The neutrophil-tolymphocyte ratio at the prostate-specific antigen nadir predicts the time to castration-resistant prostate cancer
Dear editor,
With the spread of prostate-specific antigen (PSA)screening,an increasing number of early-stage prostate cancers have been diagnosed recently,although many patients are still diagnosed in the advanced stage [1].Although most prostate cancers with metastatic lesions respond to initial androgen ablation therapy,responders ultimately develop progressive disease due to hormonerefractory cancer.Recent studies have shown the efficacy of initial docetaxel or abiraterone acetate with predonine in metastatic hormone-sensitive prostate cancer (mHSPC)[2].However,not all mHSPC patients experience efficacy with this up-front initial treatment.These previous studies have therefore underscored the importance of assessing the risk of castration-resistant prostate cancer (CRPC) in mHSPC patients.
A recent study reported that the neutrophil-to-lymphocyte ratio(NLR)was an independent prognostic factor in some solid malignancies,including prostate cancer [1].A recent study revealed the usefulness of the NLR for prostate cancer patients who were candidates for active surveillance [3].Our previous study also showed that the group with a higher NLR showed a poorer recurrence-free and overall survival in mHSPC.Although these reports showed the importance of properly assessing prognostic factors,they did not investigate the NLR values in the course of cancer therapy.The present study was the first to examine the NLR over the course of treatment in the same mHSPC patient cohort:When they were first diagnosed,when the PSA level was at its nadir,and when they developed CRPC status.
We retrospectively reviewed 46 consecutive patients with initially diagnosed metastatic prostate cancer from 2004 to 2016,at Yokohama City University Medical Center(Yokohama,Japan) and Yokohama City University Graduate School of Medicine(Yokohama,Japan).All patients were administered androgen deprivation therapy (ADT).None of the patients received up-front docetaxel or up-front abiraterone therapy.The PSA nadir was determined as the time when the patients’PSA level was lowest after ADT.The CRPC day was determined as the time when the PSA level was its nadir value +2 ng/mL or when the drug regimen was changed.This study was carried out in accordance with the ethical standards of the Declaration of Helsinki.The review board of Yokohama City University(D15060003)approved this study.
A total of 138 patients with initially diagnosed metastatic prostate cancer were enrolled in this study.Of these patients,46 had available data for their NLR over the course of prostate cancer treatment (Supplementary Table 1).The median values were used as the cut-off points for the NLR.The higher NLR group (≥1.73 at the time of PSA nadir)showed a significantly longer time from the initial diagnosis to CRPC as well as from the PSA nadir to CRPC than the lower NLR group (<1.73 at the time of PSA nadir) (p
=0.042 andp
=0.046,respectively) (Fig.1A and 1B).The NLR at the time of PSA nadir was significantly lower than that at the diagnosis (p
<0.001),and the PSA values were remeasured at the time of CRPC (p
=0.008)(Fig.1C).In addition,a high NLR at the time of the PSA nadir was an independent risk factor for a short time to CPRC (Supplementary Table 2).We therefore speculated that the NLR was correlated with prostate cancer aggressiveness.While the detailed mechanisms remain unclear,one candidate mechanism underlying this relationship is that a lower lymphocyte count reduces the immunoreactivity and thereby results in cancer progression [4].Though tumor invasive dendric cells induced acquired immunity and suppressed tumor progression,transforming growth factor(TGF)-beta and prostaglandin E2 (PGE2) changed the dendric cells and induced regulatory T cells (regT) [5].RegT suppresses cancer antigen-specific T cells,resulting in a decreased number of lymphocytes [6].Some cancers induce chemocytokine induced cytokines progressed cancer development.These previous findings suggest that increased neutrophil counts and the suppression of lymphocytes are associated with an increased NLR.A higher NLR reflects both progression of cancer and the suppression of anti-cancerous activity.
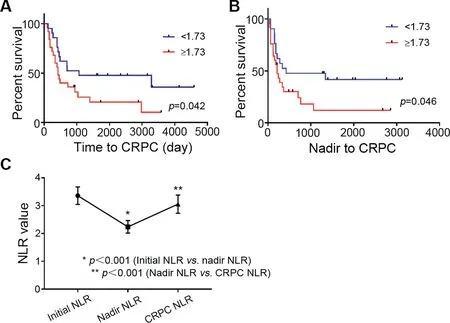
Figure 1 The results of neutrophil-to-lymphocyte ratio(NLR)and prostate-specific antigen (PSA) in castration-resistant prostate cancer(CRPC)and NLR group.(A)The lower NLR value group (<1.73) showed a longer time from the initial diagnosis to CRPC than the higher NLR group(≥1.73)(median time:1067 vs.426 days,p=0.042);(B)The lower NLR value group(<1.73)showed a longer time from the PSA nadir to CRPC than the higher NLR group (≥1.73) (median time:426 vs. 215 days,p=0.046);(C)The NLRs at the time of the diagnosis,PSA nadir,and CRPC were 3.36±1.77,2.24±1.27,and 3.06±1.85,respectively.The NLR at the time of the PSA nadir was significantly lower than the NLR at the diagnosis (p<0.001) but increased again by the point of CRPC (p=0.008).
The NLR is thought to be an important prognosis predictive marker for advanced disease or CRPC.Previous reports [7—9] discussed that NLR is easily calculated and no additional costs are required and widely used in urological field.Furthermore,an increased NLR has been shown to be associated with a worse overall,cancer specific survival,and recurrence-free survival [10].However,despite these previous findings concerning the importance of the NLR,no previous study has described the changes in the NLR induced by cancer therapy.The present study showed that the NLR was correlated with prostate cancer progression in metastatic prostate cancer patients who developed CRPC.
Author contributions
Study design
:Genta Iwamoto,Takashi Kawahara.Data acquisition
:Genta Iwamoto,Takashi Kawahara,Yumiko Yokomizo,Yasuhide Miyoshi,Hiroji Uemura.Data analysis
:Genta Iwamoto,Takashi Kawahara.Drafting of manuscript
:Genta Iwamoto,Takashi Kawahara.Critical revision of the manuscript
:Masahiro Yao.Conflicts of interest
The authors declare no conflict of interest.
Appendix A.Supplementary data
Supplementary data to this article can be found online at
https://doi.org/10.1016/j.ajur.2020.05.006.
 Asian Journal of Urology2021年3期
Asian Journal of Urology2021年3期
- Asian Journal of Urology的其它文章
- Testing for BRCA1/2 and ataxiatelangiectasia mutated in men with high prostate indices:An approach to reducing prostate cancer mortality in Asia and Africa
- Male genital damage in COVID-19 patients:Are available data relevant?
- A comparison of artificial urinary sphincter outcomes after primary implantation and first revision surgery
- Augmented anastomotic urethroplasty with buccal mucosa for post penile fracture urethral injury long segment bulbar urethral stricture review
- Conquering new battlegrounds:Successful management of isolated giant retrovesical hydatid cyst with robotic assistance
- A systematic review of dedicated models of care for emergency urological patients
