Assessment of tear film parameters post-treatment with commercial eyelid cleaning wipes: a pilot study
Amal Aldarwesh, Ali Almustanyir, Raied Fagehi, Khalaf Alruways, Abdulaziz Bin Turki,Mansour Alghamdi, Muteb Khalaf Alanazi, Balsam Alabdulkader, Wafa Alotaibi, Mosaad Alhassan
Department of Optometry, College of Applied Medical Sciences, King Saud University, Riyadh 11433, Saudi Arabia
Abstract
· KEYWORDS: dry eye; lid wipes; tear break-up time; tear meniscus height
INTRODUCTION
Dry eye disease (DED) is a multifactorial condition that relies on the health and interaction of the lacrimal functional units to produce a healthy tear film, provide adequate eye lubrication, and maintain ocular surface integrity.Epidemiological studies have shown that the global prevalence of DED is approximately 5%-50%[1].This prevalence of DED increases with age, particularly in those over 40, and is more common among women than men[2].DED has a significant impact on visual acuity, which affects the quality of life of affected patients[3-4].Patients are classified as having aqueous deficiency due to lacrimal dysfunction or evaporative DED associated with meibomian gland dysfunction (MGD).However, some patients may present with both mechanisms[1].Several risk factors have been associated with a high incidence of DED, including a low blink rate, contact lens wear,nutritional deficiencies, hormonal changes, exposure to adverse environmental factors or systemic diseases, and administration of systemic medications[5].
Given its diverse etiologies and pathophysiological mechanisms,diagnosing DED is challenging.Nevertheless, well-established diagnostic procedures are used in clinics to assess the aqueous and lipid layers of the tear film and ocular surface health.This includes, but is not limited to the Schirmer test, fluorescein staining, tear break-up time, tear meniscus measurement, lid margin lipid assessment, and assessment of tear evaporation.Additionally, clinicians tend to use validated questionnaires to classify disease severity[6].
The total annual cost of DED care for 1000 patients approximately US$0.27, 0.78, and US$1.10 million in France,the United States, and the United Kingdom, respectively[7].The direct cost of treatment, including artificial tears,anti-inflammatory agents, punctal plugs, and nutritional supplements, is estimated at an average of US$783 per patient[8].Ophthalmic lubricants including artificial eye drops, gels, and ointments, are the first-line therapies.For the management of dry eyes associated with MGD, a stepwise approach is utilized.This includes the use of warming eye masks, the elimination of bacteria causing blepharitis through antibiotics, and maintaining eyelid hygiene using over-thecounter products like eyelid wipes.These wipes containing active ingredients[9]and characterized as hypoallergenic and preservative-free, play a role in effective eyelid care.However, for individual patients, chronic use of eyelid wipes has a financial cost[9-10].Eyelid hygiene reduces postoperative blepharitis and MGD following cataract surgery[11], consequently reducing the rate of cataract surgery cancellation attributable to blepharitis[12].Moreover, dry eye treatment was associated with obtaining the best postoperative outcome in patients who undergo corneal refractive surgery to correct myopia[13].
Two commercially available products are Systane?lid wipes (Alcon Laboratories, Inc, Fort Worth, TX, USA) and Blephaclean?(Laboratory Thea, France).Systane?contains purified water, polyethylene glycol derivatives for lubrication,surfactants like disodium laureth sulfosuccinate and cocoamido propyl amine oxide, along with preservatives and solvents such as benzyl alcohol and edetate disodium[14].Blephaclean?sterile wipes are impregnated with natural active ingredients including hyaluronic acid, Centella Asiatica, Isis Florentina,as well as retinyl palmitate (vitamin A) and surfactants[15].A three-month use of Blephaclean?has been proven to alleviate dryness symptoms in individuals with blepharitis and MGD[16].Potential reactions to both products may include burning,irritation, itching, eyelid swelling, allergic reactions, and possibly excessive dryness[14-15].The use of eyelid wipes effectively cleans the eyelashes and eyelid margins, potentially improving tear film stability.This study assesses the shortterm treatment effects of Systane?and Blephaclean?lid wipes on tear film parameters in dry eye patients without evidence of blepharitis or MGD.
SUBJECTS AND METHODS
Ethical ApprovalThis study was approved by the Institutional Review Board Subcommittee of Health Sciences Colleges Research on Human Subjects at the College of Medicine, King Saud University (approval letter number E-22-6609).Written informed consent was obtained from all participants, and the study adhered to the tenets of the Declaration of Helsinki(2013).
