Prevalence and risk factors of infertility in a Mongolian population
Tuvshinbayar Negdel, Arigbukh Enkhbat, Badrakh Munkhbayar, Khantushig Bilegsuren, Ariunaa Ganbold,Khuderchuluun Nanjid, Carol W Readhead, Lkhagva-Ochir Erkhembaatar, Erkhembaatar Tuduvdorj,Munkhzol Malchinkhuu, Odkhuu Enkhtaivan,
1Department of Basic Science, School of Nursing, Mongolian National University of Medical Science, Ulaanbaatar, Mongolia
2Department of Pathophysiology, School of Bio-Medicine, Mongolian National University of Medical Science, Ulaanbaatar, Mongolia
3RMC, IVF Center, Ulaanbaatar, Mongolia
4Department of Biostatistics, Mongolian National University of Medical Science, Ulaanbaatar, Mongolia
5Biology and Biological Engineering, California Institute of Technology, California, USA
6First Maternity Hospital, Ulaanbaatar, Mongolia
7Department of Obstetrics and Gynecology, School of Medicine, Mongolian National University of Medical Science, Ulaanbaatar, Mongolia
ABSTRACT
Objective: To investigate and analyze the prevalence and risk factors of infertility in a Mongolian population.
Methods: We conducted a population-based cross-sectional study between September 2016 and November 2021. Our study population of 1 919 participants consisted of residents of Ulaanbaatar city and four regions of Mongolia. A pretested standardized and structured questionnaire was used to gather data from the participants. Our questionnaire comprised categories influencing infertility, such as socioeconomic status, lifestyle factors, health, reproductive history, present status, and sexual function. In addition, trained staff conducted face-to-face interviews with the participants.
Results: Our study showed an infertility incidence of 8.2% , with primary infertility at 2.76% and secondary infertility at 5.47% .Compared with the urban area of Ulaanbaatar, the prevalence of infertility was significantly higher amongst the rural population(P<0.001). Risk factors of infertility included advanced age (35-39 years, OR 1.8, 95% CI 1.99-6.55; >40 years, OR 2.1, 95% CI 2.62-8.55), living rural region (aOR 2.4, 95% CI 1.62-3.69), alcohol consumption (aOR 1.6, 95% CI 1.11-2.44), chronic diseases (aOR 1.6, 95% CI 1.20-2.38), reproductive disease (aOR 2.6, 95% CI 1.86-3.88), gynecological operative history (aOR 2.1, 95% CI 1.38-3.21), ovarian cyst (aOR 4.2, 95% CI 2.70-6.40), gonorrhea (aOR 2.4,95% CI 1.01-6.16), non-malignant uterine cancer (aOR 2.9, 95% CI 1.40-6.70), and endometriosis (aOR 4.7, 95% CI 1.41-15.62).
Conclusions: In Mongolia, the average infertility rate is 8.2% ,similar to the average worldwide and is significantly higher in rural communities. Our study shows the most significant risk factors for infertility are age, alcohol consumption, and rural living. In addition,an unfavorable gynecological history and some diseases also pose a risk to fertility.
KEYWORDS: Infertility; Risk factors; Prevalence, Region;Primary infertility; Secondary infertility; Reproductive health; Age
Significance
Many studies have shown that the prevalence of infertility in developing and developed countries is different due to factors that cause infertility. This study investigated the prevalence and risk factors of infertility throughout Mongolia using a population-based research study design, and revealed that in Mongolia, the overall 12 monthly prevalence of infertility was 8.2% , and primary and secondary infertility was 2.76% and 5.47% , respectively. In addition, the study shows the most significant risk factors for infertility are age, alcohol consumption, and rural living. Moreover, an unfavorable gynecological history and some diseases also pose a risk to fertility.
1. Introduction
As defined by the World Health Organization (WHO), infertility is the failure to conceive after at least 12 months of regular unprotected sexual intercourse[1]. Infertility is a medical issue that carries a social stigma and leads to decreased quality of life, emotional instability,and low self-esteem, especially in women[2]. There are wideranging estimates of infertility prevalence depending on the study and definition of infertility[3-5]. A global study estimated the 12-month infertility prevalence to be 9% , with rates ranging from 3.5% to 16.7% in more developed nations and from 6.9% to 9.3% in lessdeveloped nations[6]. There are around 186 million married women in developing countries (excluding China) between the age of 15 and 49 years with primary and secondary infertility[7].
The differences between the developed and developing world have been increasing because of the availability and accessibility of infertility care and different socio-cultural values for procreation and childlessness[8]. The only available data on infertility in Mongolia were represented demographically with a primary infertility occurrence of 1.00% -1.99% , while secondary infertility was 13% [9].In some areas, including developing countries, unsafe abortion, poor maternity care, and sexually transmitted infections contribute to a higher rate of secondary infertility than primary infertility[10].
