Endoscopic management of intramural spontaneous duodenal hematoma: A case report
Giorgio Valeri, Vittorio Maria Ormando, Carlo Cellini, Luca Sacco, Carmelo Barbera
Abstract
Key Words: Duodenal hematoma; Several pancreatic diseases; Endoscopy complication;AXIOS? stent; Case report
INTRODUCTION
Intramural duodenal hematoma (IDH) is a rare intestinal condition described for the first time at autopsy in 1838 [1 ], and the first source in the PubMed database accessing the MEDLINE database (http://www.ncbi.nlm.nih.gov/pubmed/) dates from 1952 [2 ].
This condition is usually associated with blunt abdominal trauma in children[3 ] and upper endoscopy procedures (duodenal biopsy or injection therapy for bleeding peptic ulcers) or various nontraumatic conditions in adults (> 70 % of cases). These include several pancreatic diseases even if the association remains unclear, such as certain coagulation disorders (anticoagulant therapy, haemophilia,Von Willebrand disease, Henoch-Sch?nlein purpura), malignancy, collagenosis, peptic ulcers and vasculitis[4 -7 ].
Clinical symptoms for IDH may vary from vague abdominal pain to acute abdomen, intestinal obstruction or gastrointestinal bleeding[3 ,8 ], and diagnosis is subsequently confirmed by magnetic resonance imaging or computed tomography (CT) and upper gastrointestinal endoscopy (UGIE).
Most IDH cases resolve spontaneously or with correction of abnormal coagulation. Percutaneous drainage or surgery may be needed in some refractory IDH cases, malignancy, perforation and intestinal tract obstruction.
Here we present the use of the innovative lumen apposing metal stent catheter (LAMS) Hot AXIOS?(Boston Scientific Corp., Marlborough, MA, United States) in the case of spontaneous IDH with intestinal substenosis, which was non-responsive to conservative management, in a patient without risk factors. This innovative device, with a lumen apposing self-expandable metal stent fitted onto an electrocautery-enhanced tip catheter, is safe and feasible in gallbladder drainage, choledochoduodenostomy and drainage of pancreatic fluid collections. In recent years, Hot AXIOS? has also been used for off-label indications including gastrojejunostomy, gastro-gastrostomy and drainage of postsurgical collections. Herein we report the use of Hot AXIOS? in the rare digestive disorder spontaneous IDH.
CASE PRESENTATION
Chief complaints
A 51 -year-old man was admitted to the hospital with abdominal pain, bloating and vomiting.
History of present illness
The clinical data suggested a diagnosis of intestinal obstruction.
History of past illness
The patient did not report comorbidities or recent abdominal trauma without relevant previous medical history and in particular without having taken anti-platelet medication.
Personal and family history
He did not have relevant family history.
Physical examination
Physical examination on admission revealed slight tenderness over the epigastric region and right flank.
Laboratory examinations
Initial biochemical analysis indicated neutrophilic leukocytosis (13 .07 × 109 /L) and an increased level of C-reactive protein without alterations of serum haemoglobin, D-dimer, platelet function and coagulation parameters.
Imaging examinations
A contrast-enhanced abdominal CT scan revealed an IDH (Figure 1 A). On admission UGIE and then endoscopic ultrasound (EUS) confirmed submucosal swelling of the second part of the duodenum that measured approximately 90 mm along the long axis with substenosis of the duodenal lumen(Figure 1 B).
MULTIDISCIPLINARY EXPERT CONSULTATION
A conservative approach was attempted with clinical observation and empirical antibiotic therapy. The patient was discharged in good clinical condition after 8 d of intravenous antibiotic therapy.
FINAL DIAGNOSIS
Intramural spontaneous duodenal hematoma.
TREATMENT
After 48 h the patient was readmitted to the hospital due to clinical relapse. Biochemical analysis indicated a significant increase of both leukocytosis and C-reactive protein, and the radiological evaluation confirmed the previous diagnosis. After 10 d a multidisciplinary evaluation was performed,and minimally invasive endoscopic treatment was proposed.
EUS-guided drainage was performed with the Hot AXIOS? system. A direct LAMS 15 mm × 10 mm was inserted into the submucosa lumen with an electrocautery-enhanced tip catheter and released under complete EUS control after the second flange was deployed in the duodenal lumen (Figure 2 A).UGIE control confirmed the correct LAMS placement, and hematinic material associated with slightly purulent drainage was observed (Figure 2 B).
OUTCOME AND FOLLOW-UP
A control CT scan demonstrated the presence of LAMS and the complete drainage of the intramural collection (Figure 2 C). The patient was discharged in good clinical condition after 7 d. After an additional 2 wk he repeated UGIE, which revealed a complete resolution of the duodenal bulging, and the LAMS was contextually removed with complete closure of the mucosal defect with a clip. At the 30 -d follow-up the patient was completely asymptomatic.
DISCUSSION
IDH is a rare condition usually caused by trauma, anticoagulant therapy, rupture of a duodenal aneurysm or biopsy[4 -7 ,9 ]. Rare cases of IDH have also been described as a consequence of acute pancreatitis[3 ] or after endoscopic retrograde cholangiopancreatography procedures[10 ].