Research ParticipantsThis study enrolled 48 healthy participants aged 20-35y with a visual acuity of 20/20.Participants were excluded if they showed evidence of blepharitis or MGD, reported chronic ocular conditions, eye surgery, regular contact lens use, and the use of systemic medications well-known to impact tear film stability.These medications include but are not limited to non-steroidal antiinflammatory drugs, steroids, antihistamines, antidepressants,anxiolytics, proton pump inhibitors, and systemic isotretinoin[17].Initially, all patients completed a subjective self-reporting of the Ocular Surface Disease Index (OSDI) questionnaire.Subsequently, non-invasive tear break-up time (NITBUT),tear meniscus height (TMH), lipid layer pattern (LLP)were assessed.Individuals who scored 0-12 on the OSDI questionnaire, had NITBUT of more than 10s, a TMH>0.2 mm, and a normal or thick LLP were allocated to the non-dry eye group.Other participants who scored above 12 on the OSDI, indicative of mild, moderate, or severe eye dryness,and did not achieve the cut-off value of the NITBUT, TMH and had a thin LLP were categorized as dry-eye individuals.Based on these initial results, participants in each group were randomly assigned to either Blephaclean?or Systane?treatment.Participants were instructed to close their eyes and gently sweep their eyelids several times.After 5min of eyelid cleaning, the NITBUT, TMH, and LLP were repeated.The procedure is described below.
Ocular Surface Disease Index QuestionnaireThe OSDI consists of 12 items that assess dry eye symptoms and their effects on vision-related functions, with final scores ranging from 0 to 100.The score was calculated for each participant at the start of the experiment.Scores 0 to 12 indicate normal conditions, 13 to 22 suggest mild DED, 23 to 32 represent moderate DED, and scores greater than 33 indicate severe DED[18-19].
Non-invasive Tear Break-Up Time and Tear Meniscus HeightThe NITBUT and TMH were measured using the EASYTEAR view (EASYTEAR S.R.L., Via Maioliche,Trento, Italy).The EASYTEAR view is a practical and compact device that visualizes lipid-phase interference within the tear film.This device also measures NITBUT, TMH, and LLP.A cutoffof NITBUT than 10s was employed to indicate dryness, while a TMH value below 0.2 mm was considered indicative of dryness[20].
Lipid Layer PatternLipid layer patterns were evaluated for each participant based on images captured using EASYTEAR View+ (EASYTEAR S.R.L., Via Maioliche, Trento, Italy).The grading of lipid layer pattern (grades A, B, C, D, and E)followed criteria from a prior report[20].Grade A signifies a very thin layer with a lipid layer thickness of 13-15 nm, while E refers to a dense white-blue layer with variable colors and a lipid layer thickness 90-140 nm.
Statistical AnalysisData were inspected using the Shapiro-Wilk test to detect non-normality.Based on the normality of the data, NITBUT, TMH, and LLP levels before and after lid wipe treatment were compared using the pairedt-test or Wilcoxon rank sign test.Comparison between groups before and after the lid wipe condition for each parameter were made using the unpairedt-test or Mann-WhitneyUtest.The lid photo grading system was performed similarly to the other parameters; however, non-parametric tests were used to compare treatments and groups.
RESULTS
Participants DataThe study involved 94 eyes from 48 participants with a visual acuity of 20/20, including 23 normal subjects (8 males and 15 females; mean age, 23.1±3.5y) and 25 subjects with eye dryness (18 males and 7 females; mean age, 23±4.2y.Measurements were taken for both eyes in all participants, with the exception of two subjects for whom only the right or left eye was included due to time-constraints issues.Table 1 presents the average OSDI scores for the two groups.
The participants were randomly distributed into two lid-wipe treatments without sex consideration (Table 2).OSDI scores were similar between the two groups.However, participants with dry eye reported significantly higher OSDI scores than non-dry eye participants for both lid wipes (Table 2).
Effects of Lid Wipe Treatment on Dry Eye ParametersAll participants underwent assessment for NITBUT and TMH before and after the lid-wipe treatment (Table 3).The results revealed an improvement in all parameters after using both types of lid wipes compared to baseline levels.Specifically,there was an approximately 14%, and 23% increase in the NITBUT level for the non-dry eye and dry eye group,respectively in the Systane?group compared to 7% and 10%in the Blephaclean?treated groups.A smaller increase was observed in the TMH values in both treatments (Table 3).
Lid Layer PatternParticipants in both treatment groups partially completed the lid photo grading test.Specifically, only 9 non-dry eye subjects (18 eyes) in both treatments and 10 dry eye subjects (20 eyes) completed used Systane?lid wipes,while 10 dry eye subjects (20 eyes) used Blephaclean?lid wipes.The data comparison showed a significant improvement in the lid photo grading scales after treatment with the lid wipe(Figure 1, Table 4).
