Radiological review of rhinocerebral mucormycosis cases during the COVID-19 Pandemic:A single-center experience
INTRODUCTION
Mucormycosis is caused by fungi belonging to the order
and class
[1].Fungal spores that are present in the air constitute a source of infection.However,these fungi rarely infect healthy individuals,as normal host defense mechanisms prevent invasion by these organisms.However,when host defense mechanisms are weakened due to several factors,such as congenital disorders,acquired immunodeficiency syndrome,hematological malignancies,uncontrolled systemic illnesses,and the use of immunosuppressive medication,these organisms invade and proliferate in human tissues.The incidence of mucormycosis has increased over the past few years due to the aging population,medical comorbidities,the increase in the incidence of malignancies,and the pandemic of human immunodeficiency virus infection[2].
The situation has worsened with the onset of the severe acute respiratory syndrome coronavirus 2 infections,which has led to the coronavirus disease 2019(COVID-19)pandemic that began in late 2019 and has continued till the present.The main pathogenesis of the complications of this viral infection is due to the excessive immunological response that leads to damage to host’s own tissues[3].This has resulted in the use of immunosuppressive medication in the form of corticosteroids,interleukin antagonists,and various antibodies to counter the inflammatory cytokines.These drugs have proved to be efficacious in dealing with the complications and cytokine storm of COVID-19.However,they come with serious side effects of immunosuppression.
And then she tucked up her little dress, that she might run faster, but the narcissus caught her by the leg as she was jumping over it; so she stopped and looked at the tall yellow flower, and said, “Perhaps you may know something.”
13. Great forest: The dark and mysterious forest is often a place of exile where psychological growth occurs. It symbolizes the unconscious, the realm of the psyche. It is often a threshold through which the soul encounters the perils of the unknown and survives as a wiser person. IRReturn to place in story.
The number of cases of mucormycosis has rapidly increased in the last few months.This rise is attributed to the use of immunosuppressive medication to treat COVID-19 infections[4].The paranasal sinuses and lungs,being the first spaces to come in contact with the fungus,are most commonly affected.Once the disease is established,it spreads to the surrounding structures,such as the orbit,brain,mediastinum,
.The overall mortality of mucormycosis is more than 50%,and the mortality rate for disseminated disease reaches 100%[5].The infection responds to only a few antifungals,such as amphotericin B,which are very toxic[5].
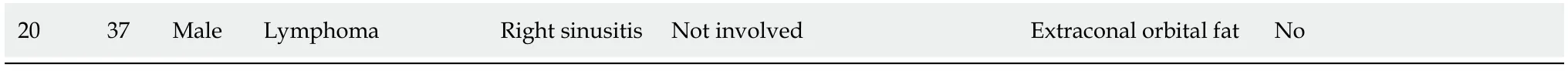
A total of 20 patients with rhinocerebral mucormycosis were studied.Eighteen patients had isolated rhino-cerebral mucormycosis,and two patients had combined pulmonary and rhino-cerebral mucormycosis(Table 1).Most study subjects were male patients(90%).The age distribution of the subjects is as follows:10% were between 20–30 years of age,20% were between 31–40 years of age,30% were between 41–50 years of age,5% were between 51–60 years of age,20% were between 61–70 years of age,and 15% were between 71–80 years of age.Most patients in the review had comorbidities(85%):20% had hematological malignancy,40% had diabetes,10% had acquired immunodeficiency syndrome,and 15% were transplant recipients on immunosuppressive medication.
Annie Mae was my in-law’s maid. She prepared and served meals in her quiet, gentle way and then returned to the kitchen to read her Bible while we ate. She was a dedicated3 and devoted4 Christian5. To me, she reflected the fruit of the Holy Spirit as found in Galatians 5:22-23. I found this increasingly true even though I came to know her more by observation than by conversation.
MATERIALS AND METHODS
We have retrospectively collected data on cases of mucormycosis diagnosed from April 2020 to April 2021 at our institute,which is a tertiary care center located in the state of Kerala,India.
All adult patients above the age of 18 years who were diagnosed with mucormycosis by imaging post–COVID-19 infection and confirmed by histopathological examination were studied.Patients with an unknown medical history,absent hospital records,and unknown outcomes were excluded from the review.
