. Further, because of the tendency toward extended sequelae of COVID-19 symptoms, some of which include multi-organ involvement, there is an increasing need to develop follow-up strategies to prevent further deterioration of patients. Therefore, this review provides an update on the effectiveness of thoracic imaging techniques in the follow-up of COVID-19 survivors who suffer from long COVID.
THE USE OF THORACIC IMAGING IN COVID-19 PATIENTS
Using diagnostic thoracic imaging techniques on patients diagnosed with COVID-19 can sometimes be challenging due to the strict infection control measures that are required to prevent or reduce the spread of infection to healthcare providers and other patients[13]. However, various imaging modalities have been used due to the value of thoracic imaging in detection and monitoring of disease progression. Generally, chest radiography and CT of the chest are used with COVID-19, while the use of MRI and LUS is limited in the literature[14].
In the early stages of COVID-19 infection, chest radiography is insensitive especially in mild cases[15], whereas CT is more sensitive for early parenchymal lung disease,disease progression, and alternative diagnoses, including acute heart failure[16].Nevertheless, concerning the importance of chest radiography or CT for diagnosing viral pneumonia, experiences and decisions vary widely based on cultural standards and public health recommendations[17]. This is exemplified in China where patients are encouraged to present themselves early in the course of their disease when chest radiography has limited clinical value. CT has therefore proved a more efficient tool in detecting COVID-19 and guiding public health measures such as self-isolation[16]. In contrast, patients in the US have been instructed to stay at home until they suffer severe symptoms and so, as expected, a chest radiograph is generally abnormal at the time of presentation. In some countries, chest radiography is preferred in certain groups of patients because of portability; therefore, imaging can be performed in an infected patient’s isolation room, thus reducing the risk of SARS-CoV-2 transmission that may result from in-hospital transportation[17]. Although chest radiography can be beneficial for evaluating disease progress and alternative diagnoses, many hospitals rely on CT scan findings when clinical management decisions are needed, such as discharge from hospital or the need for intensive care unit[18]. Generally, the choice of thoracic imaging will depend on available equipment (chest radiography, CT, MRI or LUS), expertise, and the judgment of the healthcare staff at the points of care, with the final decision based on appropriate and reasonable assessment of related risks.
CHEST RADIOGRAPHY IN COVID-19 SURVIVORS
Chest radiography, also referred to as chest X-ray (CXR), involves using short wavelength electromagnetic radiation to produce images of the chest’s internal organs.With moderate ease of use and interpretation and low side effects, CXR remains one of the oldest and most used non-invasive chest imaging techniques[19]. However, in the context of COVID-19, the use of CXR has been reported to vary in importance and usefulness in both diagnosis and prognostication of disease course. Common CXR findings that have been described in COVID-19 patients are pulmonary lesions associated with inflammatory injuries, ground-glass opacity (GGO), linear opacity consolidation, crazy-paving pattern and vacuolar sign[20].
GGO remains the major structural change indicative of COVID-19 infection, with a majority of patients developing bilateral CXR findings of this nature[21,22]. A combination of GGO and consolidation of the lung image usually occurs in the periphery of the lung[23] and is scored from 0-4 based on the percentage of the lung affected[24]. In a study by Wong[15], the sensitivity of baseline CXRs in the diagnosis of COVID-19 was 62%, with 9% of patients showing abnormal CT findings before reverse transcription polymerase chain reaction (RT-PCR) confirmation of SARS-CoV-2 infection. A significant majority of patients with COVID-19 infection show CXR abnormalities indicative of damage to the lung tissue, which is attributable to systemic inflammatory response syndrome[22,25].
In most patients who survive severe COVID-19, there is a significant tendency to develop fibrotic lung tissue after recovery. However, while CRX is promising in diagnosing COVID-19, its use as a marker for pulmonary tissue recovery in patients with long COVID-19 remains unclear. For instance, in a study assessing 119 COVID-19 patients, D’cruz[26] found that follow-up CRX did not correlate with abnormal CT findings or prolonged functional disability in infected patients, while another study involving 134 patients concluded that CXR findings were an independent risk factor for poorer prognosis in COVID-19 patients[20]. Liao[22], in another study of 172 COVID-19 survivors, showed that 86% of patients had abnormal CT findings three months after discharge. In this study, change in CXR findings was associated with recovery duration, and abnormal lung findings were reported to correlate significantly with severity of COVID-19. Generally, the effectiveness of CXR as a prognostic marker or in tracking lung tissue regeneration in patients with long COVID remains uncertain.