CT and magnetic resonance imaging represent the most sensitive diagnostic exams for IDH.Radiological exams have a role both for diagnosis as well as follow-up of small bowel hematoma within 2 wk[11 ,12 ]. Once IDH is confirmed, conservative management with fasting and total parenteral nutrition should be given[13 ]. Traditionally, in the case of persistent IDH, surgical drainage[14 ,15 ] and percutaneous drainage were performed[16 ], both causing great trauma for the patient. The indications for surgical intervention are not well clarified, certainly in the case of occlusive symptoms over 7 -10 d or where there is evidence of perforation with a generalized peritonitis[17 ].
To date there are few described cases of endoscopic drainage of duodenal hematoma. This consists of endoscopic incision of the hematoma using a needle-knife or a biopsy forceps in order to obtain rapid submucosal decompression[18 ,19 ] with improvement of abnormal laboratory findings and abdominal pain in up to 1 wk. The persistence of duodenal ulcer at the site of endoscopic incision has also been described with a complete resolution only after 1 mo[18 ].
In our case we had a patient with an unremarkable previous medical history, with no risk factors for IDH who presented with intestinal pseudo-obstruction symptoms and leukocytosis without evidence of pancreatitis. We first attempted a conservative approach according to the existing data, but after recurrence of symptoms an endoscopic approach was proposed.
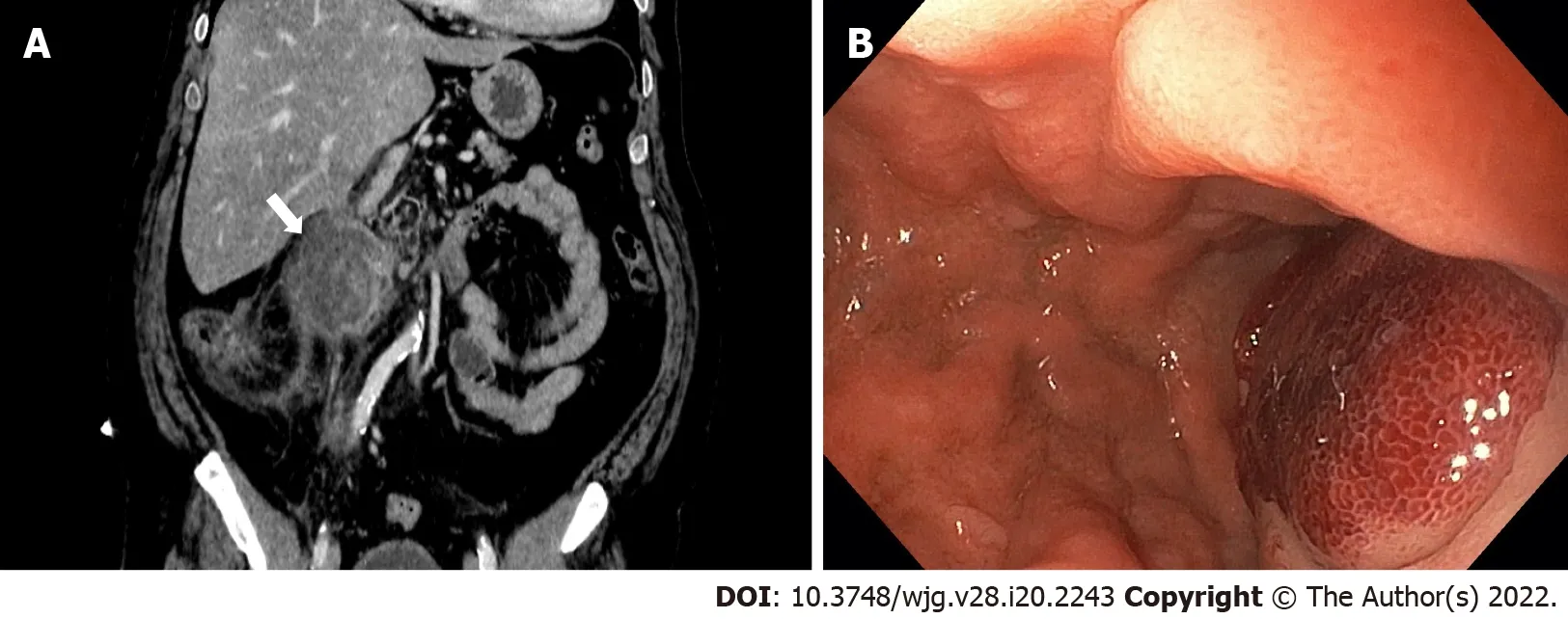
Figure 1 Intramural duodenal hematoma. A: Contrast-enhanced abdominal computed tomography in coronal section; B: Endoscopic visualization with substenosis of duodenal lumen.