Mongolia has one of the highest rates of secondary infertility[9],which may largely be attributed to high rates of sexually transmitted infections. For instance, the rate of gonorrhea among women and men in Mongolia was 3.3% and 2.9% , and chlamydia was 19.5% and 15.6% , respectively[11]. Mongolia has an unregulated growth of the private healthcare sector and poor enforcement of standards and technical guidelines for safe abortion[12]. Mongolian-based studies on infertility, such as Bayasgalan et al, are clinically based; they found a female infertility rate of 45.8% and a male infertility rate of 25.6% , unexplained infertility was 9.8% , and the combined rate for couples was 18.8% .
In Mongolia, the significant factors for female infertility were tubal adhesions and endocrinal background. Male factors were varicocele, azoospermia, and testicular damage[13]. Infertility studies in Mongolia have mainly been hospital-based, with limited epidemiological studies. Therefore, accurate assessment of infertility using epidemiological study methods is crucial to provide highquality assessment, treatment, and management. This study aimed to provide the first 12-month prevalence rate of infertility with a population-based study, including causative factors leading to infertility in women of reproductive age in Mongolia.
2. Subjects and methods
2.1. Design and study population
We conducted a population-based cross-sectional study from September 2016 to November 2021 in the four regions of Mongolia and the capital city of Ulaanbaatar. Mongolia is divided into four regions based on geographical and economic factors (Eastern,Western, Central, and Khangai), while the capital city Ulaanbaatar is viewed as a separate region. Each region is made up of provinces,with a total of 21 provinces in all.
For the study, we selected married couples who were Mongolia′s citizens and had been living together for at least one year at a permanent residence in one of the selected regions. The women were between 20-45 years of age, while there was no age selection for men. Couples excluded from the study were those who had lived apart for longer than three months, used birth control, were presently breastfeeding, or were women in early menopause.
2.2. Sample and data collection
The appropriate sample size for the study was calculated by taking the average international rates of infertility of around 8% -10% .International infertility rates were used to calculate the appropriate sample size since no previous infertility studies have been undertaken in Mongolia. With an allowable error of 5% and a confidence level of 95% , a total sample size of 2 000 couples was required for the study. Incomplete questionnaires (81 respondents) were excluded resulting in a total of 1 919 couples participating in the study, giving a response rate of 96% . This nationwide study involved one or two provinces within each region randomly selected by a multi-stage stratified cluster sampling design. First, we calculated the study sample of reproductive-age couples in each of the four regions[(Govi-Altai province (n=300) from the Western region, Khuvsgul(n=220) and Orkhon (n=218) provinces from the Northern region,Darkhan (n=174) and Umnugovi (n=150) provinces from the Central region, Dornod province (163) from the Eastern region and Ulaanbaatar (n=694) region]. After participants agreed to participate in the study, they were asked to sign a consent form. Then, we randomly approached eligible couples with assistance from the local family healthcare centers from each Sum (territorial administrative unit of Mongolia) and District. The couples that agreed to participate were interviewed at the local family healthcare center. In some cases,participants could not come to the local healthcare center, so we surveyed their homes.
A pretested standardized and structured questionnaire was used to gather data from the participants. We tested the validity of the questionnaire using the face validity method. As a precaution against possible difficulties arising from illiteracy and cultural miscommunication errors, we conducted a verbal interview following the questionnaire. In order to protect the participant′s privacy and to gather accurate information, a trained interviewer conducted the interview individually with each person in a private setting. Our questionnaire assessed general demographic and socio-economic status, medical history, toxin exposure, reproductive history, female reproductive health (e.g., age of menarche, last menstrual period,menstrual regularity, menstrual cycle, menstrual blood volume,medical history, operative history), marriage and childbearing status (e.g., length of marriage and cohabitation, pregnancy history including information concerning live births, miscarriage,induced abortions and stillbirths, frequency of sexual intercourse)and past medical consultation on infertility. We also conducted anthropometric measurements. For gauging alcohol consumption,tobacco use, and physical activity, we based our questions on WHO STEPS Instrument′s NCD (non-communicable disease) risk factor questionnaire[14].
2.3. Infertility definitions
Our study used WHO′s definition of infertility as "a disease of the reproductive system defined by the failure to achieve a clinical pregnancy after 12 months or more of regular unprotected sexual intercourse"[15]. In addition, primary female infertility is defined as a woman who has never before been diagnosed with a clinical pregnancy and meets the criteria of being classified as having infertility. In contrast, secondary female infertility is defined as "a woman currently unable to establish a clinical pregnancy but who has previously been diagnosed with a clinical pregnancy"[16]. Since the female population usually defines infertility, we calculated the epidemiology of infertility solely based on female data.