CT IN COVID-19 SURVIVORS
CT scans have been extensively used in the diagnosis of COVID-19. In a series of 51 patients, the sensitivity of CT scan in detecting SARS-CoV-2 infection was reported to be higher (98%) compared to RT-PCR (71%)[27,28]. In another study involving 167 patients considered at high risk for SARS-CoV-2 infection, chest CT scan confirming viral pneumonia correlated significantly with positive RT-PCR results[29]. Generally,chest CT findings of lung tissue pathology are similar to those of CXR scans in COVID-19 and are scored based on bilateral lung involvement, including GGO, consolidation,vacuolar sign, linear opacity and crazy-paving pattern[30,31]. However, while the sensitivity of CT is high in detecting lung tissue pathology associated with pneumonic infections, the specificity for SARS-CoV-2 infection is relatively low (25%-56%)[31].
Because of its sensitivity, the first point of call and the reference technique for chest imaging has been CT. Although CT is expensive, less portable and available, and requires well-trained and experienced radiographers for standard operation and interpretation of findings[32], it has been extensively used in the prognosis and followup of COVID-19 patients. In a study involving 55 COVID-19 survivors followed up for three months after discharge, abnormal CT findings were detected in 71% of patients[33]. Another study in which final CT scans were obtained from 70 COVID-19 survivors at discharge showed unresolved lung tissue pathology in 94% of the patients, mainly in the form of residual GGO (60%)[34]. Tabatabaei[35] studied 52 patients who had recovered from COVID-19 and reported residual CT abnormalities in 42% of the survivors. These findings showed significant correlation with disease severity. Generally, CT is a useful and more sensitive tool in the follow-up of patients recovered from COVID-19. It may be helpful in the assessment of treatment effects.
LUS IN COVID-19 SURVIVORS
LUS provides a faster, safer and more sensitive assessment of lung tissue pathology compared to radiation-based CXR and has been extensively used in the monitoring of patients with COVID-19. LUS is also relatively more accessible because of the inherent portability and bedside availability, making it a technique of choice where timely assessment of lung complications is needed, especially in COVID-19 patients with severe or unstable health conditions[36]. Further, the ability to delineate alterations in superficial lung tissue through the air and tissue ratio (using A- and B-lines) makes LUS unique and more sensitive in characterizing the nature, topography, and size of lung tissue lesions[37,38]. In general, irregular thickening of the pleural line, heterogeneous B-lines and consolidations, pleural effusions, and recovery-phase A-lines in the lung image have been detected in COVID-19 patients using ultrasonography[39-41]. LUS has been reported to correlate strongly with systemic inflammation and severity of COVID-19, although not with survival[42].
In the follow-up of COVID-19 survivors with long-persisting symptoms, LUS findings have shown promising outcomes. In a case series of long COVID patients by Tung-Chen[43], LUS findings correlated with chest CT and accurately assessed the resolution of residual lung tissue abnormalities. LUS findings, specifically the frequency of B-lines, which measures the thickening of pleural lines, were also reported to correlate with the duration of COVID-19 symptoms in patients[44].Further, LUS was successfully used in the assessment of the progression of COVID-19 in a 35-year-old survivor for up to three weeks in a home setting[45]. These highlights both the sensitivity and availability of LUS for the assessment of both short- and longterm effects of SARS-CoV-2 infection.
MRI IN COVID-19 SURVIVORS
MRI was first introduced in the United Kingdom in 1980, and since that time, it has become widely used in clinical practice[46,47]. It is extremely effective, particularly in the diagnosis of patients without exposing them to dangerous ionising radiation[48].Angiotensin-converting enzyme 2 (ACE2) is the path for SARS-CoV-2 to attack thoracic organs, including lung and cardiac systems. MRI has been used regularly to assess cardiac involvement in patients who have recovered from COVID-19[11,49].Huang[49] conducted a study on patients who reported cardiac symptoms during their hospitalization due to COVID-19 to assess whether there was continued cardiac involvement after the patients’ recovery from COVID-19. This study found that 58% of the recovered patients had abnormal MRI findings, including myocardial oedema(54%) and late gadolinium enhancement (31%). Further, fibrosis and compromised right ventricle function have also been found in patients who have recovered from COVID-19. In another study conducted by Puntmann[11], independent of preexisting comorbidities, severity and overall course of the acute illness, cardiac involvement was reported in 78% of patients and around 60% had ongoing myocardialinflammation. The abnormal findings included elevated myocardial native T1 and myocardial native T2 and pericardial enhancement. Cardiac involvement in patients recovered from COVID-19 is common and has the potential to affect the overall prognosis. Although rarely used, MRI is effective in detecting cardiac involvement in patients and provides a holistic diagnostic assessment of residual symptoms in COVID-19 survivors. Further studies are essential to explore the long-term cardiopulmonary burden of long COVID.