Hospital databases in the radiology department of our hospital were searched with the keyword “mucormycosis,” and results were obtained.A list of cases was obtained,which was filtered to include only those cases from April 2020 to April 2021.Hospital identification numbers were then used to trace the clinical details and outcomes of the patients.The demographic details of the patients were recorded,and the COVID-19 infection history and treatment history were noted.History of various comorbidities,including malignancies,was obtained from the hospital records.The findings of the CECT scans,which were obtained using a 128-slice dual-energy CT scanner(SOMATOM Definition Flash,Siemens,Germany),were reviewed by the same radiologist to ensure uniformity in reporting.Images were acquired with 1–3 mm collimation and a pitch of up to 2:1 to allow for coverage of the area of interest in a single breath-hold.
Imaging was repeated at one-month follow-up to study the lesions.
RESULTS
The authors of the present study have also come across many cases of mucormycosis in the last few months during the times of the COVID-19 pandemic.The following is a mini-review of the radiological findings of the rhinocerebral mucormycosis cases recorded by us in the last few months.
Sinuses were involved in all the cases.Unilateral involvement of the sinuses was more common than bilateral involvement.In most cases(35%),all four sinuses(maxillary,frontal,ethmoid,and sphenoid)were involved.The isolated maxillary sinus was involved in 20% of the cases.The isolated frontal sinus was involved in 5% of the cases.The ethmoid and sphenoid sinuses combined were involved in 10% of the cases.The frontal,ethmoid,and sphenoid sinuses combined were involved in 5% of the cases.
33.Change yourself into all sorts of creatures you have a mind to: Shapeshifting is a common motif in folklore and found in almost every culture around the world, often attributed to gods and mythical creatures, but sometimes practiced by humans.Return to place in story.
She knew it would so soon fade; so she took only a single greenleaf, carried it home, and laid it in her Bible, where it remainedever green, fresh, and unfading. Between the pages of the Bible itstill lay when, a few weeks afterwards, that Bible was laid underthe young girl s head in her coffin13. A holy calm rested on her face,as if the earthly remains14 bore the impress of the truth that she nowstood in the presence of God.
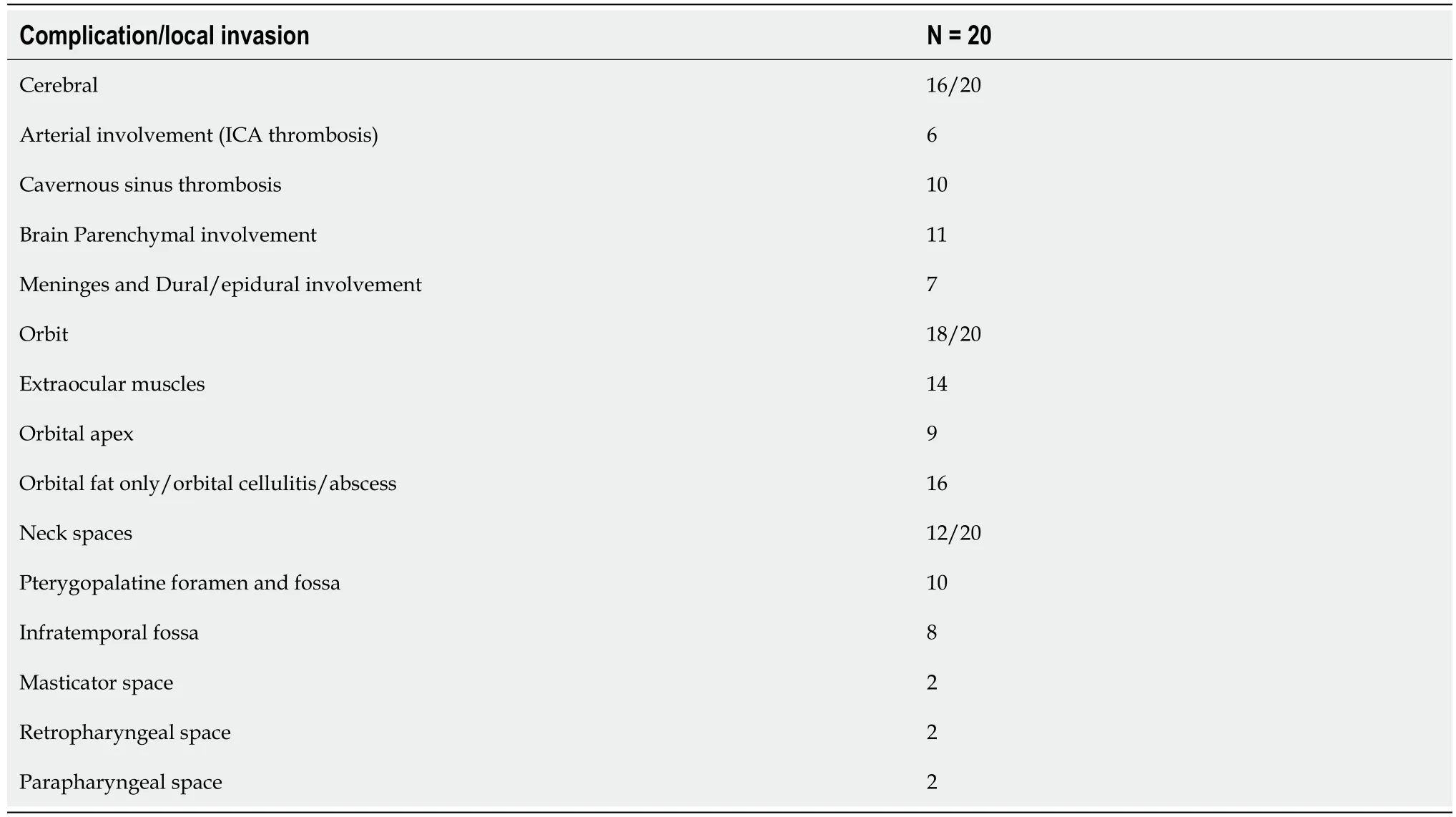
Involvement of the neck spaces was present in 60% of the cases(Table 2).The pterygopalatine space was involved in 50% of the cases.The infratemporal fossa was involved in 40% of the cases.The masticator space,retropharyngeal space,and parapharyngeal spaces were each involved in 10% of the cases.
At one month follow-up,only 50% of the patients survived,25% had progression of the lesions,20% had improvement in the lesions,and 5% had static lesions.