2.4. Statistical analysis
Data analysis was performed using the Statistical Program for Social Sciences (SPSS v 20, IBM). Missing data for the variables analyzed were excluded. Continuous measurements were shown as mean, standard deviation (SD), and categorical variables were expressed as percentages. We used Pearson′s Chi-squared test to compare disordes classified data and independent sample t test to compare the means of two samples. Binary logistic multivariate regression analysis was performed to explore potential risk factors and corresponding odds ratio (OR). We chose covariates examined by multivariable logistic regression based on the results of univariate analysis. All P value differences were considered statistically significant when P<0.05.
2.5. Ethics approval statement
We gained approval from the Mongolian National University of Medical Sciences ethics committee (No. 16/3/2016-16) to conduct our survey. All participants agreed to an informed consent form after accepting to be included.
3. Results
3.1. Study population
Our study population of 1 920 participants consisted of residents of Ulaanbaatar city and four regions of Mongolia (Western, Eastern,Central, and Khangai). The general characteristics of the participants are shown in Table 1.
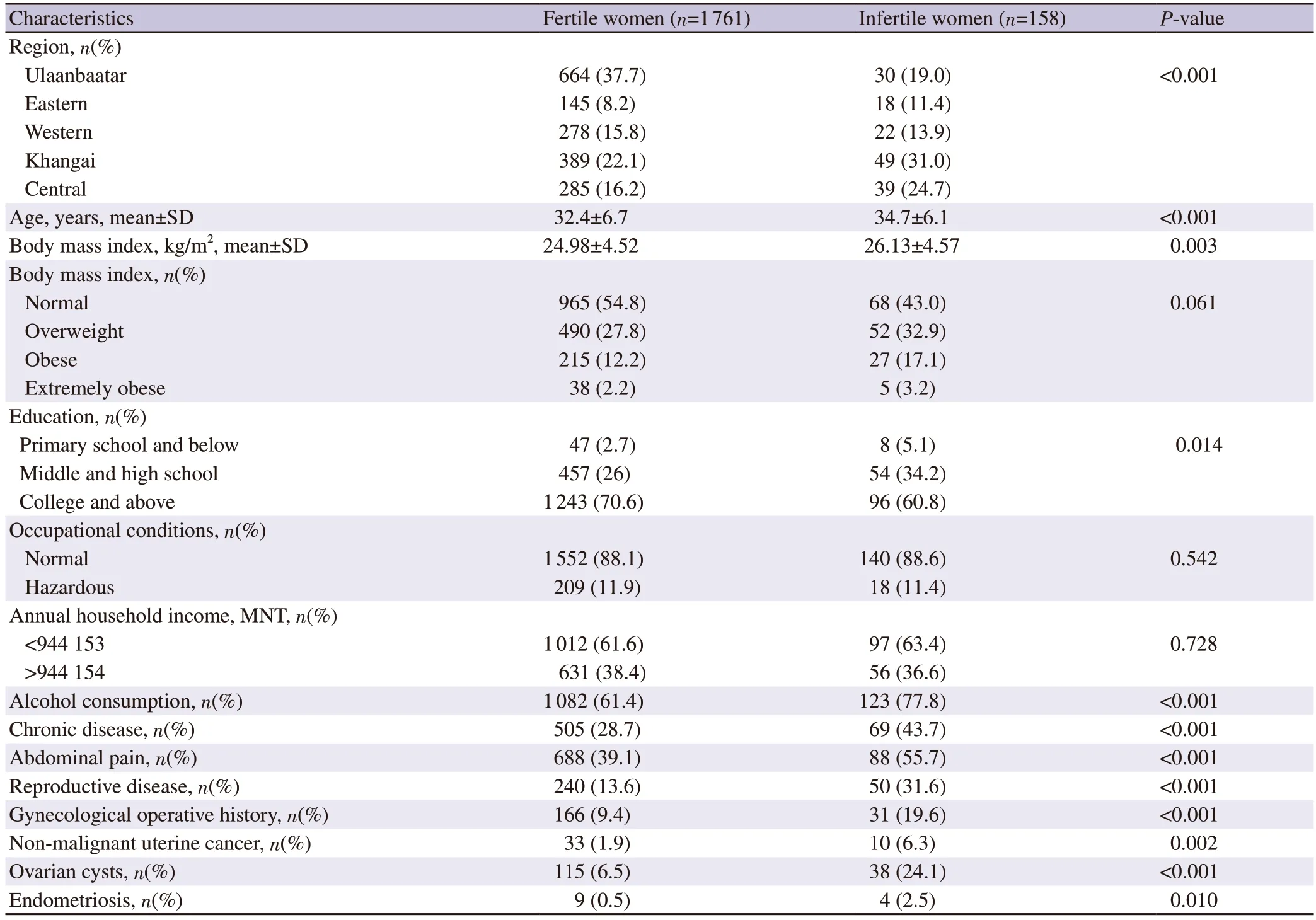
Table 1. General characteristics of study participants.