In summary, Table 1 shows the major findings of thoracic imaging tools in COVID-19 survivors.
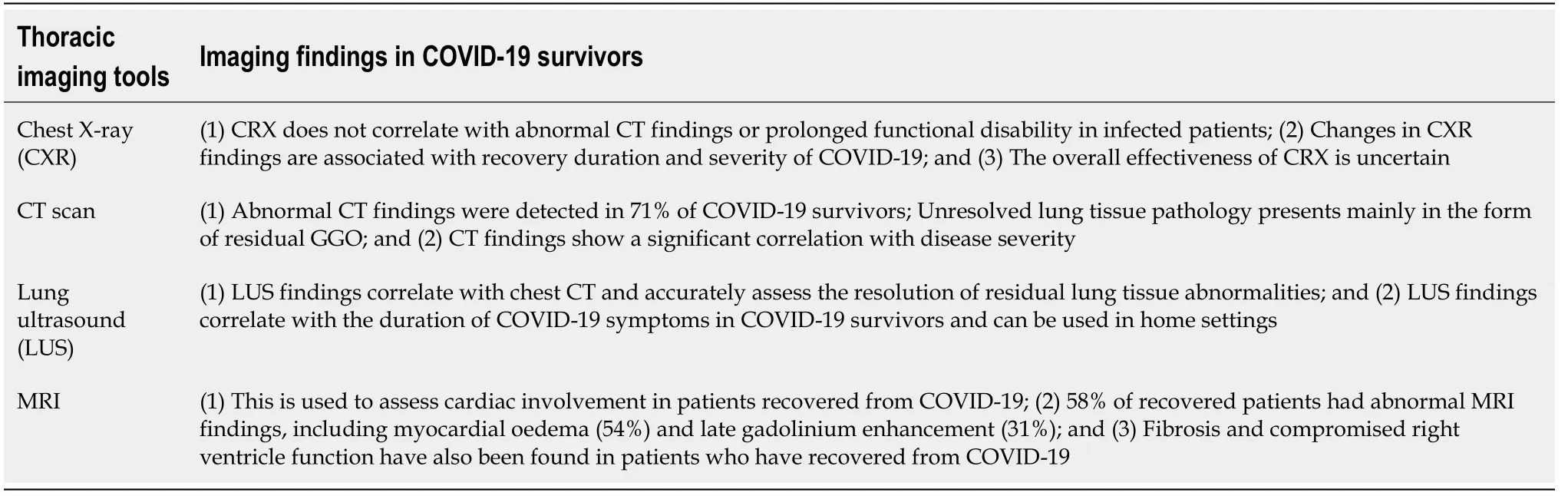
Table 1 Findings of thoracic imaging tools in coronavirus disease 2019 survivors
KEY POINTS
(1) COVID-19 survivors sometimes develop long-term sequelae, generally termed“l(fā)ong COVID”, which can be assessed by different imaging tests; (2) Various imaging modes have been used as diagnostic, prognostic, and follow-up tools in COVID-19.However, sensitivity and specificity, as well as modes and ease of use, vary; (3) The effectiveness of CRX as a prognostic marker or in tracking lung tissue regeneration in patients with long COVID remains uncertain; (4) CT is a relatively more sensitive tool in the follow up of COVID-19 survivors and could be used for the assessment of treatment effects; (5) LUS is sensitive and relatively more portable than radiologybased imaging tools, allowing for use in out-of-hospital settings, and it may be the best tool for the follow-up of COVID-19 survivors; and (6) Although rarely used, MRI is effective in detecting cardiac involvement in patients and provides a holistic diagnostic assessment of residual symptoms in COVID-19 survivors.
CONCLUSION
COVID-19 survivors, especially those with a severe clinical course, have residual lung tissue abnormalities and suffer extensive sequelae, currently termed “l(fā)ong COVID”.Fibrotic lung tissue from systemic inflammatory response to SARS-CoV-2 infection is characteristic of severe COVID-19 and can be picked up in follow-up scans. Various imaging techniques have been extensively used for the follow-up of long COVID,including CXR, CT, LUS and MRI with varying efficiency. However, CT remains the most commonly used because of its sensitivity, while LUS is favoured because of its accessibility and portability.