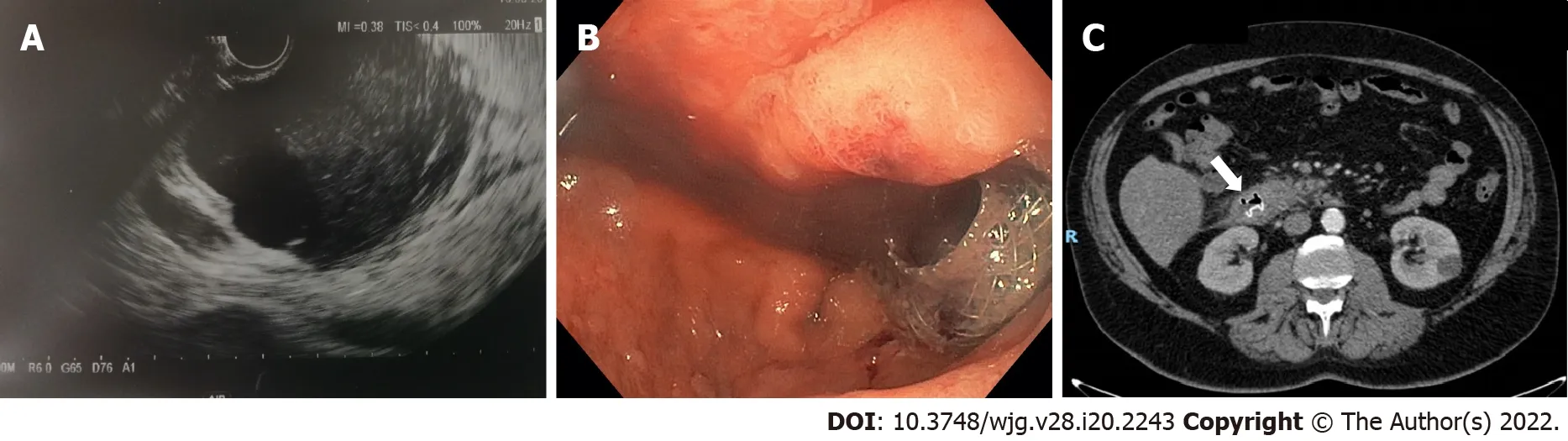
Figure 2 Intramural duodenal hematoma after endoscopic treatment. A: Endoscopic ultrasonography (EUS) image showed deployment of the distal flange of a cautery-tipped lumen apposing metal stent (LAMS) in the intramural duodenal hematoma under EUS guidance; B: Endoscopic views showed the proximal flange of the LAMS; C: Control abdominal computed tomography confirmed the correct position of the LAMS.
The Hot AXIOS? lumen-apposing stent is a novel double-flanged covered, self-expanding metal stent, safe and effective in gallbladder drainage, choledochoduodenostomy and drainage of pancreatic fluid collections. In the recent years, Hot AXIOS? stents have also been used for off-label indications including gastrojejunostomy, gastro-gastrostomy and drainage of postsurgical collections.
Here we present the use of Hot AXIOS? in a rare but possible digestive disorder with a rapid and complete resolution of this insidious clinical entity, as confirmed by CT scan and with only 7 d length of stay without abnormal laboratory findings and abdominal pain after the procedure.
CONCLUSION
In our experience Hot AXIOS? is a safe and effective endoscopic procedure for the treatment of IDH,reserved for patients who are not responsive to conservative management. However, it should be performed by expert endoscopists trained in EUS and radiological procedures. To reduce the rate of postoperative complications and improve clinical outcome a previous careful clinical evaluation focusing on coagulopathies is mandatory.
FOOTNOTES
Author contributions:All authors contributed to writing this case report.
Informed consent statement:Informed written consent was obtained from the patient for publication of this report and any accompanying images.
Conflict-of-interest statement:All authors declare no conflict of interest for this case report.
CARE Checklist (2016 ) statement: The authors have read the CARE Checklist (2016 ), and the manuscript was prepared and revised according to the CARE Checklist (2016 ).
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4 .0 ) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4 .0 /
Country/Territory of origin:Italy
ORCID number:Giorgio Valerii 0000 -0001 -8268 -2022 ; Vittorio Maria Ormando 0000 -0003 -4481 -755 X; Carlo Cellini 0000 -0001 -7210 -0439 ; Luca Sacco 0000 -0003 -1007 -9894 ; Carmelo Barbera 0000 -0002 -4051 -4976 .
S-Editor:Yan JP
L-Editor:Filipodia
P-Editor:Yan JP
 World Journal of Gastroenterology2022年20期
World Journal of Gastroenterology2022年20期
- World Journal of Gastroenterology的其它文章
- Future prospect of “Gut microbiome composition can predict the response to nivolumab in advanced hepatocellular carcinoma patients”
- First prospective European study for the feasibility and safety of magnetically controlled capsule endoscopy in gastric mucosal abnormalities
- Digital single-operator video cholangioscopy improves endoscopic management in patients with primary sclerosing cholangitis-a retrospective observational study
- Long noncoding RNA TNFRSF10 A-AS1 promotes colorectal cancer through upregulation of HuR
- Radiomics for the detection of microvascular invasion in hepatocellular carcinoma
- Gadolinium-ethoxybenzyl-diethylenetriamine penta-acetic acid-enhanced magnetic resonance imaging for evaluating fibrosis regression in chronic hepatitis C patients after direct-acting antiviral