3.2. Prevalence of infertility and patterns of region
Our study showed an infertility incidence of 8.2% (n=158), with primary infertility at 2.76% (n=53) and secondary infertility at 5.46% (n=105). Geographically, the prevalence rate was as follows:Central region (12% , n=39), Khangai region (11.2% , n=49),Western region (7.3% , n=22), Eastern region (11% , n=18), Capital city Ulaanbaatar (4.3% , n=30). Compared with the urban area of Ulaanbaatar, the prevalence of infertility was significantly higher amongst the rural population (P<0.001). As it is the only territory with city status in Mongolia, we viewed it as an urban area.
3.3. Age-related patterns of infertility
Our results showed a trend of secondary and overall infertility that increased with the women’s age. However, the same trend was present in primary infertility (Table 2). Women between 40-45 years of age had the highest rate of infertility (11.9% ) compared to women 20-24 years of age, who had a low infertility rate (1.4% ) (P<0.001).Furthermore, when we mapped the prevalence of infertility as individual ages instead of groups, we noticed a slow decline from ages 30-36 and then a sudden spike at ages 36-39, followed by a plateau until age 45 (Figure 1).
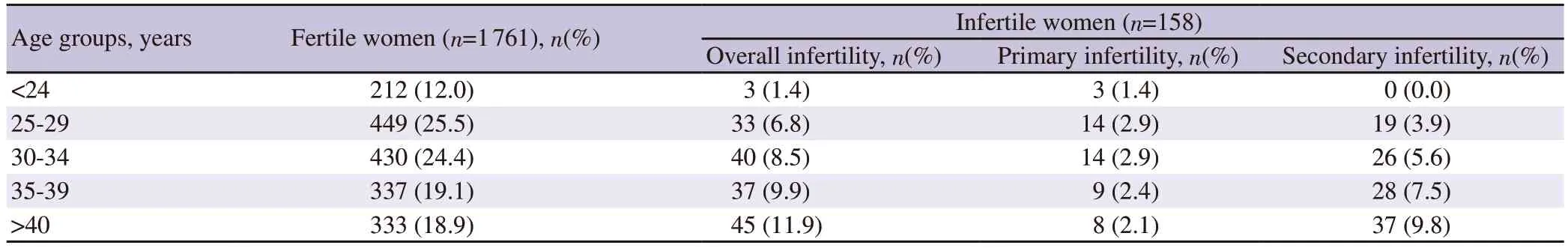
Table 2. Infertility prevalence of different age groups.
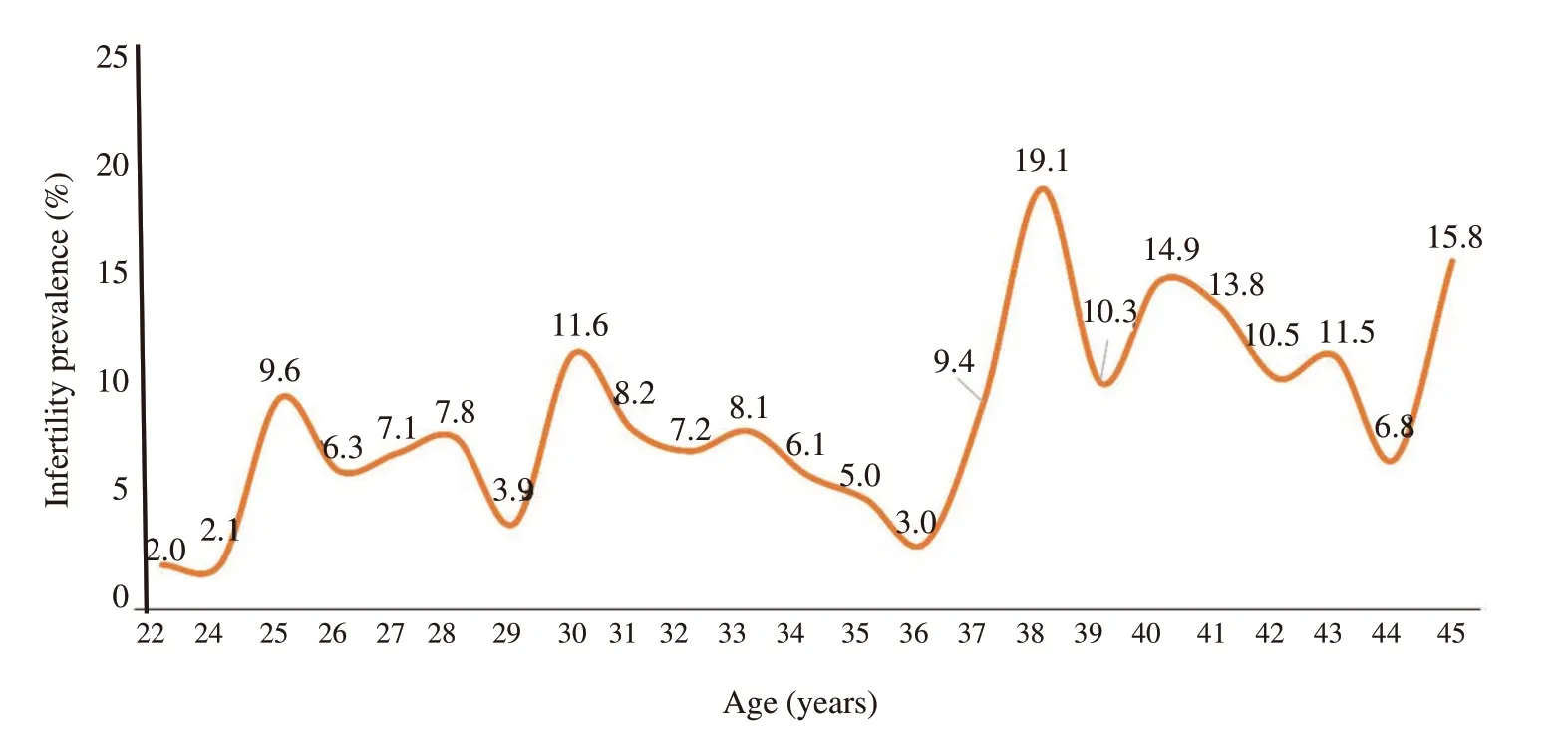
Figure 1. Infertility prevalence by age.
3.4. Risk factors for infertility