There were no cases of isolated cerebral mucormycosis.Involvement of the central nervous system(CNS)was present in 80% of the cases.The involvement of CNS included the following:leptomeningeal enhancement,meningoencephalitis,brain infarcts,brain abscesses,internal carotid artery thrombosis,cavernous sinus thrombosis,dural venous sinus thrombosis,and epidural abscesses.
The involvement of various structures of the CNS is listed in Table 2.Vascular involvement was present in 60% of the patients in our study,with the most common lesion being cavernous sinus thrombosis.Orbital involvement,which included orbital fat involvement,extraocular muscle involvement,and orbital cellulitis,was present in 90% of the cases(Table 2).
Most of the imaging features correlate with the angioinvasive pattern of the mucormycosis infection.The imaging findings are nonspecific,but early diagnosis is of paramount importance because of the associated morbidity and mortality.Senet al[19]found that cavernous sinus thrombosis and cribriform plate erosion were the commonest pathways of spread into the cranium and were present in 76% and 22% of the patients,respectively[19].The involvement may appear as leptomeningeal inflammation,which appears as leptomeningeal enhancement and involvement of the cranial nerves with signs of meningism.This may be accompanied by cerebritis.Cerebritis appears as T2-FLAIR hyperintensity with variable enhancement and heterogeneous diffusion restriction on diffusion-weighted imaging.Invasion of the parenchyma may appear as granuloma formation or abscess formation.Fungal granulomas may show faint enhancement and surrounding edema.

DISCUSSION
Most cases of rhinocerebral mucormycosis occurred in males in the present review as in other previous case series and reviews[6,7].Most patients had comorbidities,with diabetes being the predominant comorbidity as in other previous studies.In the study by Dubey
[8],all post–COVID-19 patients diagnosed with rhinocerebral mucormycosis were diabetic.This also includes new-onset diabetes due to the usage of corticosteroids during the treatment of COVID-19,which is as high as 38.18%[8].
In the present study,similar to the study by Therakathu
[9],unilateral involvement of the sinuses was more common.The ethmoid sinus was the most common sinus to be involved in the present study,followed by the maxillary sinus,as in the studies by Therakathu
[9]and Patel
[10].In the study by Therakathu
[9],the most common site to be involved other than the sinuses was the orbit(76%)and the face(57%),followed by the orbital apex,masticator space,pterygopalatine fossa,bone,skull base,cavernous sinus,brain,and internal carotid artery.Orbital involvement was also very common in the present study,accounting for 90% of the cases.However,in the study by Patel
[10],orbital involvement was present in only 60% of the cases.