DISCUSSION
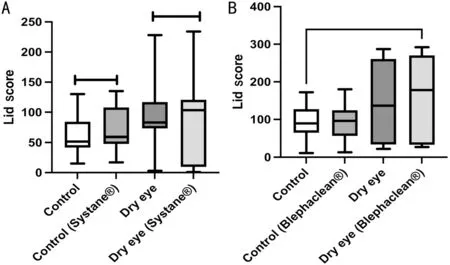
Figure 1 Side by side boxplots of the lid layer pattern (LLP, nm) for Systane?-treated (A), and Blephaclean?-treated (B) groups.
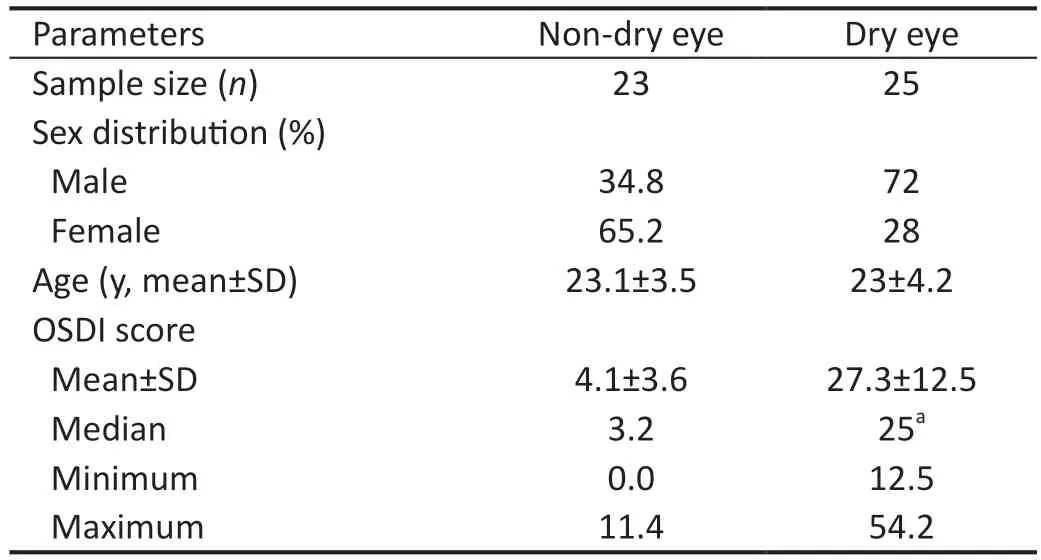
Table 1 Characteristic data for all participants
The primary objective of this cross-sectional research was to evaluate the immediate effects of lid wipes on the tear film quality and stability using Systane?and Blephaclean?eyelid wipes commonly used to manage blepharitis or evaporative DED induced by MGD.The study focused on individuals with dry eye symptoms, as indicated by OSDI scores and diagnostic tests, including NITBUT, TMH, and LLP, compared to non-dry eye individuals.However, it is important to note that this study did not investigate the presence of blepharitis or MGD in the recruited participants, nor did it explore the long-term effect of lid wipes on dryness, given that the wipes are widely used for purposes such as makeup removal and for daily eyelid and lash hygiene.This purpose is also advertised on the product's website and other retailers selling these products or similar ones used in the study.Additionally, contact lens wearers can use the product for overall eye care.On the other hand,in Riyadh city, where the weather is hot and dry most of the year, people use different products to manage eye problems.For some, artificial tears may not be the only way to relieve ocular dryness symptoms.Where some people find difficulties adhering to the drops, and the eyelid wipes are considerably more accessible.
In relieving the symptoms associated with DED has been investigated by many researchers.Various active ingredients have been proven to be effective for eyelid hygiene and control factors related to blepharitis or MGD usingin vivoandin vitromodels.Gostimir and Allen[9]examined the efficacy of various eyelid wipes and concluded that some of the types studied were effective.However, more evidence is needed to support long-term administration.Cheunget al[21]reported similar anti-demodetic activities of four commerciallyavailable eyelid cleansers with different active ingredients for managing blepharitis in an in vitro model.Moreover, evidence supports the use of cleaner-containing tea tree oils to manage blepharitis[22].Similarly, an earlier investigation by Guillonet al[16]showed that eyelid hygiene with Blephaclean?wipes significantly reduced the symptoms associated with blepharitis or MGD when used consistently for three months.