We then divided our participants into infertile or fertile female groups. Adjusting for age, we calculated the association between infertility and risk factors among women. We calculated the socioeconomic risk of infertility compared to the 20-24-year age group. Age was the most significant risk factor among the risk factors, with the risk increasing by 1 to 2-fold with each progressing age group. Social factors, for example, monthly household income,were not significant risk factors for infertility; however, rural living was a significant risk factor (aOR 2.4, 95 CI 1.62-3.69, P<0.001) (Table 3).
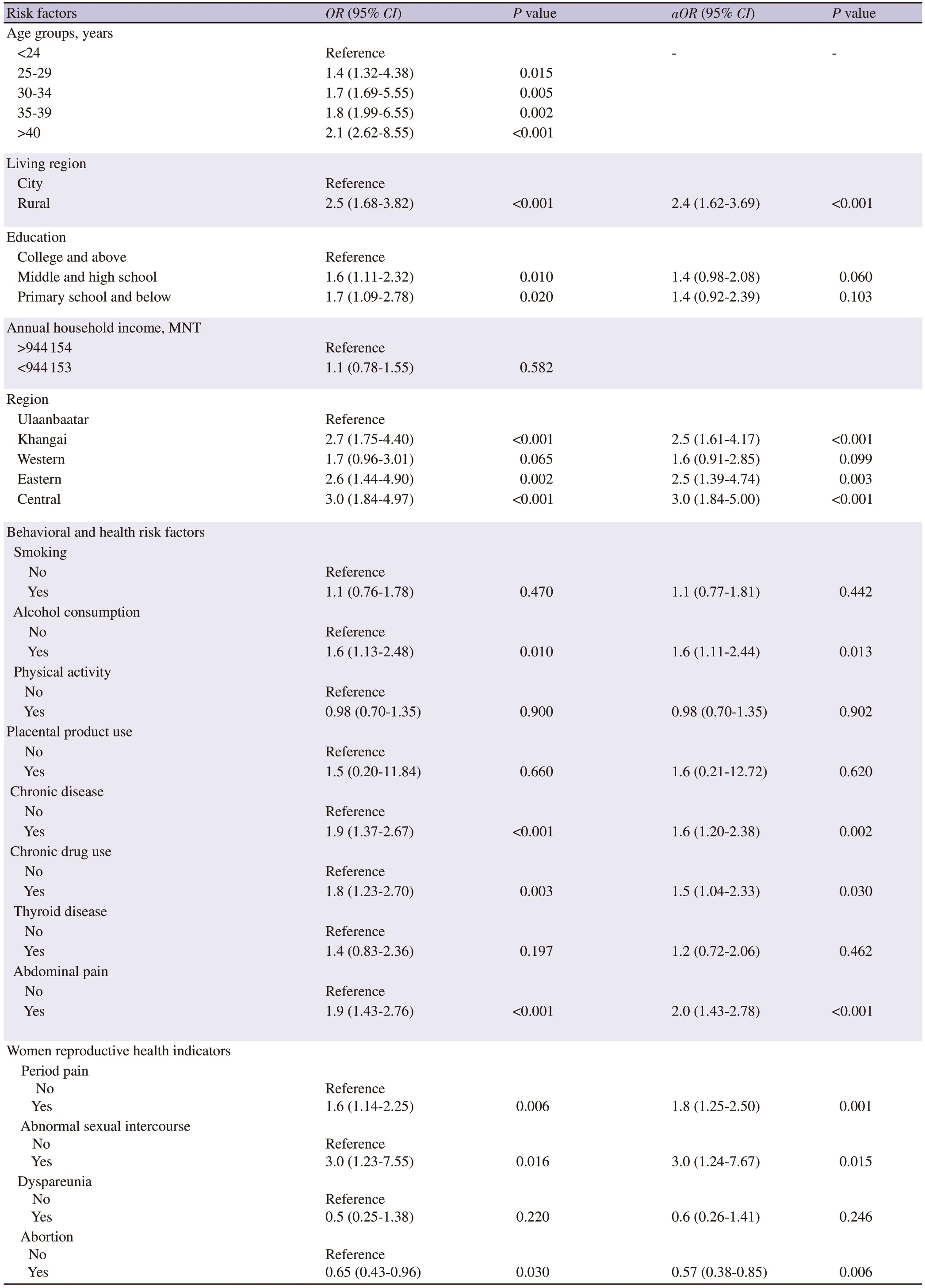
Table 3. Multivariate logistic regression analysis predicting risk factors for female infertility.
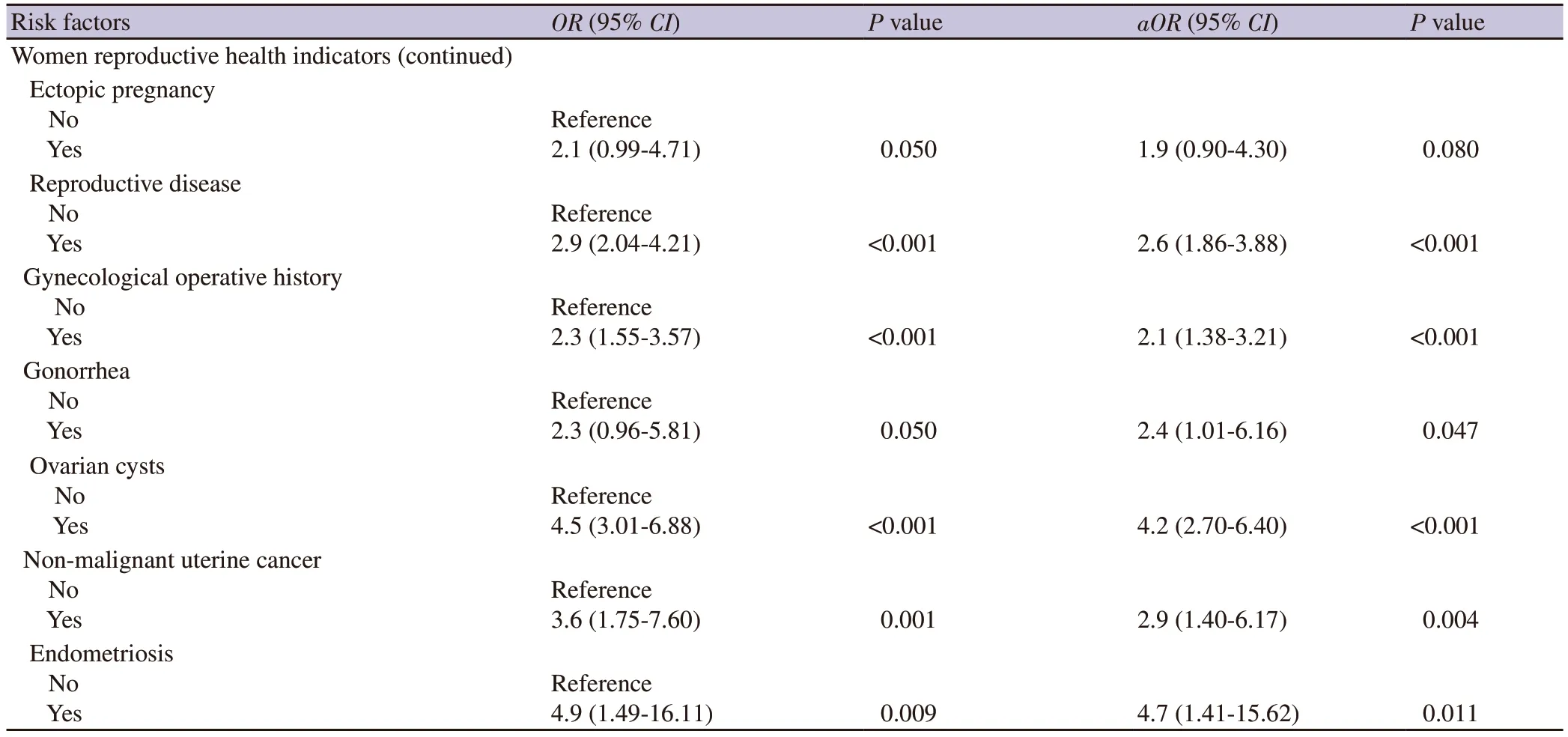
Table 3. Multivariate logistic regression analysis predicting risk factors for female infertility (continued).