Infection by fungi of the order
begins in the nasal cavity mostly in the middle turbinate and starts spreading,mostly invading the sphenoethmoidal complex[11,12].As the fungi have the ability to invade the blood vessels and the bony walls,they spread rapidly in immunocompromised hosts and those with chronic debilitating illnesses,to reach the sinus cavity[13].The necrotic tissue formed due to vascular occlusion acts as a rich niche for the further growth of the organism.Further invasion of the orbits and brain occurs through the foramen and through the sphenopalatine and internal maxillary arteries[14].
However,in the COVID-19pandemic,mucormycosis should be considered the first differential diagnosis.
The invasion in mucormycosis can be divided into three stages as per Rupa
[15]:
In contrast to the pyogenic abscess,fungal abscesses are frequently multiple and form at the corticomedullary junction and in the basal ganglia.Isolated fungal abscesses are rare,and one should suspect intravenous drug abuse if encountered with such a situation.Fungal abscesses have crenated borders and non-enhancing,diffusion-restricting intracavitary projections[20].They are hypointense on T1 and hyperintense on T2 and show rim enhancement[20].On diffusion-weighted imaging,Luthra
[20]found that fungal abscesses showed restriction of diffusion in the projections and the wall,and the core of the abscess had no restriction of diffusion.In the same study,the authors found that the apparent diffusion coefficient was higher for the wall of the abscess when compared to the intracavitary projections for the fungal abscess,and it was statistically significant[20].
Stage 2:The infection begins to spread to the peri-sinus areas,which are completely resectable.
Stage 3:The infection spreads into the intracranial cavity and to the surrounding areas of the sinuses,which are partially resectable.
The little pile of straw grew higher and softer. With only two weeks left until Christmas, the children wondered if their homemade bed would be comfortable enough for Baby Jesus.
Computed tomography appearance of the lesions in the sinuses
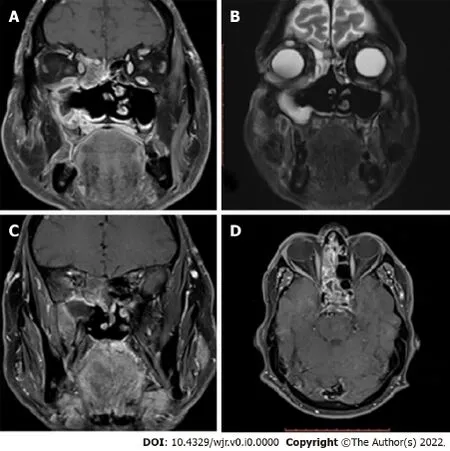
Computed tomography(CT)is usually the first investigation to be performed whenever invasive rhinocerebral mucormycosis is suspected based on clinical history and examination.The CT findings are nonspecific and include inflammatory changes in the sinuses.Early changes include mucosal thickening due to inflammation,bony erosions,and the formation of a mass lesion inside the sinuses,leading to the opacification of the sinuses.Hyperattenuation of the secretions on CT is suggestive of fungal sinusitis.The hyperdense areas seen in the sinuses are due to the presence of fungal hyphae and debris.Early changes suggestive of the spread of the infection outside the sinus include loss of normal fat density in the periantral fat(anterior,premaxillary,or retroantral)and orbit owing to edemafrom vascular congestion[16].Superficial cellulitis is another early sign of invasion,which is not common in nonfungal sinusitis[10].Late stages are characterized by signs suggestive of gross invasion of the structures of the orbit and the cranial cavity,which are more specific(Figure 1).Bone changes are also better visualized on CT.

The enhancement pattern of the lesions on contrast-enhanced computed tomography(CECT)varies from none to mild to heterogeneous enhancement,which was also seen in the cases in the present study[9,10].The mild form was the most common type of enhancement observed by Therakathu
[9].Mucosal involvement may appear as a diffuse thickening or nodular thickening.Bone involvement was seen in the form of bone rarefaction,erosion,and permeative destruction in 40% of the cases in the study by Therakathu
[9].Middlebrooks
[17]designed a CT-based model based on seven variables;this model can be used to suspect acute invasive fungal sinusitis.The variables are periantral fatinvolvement,bone dehiscence,orbital invasion,septal ulceration,pterygopalatine fossa,nasolacrimal duct,and lacrimal sac.In a study by Silverman
[16],most cases of extra sinus invasion occurred without bony invasion,suggesting that perivascular or perineural invasion plays an important role in the spread of mucormycosis.In the same study,Silverman
[16]noted that the presence of retroantral,facial,and orbital fat stranding was associated with a more aggressive infection.