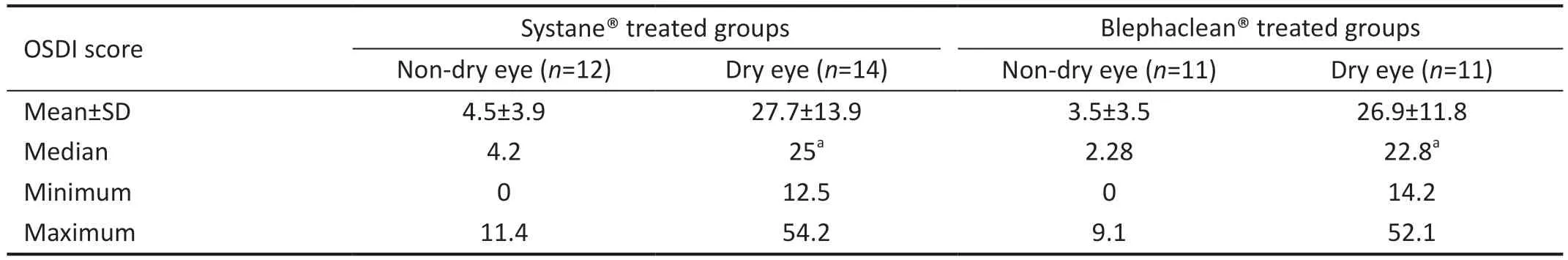
Table 2 Distribution of OSDI scores for research groups before treatment with lid wipes
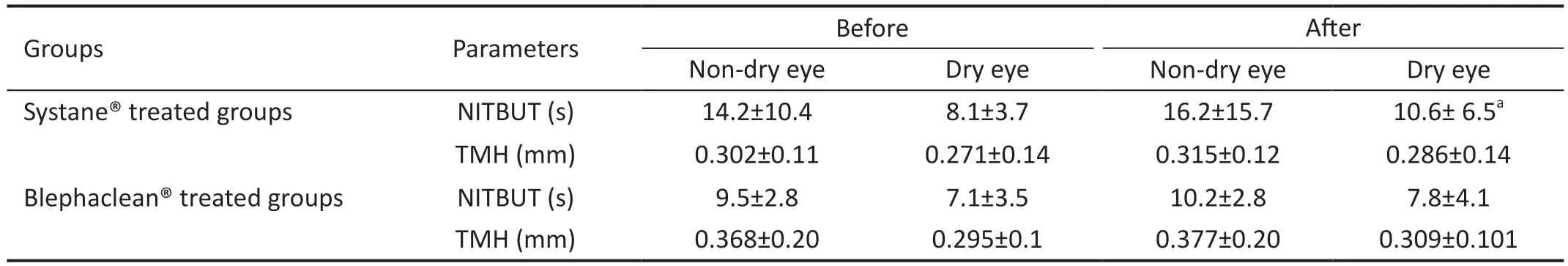
Table 3 Dry eye parameters before and after treatment with lid wipes mean±SD
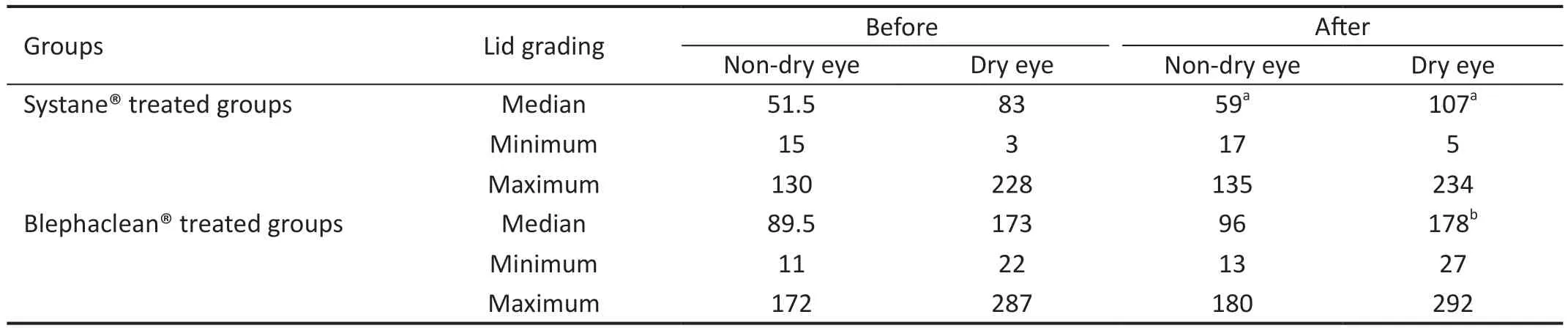
Table 4 Lid layer pattern grading system for participants before and after treatment nm
In the current study, both types of eyelid wipes improved tear film parameters, including NIBUT, and TMH, when compared to the dry eye status before treatment; however, they did not show an adequate trend of improvement compared to the nondry eye.This is in line with the findings of Rundaet al[23], who reported an improvement in tear film lipid layer thickness following the use of physiological detergent-free eyelid wipes without significant changes in NIBUT and TMH levels.Despite this, Systane?wipes exhibit a more favorable impact on the levels of these parameters compared to Blephaclean?.