Table 3 shows the risk of one factor in the behavioral and health indicators of the women surveyed. Factors contributing to infertility included alcohol consumption (aOR 1.6, 95 CI 1.11-2.44, P=0.013),chronic disease (aOR 1.6, 95 CI 1.20-2.38, P=0.002), abdominal pain (aOR 2.0, 95 CI 1.43-2.78, P<0.001), and drug abuse (aOR 1.5, 95 CI 1.04-2.33, P=0.030). We also surveyed the risk of one factor in women′s reproductive health indicators, such as menstrual information, sexual behavior, obstetrics, and women′s disease history. It can be seen that menstrual changes, lack of regular sexual intercourse, gynecological diseases, ectopic pregnancies,gynecological surgery, and infection of gonorrhea were significant risks for infertility. However, abortion was not a risk factor for infertility.
4. Discussion
Mongolia is a landlocked nation that borders the People′s Republic of China to the south and the Russian Federation to the north. It comprises 21 provinces distributed in 4 regions (Khangai, Central,Eastern, and Western) and Ulaanbaatar city. Globally, it ranks 6th for the least densely populated country at approximately 1.7 persons per square kilometer. The Mongolian Government′s policy on population development between 2016-2025 is to create favorable conditions for sustainable population growth. Until now, there have not been population-based studies on infertility and its risk factors in Mongolia. Researchers used the number of couples and females with infertility at a particular time and location concerning the total population to calculate the prevalence rate of infertility. The prevalence of infertility can be defined as the total number of women or couples who experience infertility within a given particular time and in a given place, in proportion to the total population in the same time and place. Our study was done using this definition for the population of Ulaanbaatar and the four regions of Mongolia. We found an infertility prevalence of 8.2% , which agrees with similar global studies with a median infertility prevalence ranging from 6.9% to 9.3% [2].
Mongolia is a developing country, and our result of 8.2% was similar to the global rate of infertility in developing countries at 6.9% -9.3% . Larsen et al′s study of primary and secondary infertility in sub-Saharan Africa showed a prevalence of 3% and 5% , respectively[17]. This was in keeping with our study, which showed a prevalence of primary and secondary infertility of 2.76% and 5.47% , respectively. However, their definition of infertility as "5 years or more of failure to conceive" was not the same as our definition of infertility, which was 12 months of failed conception.Mongolia and the Sub-Saharan region had a high rate of gonorrhea and chlamydia[11,18], risk factors for secondary infertility that could explain the similar results of the two studies. A study was done in a fellow low- and middle-income country, Nigeria which had a prevalence rate of infertility rate of 31.1% [19]. This is much higher than the infertility rate we measured in Mongolia, but it may be due to a different study design. A population-based study conducted in our neighboring country China had a prevalence of 15.5% [20].Although both studies used the exact definition of infertility and study methods, the contrasting result of 8.2% is due to governmental policy on reproduction , inclusion criteria, the age of the participants,socio-economic values, and other factors. Recent meta-analysis study results in Iran showed a very similar result to ours, with a total infertility prevalence of 7.8% to our 8.2% . However, these studies had primary and secondary infertility rates of 3.9% and 2.18% , while our data showed 2.76% and 5.47% , respectively[21].