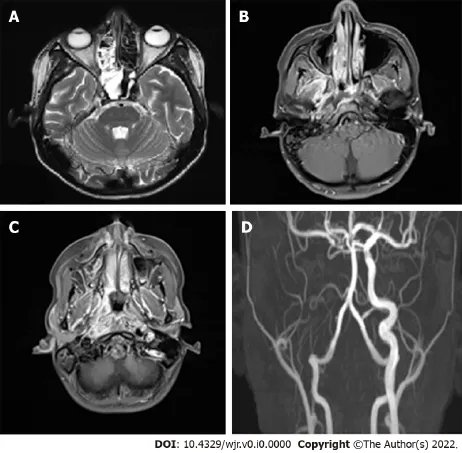
Magnetic resonance imaging appearance of the sinus lesions
Orbital and intracranial invasions are best seen by magnetic resonance imaging(MRI).Early changes are nonspecific.These include mucosal thickening,which appears hypointense on T1-weighted images and hyperintense on T2-weighted images.In the study by Therakathu
[9],on a T2-weighted sequence,37% of the lesions were isointense to mildly hypointense,32% were heterogeneous,and 32% were hyperintense.Fungal elements are hypointense on T2-weighted images(Figure 2).The enhancement pattern is best studied on fat-suppressed post-gadolinium images and is different for different lesions.Of all the cases in the study by Therakathu
[9],29% showed intense homogenous enhancement,36% showed heterogeneous enhancement,and 36% showed no enhancement.
Differential diagnosis on imaging for mucormycosis includes the following:Acute rhinosinusitis with complications,Wegener’s granulomatosis,and squamous cell carcinoma.
Because of the angioinvasive nature of mucormycosis,the vessels get thrombosed.Upon injection of the contrast,the normal expected pattern of mucosal enhancement in case of inflammatory lesions may not be visible.Instead,there will be a low-signal intensity of the affected mucosa of the nasal turbinate on T2-weighted MRI images associated with an increased signal on diffusion-weighted images.This was referred to as the black turbinate sign by Safder
[18].
I suppose it is only on our account that you perform thiscommon-place work yourself, instead of leaving it to your servant todo all that sticking together.
Imaging features of intracranial mucormycosis
THERE was once upon a time a widow1 who had two daughters.2 The eldest13 was so much like her in the face and humor that whoever looked upon the daughter saw the mother. They were both so disagreeable and so proud4 that there was no living with them.
Stage 1:The infection is localized to the nasal cavity and paranasal sinuses.
Vascular complications are observed in the late stages.They include both venous and arterial complications such as cavernous sinus thrombosis,arterial thrombosis,and aneurysmal dilatation(Figure 3).In the study by Mohindra
[21],the role of MRI in the detection of vascular lesions was studied.In the study by Razeket al[22],cavernous sinus involvement in mucormycosis appears hypointense on T1 and T2 sequences with intense,inhomogeneous post-contrast enhancement.Cavernous sinus thrombosis is the most common complication in the present study,as in certain published studies.
Cause of the increased incidence and severity of mucormycosis during the COVID-19 pandemic
Diabetes was one of the major predisposing factors for mucormycosis during the COVID-19 pandemic.Prakash
[23]highlighted that rhinocerebral mucormycosis cases were predominantly present in those with uncontrolled diabetes and diabetic ketoacidosis,and few were present in immunosuppressed hosts.The findings were similar to those in other studies by Sen
[18],John
[24],and Hoenigl
[25].In the afore mentioned studies,the prevalence of diabetes was 78%-94% among patients with mucormycosis post–COVID-19 infection.In Patel
’s study,patients with mucormycosis with poor glycemic control had a more invasive disease,which was statistically significant(
value = 0.040)[10].The rampant use of corticosteroids and other immunomodulatory drugs to control the severity of the COVID-19 infection has further led to the increased predisposition[26].During the peak of the pandemic,when healthcare facilities were functioning beyond their capacities,there were instances of unsupervised treatment with these immunomodulatory agents,leading to further escalation of the problem.