Initial trials of Systane?demonstrated its effectiveness in alleviating the symptoms of DED, facilitating the ocular surface recovery and improving the NITBUT after one month of use but not affecting the TMH[24-25].Conversely, Wojtowiczet al[26]reported that a one-week application of systemic eye drop had no significant effect on the aqueous tear evaporation rate in patients with DED.
The Systane?lubricating eye drop comprises 0.4% polyethylene glycol 400, a component also presents in the Systane?eyelid,which forms mechanistically borate/hydroxypropyl guar gel crosslinks.These crosslinks extend retention time and maintain lubrication, safeguarding the ocular surface[27].This beneficial effect has also been reported with crosslinked hyaluronic acid for managing dry eye symptoms[28].
However, the action of the wipes is not intended to replicate the effects of the drops, given the differences in ingredients.However, the application method did not deliver these active compounds for an extended time on the ocular surface.Instead, the detergent effects of wipes on lashes and lids may alleviate the dryness symptoms.Instead, the detergent effects of wipes on lashes and lids may alleviate the dryness symptoms.This effect has been shown recently by Diaz-Vegaet al[29], who found that lid scrubbing with a gel combining natural extracts alleviates the ocular signs and symptoms of evaporative dry eye.The short-term impact of the lid wipes on NITBUT and TMH is expected to be augmented if patients use an appropriate ophthalmic lubricant.This method delivers a combination of vital components, including polyethylene glycol as a lubricant and sodium hyaluronate, a derivative of hyaluronic acid that has proven its efficacy in lubricating the ocular surface, prolonging NIBUT, and promoting epithelial healing[30-31].Moreover, short-term treatment with sodium hyaluronate temporarily increases the lipid layer thickness of patients with lipid deficiency one and five minutes postinstillation[32], consistent with the effect reported by our study.Furthermore, Blephaclean?is impregnated with the natural extract of Centella Asiatica, known for its antioxidant,anti-inflammatory, and healing properties on the ocular surface[33].However, our results show that Blephaclean?did not demonstrate the same level of improvement in tear film parameters as Systane?lid wipes.Thus, these findings need confirmation in a prospective study involving a larger cohort of patients with DED.The limitations of the current study include the small sample size and the disparity of sex distribution in the treatment arms.
In conclusion, the short-term effects of eyelid wiping on tear film parameters provide evidence supporting its benefits in patients with evaporative DED.However, the long-term impact of eyelid wipes must be investigated to support the use of these products and justify the cost of eyelid hygiene and relief of eye dryness symptoms in patients without blepharitis or MGD.
The future direction of this research is to combine of eyelid wipes with ophthalmic lubricants or other treatment modalities that mechanistically address the cause of dryness, such as blepharitis, MGD, or contact lens-associated dry eye, in largescale randomized trials.
ACKNOWLEDGEMENTS
Authors’ contributions:Conceptualization: Aldarwesh A,Almustanyir A, Fagehi R; Methodology: investigation and data curation, Alruways K, Bin Turki A, Alghamdi M; formal analysis: Alhassan M; writing: Aldarwesh A; review and editing: Fagehi R, Alanazi MK, Alabdulkader B, Alotaibi W;supervision, Aldarwesh A, Almustanyir A, and Alhassan M.All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest: Aldarwesh A,None;Almustanyir A,None;Fagehi R,None;Alruways K,None;Bin Turki A,None;Alghamdi M,None;Alanazi MK,None;Alabdulkader B,None;Alotaibi W,None;Alhassan M,None.
 International Journal of Ophthalmology2024年4期
International Journal of Ophthalmology2024年4期
- International Journal of Ophthalmology的其它文章
- Comment on: Recurrence after spontaneous separation of epiretinal membrane in a young woman: a case report
- When to repair a retinal detachment?
- Bilateral iridocorneal endothelial syndrome-Chandler’s syndrome: a case report and literature review
- Penetrating canaloplasty in corticosteroid-induced glaucoma: a report of two cases
- On-spot preparation of EDTA solution for the treatment of band keratopathy: a case report
- Non-contact wide-field viewing system-assisted scleral buckling surgery for retinal detachment in silicone oilfilled eyes