Numerous risk factors contribute to female subfertility, and it is important to diagnose each carefully to treat patients appropriately[22]. Risk factors that vary between different regions include the population′s genetics, socio-economic factors, differences in government policy, health care, nutrition, age of the participants,and sexually transmitted infections. High sexually transmitted infections in the population contribute to secondary infertility[23].Our study shows that essential risk factors for infertility in Mongolia are the woman′s age, alcohol consumption, and rural living. In women, the quantity and quality of oocytes are known to decline with age, resulting in fecundity becoming clinically relevant by the mid-30s[24].
Interestingly our results showed a steady decline in fertility through the ages of 30-36, followed by a sudden spike, then plateauing until age 45. Another possible contributing factor for infertility increasing with age in women is that susceptibility to infection also increases with age. A Scottish fertility clinic study found that women over 35 years were more likely to be diagnosed with tubal factor infertility than younger women (OR 2.2, 95% CI 1.7-2.7)[25]. In a study conducted in Turkey, infertility was significantly higher among women aged between 35 and 49 years[26]. A study in China showed that increasing level of education was inversely correlated with a decreased risk of infertility[27]. This may be due to a link between higher levels of education, healthier lifestyles, and better healthcare.
Clinical studies definitively demonstrate the impact of obesity on the risk of subfertility[28]. Cohort studies showed an increased risk of anovulation in extremely heavy exercisers (>60 min/day). However,a vigorous exercise of 30-60 min/day was associated with a reduced risk of anovulatory infertility[29].
We attribute the higher rates of infertility in rural areas compared to urban areas due to limited access to healthcare. For instance, all six fertility clinics in Mongolia are located in Ulaanbaatar. Among the infertile women in our study, only 0.8% had undergone in-vitro fertilization (IVF) therapy, compared to China′s 5.6% IVF therapy and 29.4% traditional Chinese medicine rates[27]. Furthermore, only 14.3% of our infertile participants who received hormone therapy had poor access to advanced fertility treatment. Infertility is expected to change in populations over time.
A US National Health report showed that infertility fell from 8.5% in 1982 to 7.4% in 2002[30]. Further declines in infertility were seen in 2006[31]. These declines in infertility may be due to improved nutrition and general health of the population and improvements in assisted reproductive techniques. In Mongolia, we could not look for these trends as this was our first report, but we hope to conduct further studies on infertility in the future. Our study calls for further quantitative and qualitative research specifically designed to identify the causes of declining fertility, the socio-demographic and medical factors contributing to infertility, and the links between infertility and assisted reproductive techniques in Mongolia.
Our study also has several limitations. First, information about risk factors was self-reported data. Second, we set strict criteria for the inclusion of participants, such as whether they were married and had been with their husbands for 12 months.
In conclusion, in Mongolia, the average infertility rate is 8.2% ,similar to the average worldwide. We find that in Mongolia,infertility prevalence is significantly higher in rural communities.Our study shows the most significant risk factors for infertility are: age, alcohol consumption, and rural living. In addition, an unfavorable gynecological history and some diseases also pose a risk to fertility.
Conflict of interest statement
The authors declare no conflicts of interest.
Acknowledgment
We sincerely thank the Mongolian National University of Medical Sciences for its immense support. Furthermore, we thank the School of Bio-Medicine and the Department of Pathophysiology for their crucial advice and organization. Finally, we extend our appreciation to ZEPH (Young Pathophysiologists’ Club) for their contribution to the integrity of our survey.
Funding
This study was funded by the Mongolian National University of Medical Sciences’ Science and Technology Support Fund’s“Domestication of IVF technology in Mongolia project” (Fund protocol number: 2016/01).
Authors’ contributions
Tuvshinbayar Negdel performed manuscript preparation, data analysis, and literature search. Arigbukh Enkhbat, Badrakh Munkhbayar and Ariunaa Ganbold were responsible for data collection. Khantushig Bilegsuren and Carol W Readhead contributed to English langauge polish. Khuderchuluun Nanjid carried out statistical analysis. Lkhagva-Ochir Erkhembaatar,Erkhembaatar Tuduvdorj, and Munkhzol Malchinkhuu contributed to concepts and design. Odkhuu Enkhtaivan was responsible for concepts, design and manuscript preparation.
 Asian Pacific Journal of Reproduction2023年3期
Asian Pacific Journal of Reproduction2023年3期
- Asian Pacific Journal of Reproduction的其它文章
- Do not lose the moon while counting the stars: Conventional IVF versus add-on treatments
- Protein kinase inhibitors affect spermatogenic functions and blood testis barrier remodelling: A scoping review
- Buffalo anti-PDC-109 antibodies improve the semen quality profiles and in-vitro zona binding index and minimize the cryoinjury of sperm in cryopreserved buffalo semen
- Effects of a glyphosate-based herbicide on the oestrous cycle of rats
- Antifertility potential of leaves and seeds of Delonix regia in female rats