I was pleased that twenty men had signed up for the class. This was the maximum number I had said I could take. I spend the first hour with them, talking about what it was like to be a writer. Telling them that there is a joy and a freedom in the words. That no matter how much they were all forced to be alike, dress alike, eat the same food, keep the same hours, that in their writing they could finally be different. As different as they wanted to be. Writing, I told them, can be the most liberating6 of all the arts. You can be free with the word. There are no limits. told them that every time I picked up a pencil or sat down at a computer or a typewriter that it was as if I was coming home, coming home to my art, my words, that this was a world that no one else could take away. This art would sustain me throughout all my days.
CONCLUSION
Rhinocerebral mucormycosis constituted the aftermath of the COVID-19 pandemic,leading to a rapid increase in the number of cases,which were previously restricted to only a few susceptible groups of patients.Rhinocerebral mucormycosis is associated with high mortality and morbidity.Hence,it should be suspected in any patient who presents symptoms of sinusitis,facial swelling,or CNS symptoms.After clinical examination,imaging is the backbone of the diagnosis of this severe disease.CT helps in the preliminary diagnosis and helps stage the disease.CT detects bony erosion better.However,when an orbital and intracranial extension is present,MRI is preferred,as it delineates the involvement of these structures better.MRI can also delineate vascular involvement better.In accessible sites,biopsy and potassium hydroxide mount help clinch the diagnosis.The treatment of rhinocerebral mucormycosis consists of debridement of the necrotic tissue along with intravenous antifungals for a prolonged duration.Control of diabetes and judicious use of corticosteroids and immunomodulatory drugs can decrease the incidence of this life-threatening disease.
FOOTNOTES
Saneesh PS analyzed the data;Morampudi SC analyzed the data and wrote the manuscript;Yelamanchi R analyzed the data and wrote the manuscript;All authors have read and approved the final manuscript.
And so they laughed and jeered11, and it was so hot that the bear said, The enemy won t be here at this rate for many hours to come, so I ll just curl myself up in the fork of the tree and have a little sleep
None of the authors in the study have any conflict of interest.
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial(CC BYNC 4.0)license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See:https://creativecommons.org/Licenses/by-nc/4.0/
India
Immediately after this he was called upon, and swam through the sea up the river to where the troll stood on the bank and restored him to human shape with the same words as before
P S Saneesh 0000-0003-1492-7395;Satya Chowdary Morampudi 0000-0002-4061-5363;Raghav Yelamanchi 0000-0001-6786-8056.
Liu JH
A
Liu JH
1 Ibrahim AS,Spellberg B,Walsh TJ,Kontoyiannis DP.Pathogenesis of mucormycosis.
2012;54 Suppl 1:S16-S22[PMID:22247441 DOI:10.1093/cid/cir865]
2 Camara-Lemarroy CR,González-Moreno EI,Rodríguez-Gutiérrez R,Rendón-Ramírez EJ,Ayala-Cortés AS,Fraga-Hernández ML,García-Labastida L,Galarza-Delgado Dá.Clinical features and outcome of mucormycosis.
2014;2014:562610[PMID:25210515 DOI:10.1155/2014/562610]
3 Sweeney RM,McAuley DF.Acute respiratory distress syndrome.
2016;388:2416-2430[PMID:27133972 DOI:10.1016/S0140-6736(16)00578-X]
4 Song G,Liang G,Liu W.Fungal Co-infections Associated with Global COVID-19 Pandemic:A Clinical and Diagnostic Perspective from China.
2020;185:599-606[PMID:32737747 DOI:10.1007/s11046-020-00462-9]
5 Roden MM,Zaoutis TE,Buchanan WL,Knudsen TA,Sarkisova TA,Schaufele RL,Sein M,Sein T,Chiou CC,Chu JH,Kontoyiannis DP,Walsh TJ.Epidemiology and outcome of zygomycosis:a review of 929 reported cases.
2005;41:634-653[PMID:16080086 DOI:10.1086/432579]
6 Herrera DA,Dublin AB,Ormsby EL,Aminpour S,Howell LP.Imaging findings of rhinocerebral mucormycosis.
2009;19:117-125[PMID:19721767 DOI:10.1055/s-0028-1096209]
7 Gupta N,Dembla S.Cranial nerve involvement in mucormycosis in post-COVID patients:a case series.
2022;53:28[DOI:10.1186/s43055-022-00700-8]
8 Dubey S,Mukherjee D,Sarkar P,Mukhopadhyay P,Barman D,Bandopadhyay M,Pandit A,Sengupta A,Das S,Ghosh S,Adhikari S,Biswas PS,Pal P,Roy H,Patra N,Das A,Sinha P,Mondal MK,Shrivastava SR,Bhattacharya K,Mukhopadhyay M,Ahmed K,Halder TK,Saha M,Maity S,Mandal A,Chatterjee D,Saha S,Chunakar A,Saha A,Ray BK.COVID-19 associated rhino-orbital-cerebral mucormycosis:An observational study from Eastern India,with special emphasis on neurological spectrum.
2021;15:102267[PMID:34509790 DOI:10.1016/j.dsx.2021.102267]
9 Therakathu J,Prabhu S,Irodi A,Sudhakar SV,Yadav VK,Rupa V.Imaging features of rhinocerebral mucormycosis:a study of 43 patients.
2018;49:447-452[DOI:10.1016/j.ejrnm.2018.01.001]
10 Patel DD,Adke S,Badhe PV,Lamture S,Marfatia H,Mhatre P.COVID-19 associated Rhino-Orbito-Cerebral Mucormycosis:Imaging spectrum and Clinico-radiological correlation- a single Centre experience.
2022;82:172-178[PMID:34864270 DOI:10.1016/j.clinimag.2021.10.014]
11 Gillespie MB,Huchton DM,O'Malley BW.Role of middle turbinate biopsy in the diagnosis of fulminant invasive fungal rhinosinusitis.
2000;110:1832-1836[PMID:11081595 DOI:10.1097/00005537-200011000-00013]
12 Gillespie MB,O'Malley BW Jr,Francis HW.An approach to fulminant invasive fungal rhinosinusitis in the immunocompromised host.
1998;124:520-526[PMID:9604977 DOI:10.1001/archotol.124.5.520]
13 Skiada A,Pavleas I,Drogari-Apiranthitou M.Epidemiology and Diagnosis of Mucormycosis:An Update.
2020;6[PMID:33147877 DOI:10.3390/jof6040265]
14 Bhandari J,Thada PK,Nagalli S.Rhinocerebral Mucormycosis.[Updated 2021 Nov 25].In:StatPearls[Internet].Treasure Island(FL):StatPearls Publishing;2022 Jan.Available from:https://www.ncbi.nlm.nih.gov/books/NBK559288/
15 Rupa V,Maheswaran S,Ebenezer J,Mathews SS.Current therapeutic protocols for chronic granulomatous fungal sinusitis.
2015;53:181-186[PMID:26030043 DOI:10.4193/Rhino14.183]
16 Silverman CS,Mancuso AA.Periantral soft-tissue infiltration and its relevance to the early detection of invasive fungal sinusitis:CT and MR findings.
1998;19:321-325[PMID:9504486]
17 Middlebrooks EH,Frost CJ,De Jesus RO,Massini TC,Schmalfuss IM,Mancuso AA.Acute Invasive Fungal Rhinosinusitis:A Comprehensive Update of CT Findings and Design of an Effective Diagnostic Imaging Model.
2015;36:1529-1535[PMID:25882281 DOI:10.3174/ajnr.A4298]
18 Safder S,Carpenter JS,Roberts TD,Bailey N.The "Black Turbinate" sign:An early MR imaging finding of nasal mucormycosis.
2010;31:771-774[PMID:19942703 DOI:10.3174/ajnr.A1808]
19 Sen M,Honavar SG,Bansal R,Sengupta S,Rao R,Kim U,Sharma M,Sachdev M,Grover AK,Surve A,Budharapu A,Ramadhin AK,Tripathi AK,Gupta A,Bhargava A,Sahu A,Khairnar A,Kochar A,Madhavani A,Shrivastava AK,Desai AK,Paul A,Ayyar A,Bhatnagar A,Singhal A,Nikose AS,Tenagi AL,Kamble A,Nariani A,Patel B,Kashyap B,Dhawan B,Vohra B,Mandke C,Thrishulamurthy C,Sambare C,Sarkar D,Mankad DS,Maheshwari D,Lalwani D,Kanani D,Patel D,Manjandavida FP,Godhani F,Agarwal GA,Ravulaparthi G,Shilpa GV,Deshpande G,Thakkar H,Shah H,Ojha HR,Jani H,Gontia J,Mishrikotkar JP,Likhari K,Prajapati K,Porwal K,Koka K,Dharawat KS,Ramamurthy LB,Bhattacharyya M,Saini M,Christy MC,Das M,Hada M,Panchal M,Pandharpurkar M,Ali MO,Porwal M,Gangashetappa N,Mehrotra N,Bijlani N,Gajendragadkar N,Nagarkar NM,Modi P,Rewri P,Sao P,Patil PS,Giri P,Kapadia P,Yadav P,Bhagat P,Parekh R,Dyaberi R,Chauhan RS,Kaur R,Duvesh RK,Murthy R,Dandu RV,Kathiara R,Beri R,Pandit R,Rani RH,Gupta R,Pherwani R,Sapkal R,Mehta R,Tadepalli S,Fatima S,Karmarkar S,Patil SS,Shah S,Dubey S,Gandhi S,Kanakpur S,Mohan S,Bhomaj S,Kerkar S,Jariwala S,Sahu S,Tara S,Maru SK,Jhavar S,Sharma S,Gupta S,Kumari S,Das S,Menon S,Burkule S,Nisar SP,Kaliaperumal S,Rao S,Pakrasi S,Rathod S,Biradar SG,Kumar S,Dutt S,Bansal S,Ravani SA,Lohiya S,Ali Rizvi SW,Gokhale T,Lahane TP,Vukkadala T,Grover T,Bhesaniya T,Chawla U,Singh U,Une VL,Nandedkar V,Subramaniam V,Eswaran V,Chaudhry VN,Rangarajan V,Dehane V,Sahasrabudhe VM,Sowjanya Y,Tupkary Y,Phadke Y;members of the Collaborative OPAI-IJO Study on Mucormycosis in COVID-19(COSMIC)Study Group.Epidemiology,clinical profile,management,and outcome of COVID-19-associated rhino-orbital-cerebral mucormycosis in 2826 patients in India - Collaborative OPAI-IJO Study on Mucormycosis in COVID-19(COSMIC),Report 1.
2021;69:1670-1692[PMID:34156034 DOI:10.4103/ijo.IJO_1565_21]
20 Luthra G,Parihar A,Nath K,Jaiswal S,Prasad KN,Husain N,Husain M,Singh S,Behari S,Gupta RK.Comparative evaluation of fungal,tubercular,and pyogenic brain abscesses with conventional and diffusion MR imaging and proton MR spectroscopy.
2007;28:1332-1338[PMID:17698537 DOI:10.3174/ajnr.A0548]
21 Mohindra S,Mohindra S,Gupta R,Bakshi J,Gupta SK.Rhinocerebral mucormycosis:the disease spectrum in 27 patients.
2007;50:290-296[PMID:17576322 DOI:10.1111/j.1439-0507.2007.01364.x]
22 Razek AA,Castillo M.Imaging lesions of the cavernous sinus.
2009;30:444-452[PMID:19095789 DOI:10.3174/ajnr.A1398]
23 Prakash H,Chakrabarti A.Global Epidemiology of Mucormycosis.
2019;5[PMID:30901907 DOI:10.3390/jof5010026]
24 John TM,Jacob CN,Kontoyiannis DP.When Uncontrolled Diabetes Mellitus and Severe COVID-19 Converge:The Perfect Storm for Mucormycosis.
2021;7[PMID:33920755 DOI:10.3390/jof7040298]
25 Hoenigl M,Seidel D,Carvalho A,Rudramurthy SM,Arastehfar A,Gangneux JP,Nasir N,Bonifaz A,Araiza J,Klimko N,Serris A,Lagrou K,Meis JF,Cornely OA,Perfect JR,White PL,Chakrabarti A;ECMM and ISHAM collaborators.The emergence of COVID-19 associated mucormycosis:a review of cases from 18 countries.
2022;3:e543-e552[PMID:35098179 DOI:10.1016/S2666-5247(21)00237-8]
26 Al-Tawfiq JA,Alhumaid S,Alshukairi AN,Temsah MH,Barry M,Al Mutair A,Rabaan AA,Al-Omari A,Tirupathi R,AlQahtani M,AlBahrani S,Dhama K.COVID-19 and mucormycosis superinfection:the perfect storm.
2021;49:833-853[PMID:34302291 DOI:10.1007/s15010-021-01670-1]
 World Journal of Radiology2022年7期
World Journal of Radiology2022年7期
- World Journal of Radiology的其它文章
- Catheter-based renal sympathetic nerve denervation on hypertension management outcomes
- Type 2 dynamic curves:A diagnostic dilemma
- Impact of X-radiation in the management of COVID-19 disease
- Molecular imaging as a tool for evaluation of COVID-19 sequelae–A review of literature
- Expanding utility of cardiac computed tomography in infective endocarditis:A contemporary review
