Role of fractional fow reserve in guiding intervention for borderline coronary lesions
Xuekun Shi, Lu Cheng
Role of fractional fow reserve in guiding intervention for borderline coronary lesions
Xuekun Shi, Lu Cheng
Objective:This study investigated the clinical effcacy and value of fractional fow reserve (FFR) in guiding the treatment of borderline coronary lesions.
Methods:Forty-three patients with borderline coronary lesions, as demonstrated by coronary angiography, and who had FFR measurements were selected. The patients were grouped according to FFR values. All patients were evaluated 6 months after surgery to record major adverse cardiac events (MACE [sudden cardiac death, non-fatal myocardial infarction, or revascularization]) and recurrence of angina pectoris.
Results:After the 6-month follow-up, no sudden cardiac deaths or myocardial infarctions occurred in either group, and there were no statistically signifcant differences (P>0.05). Intergroup comparisons showed that in the groups with a FFR<0.75, the recurrence rate of angina pectoris in the PCI group was signifcantly lower than the drug therapy group (0.08% vs. 0.27%,P<0.05). In contrast, the recurrence rate of angina pectoris in the PCI group among the groups with a FFR<0.75 revealed no statistical signifcance when compared to the groups with a FFR≥0.75 (0.08% vs. 0.05%,P>0.05). The recurrence rate of angina pectoris in the simple drug therapy group among the groups with a FFR<0.75 was higher than the same groups with a FFR≥0.75 (0.27% vs. 0.05%,P<0.05).
Conclusion:When coronary intervention is used to treat borderline lesions, guiding interventional therapy with measurement of FFR does not increase the incidence of adverse cardiovascular events in the short term and can better guide PCI therapy.
Coronary intervention, Borderline lesion, Fractional fow reserve
Introduction
Coronary artery angiography (CAG) is the gold standard for clinical diagnosis of coronary heart disease. Borderline coronary lesions are defned as lesion with stenosis ranging from 50% to 70% based on visual inspection of coronary angiography [1]. Borderline coronary lesions are common in patients with stable angina pectoris and acute coronary syndrome [1]; however, coronary angiography can only provide an anatomic imaging evaluation regarding the degree of stenosis and characteristics of plaques, and is incapable of functionally evaluating whether or not the lesion can cause myocardial ischemia.
Considerable research has been completed on the functional evaluation of coronary arteries, and in 1993 the Dutchscholar, Nico Pijls, proposed the fractional fow reserve (FFR) as a new functional indicator to calculate blood fow of the coronary arteries by measuring coronary artery pressure [2]. The FFR is recognized internationally as the best method by which to diagnose the degree of stenosis of coronary arteries, select the optimal treatment strategy, and assess effcacy [3].
Subjects and methods
Forty-three patients with borderline coronary lesions (stenosis diameter=50%—70% by visual evaluation) based on coronary angiography performed between January and June 2013 at the Affliated Hospital of Traditional Chinese Medicine of Xinjiang Medical University and who had FFR measurements were selected. This group comprised of 24 men and 19 women with a mean age of 59.49±8.43 years.
Inclusion criteria
(1) Patients who were aware of the content of the examination and surgery and signed an informed consent form.
(2) Patients who accepted CAG, which confrmed a stenosis diameter of 50%—70% by visual evaluation and accepted FFR testing.
Exclusion criteria
(1) Patients who had a history of myocardial infarction (MI), CABG, or percutaneous coronary intervention (PCI).
(2) Patients who had an acute coronary syndrome (ACS) within 1 week.
(3) Patients who had left main coronary artery or diffuse lesions, primary and secondary myocardial hypertrophy, severe renal insuffciency, disturbances of blood coagulation, second or third degree atrioventricular block, or asthma.
CAG and FFR measurement
The standard Judkins method was adopted for CAG and the standard method was adopted for FFR measurement. A 6F guiding catheter with no side opening was placed through a radial artery sheath to push a 0.014-inch pressure wire to the coronary artery orifce. A correction was made to ensure that the pressure tested by the guiding catheter and pressure by the pressure wire were consistent, then the 0.014-inch pressure wire (the pressure receptor was 3 cm away from the top of the guiding wire) was sent to the distal target vessel (the receptor was located 3—4 cm from the distal lesion). The top of the guiding wire was maintained in the middle of the vessel lumen without touching the vessel walls. ATP (drug concentration=1 mg/mL; infusion speed (mL/h)=weight (kg)×8.4) was pumped continuously by an 18G trocar through the median cubital vein. The pumping was stopped after 1—2 min when the coronary target vessel was induced to the maximum bloodshot state, and the instrument automatically displayed the FFR value. The receptor of the pressure wire was withdrawn from the catheter after each lesion test, and the difference between the aorta arterial pressure (Pa) and the average pressure of the guiding wire (Pd) was verifed; thus, the presence of reality and reliability when the difference was within ±5 mmHg. For patients whose a FFR<0.75 and who needed further PCI, the FFR was re-measured after stent implantation. For patients with a FFR<0.90, dilation was performed after balloons were selected [4, 5].
Grouping
The patients were divided into two groups according to the FFR value, with 0.75 as the boundary value. Twenty patients with a FFR≥0.75 were divided into the delayed PCI treatment group; a total of 21 patients had a FFR value <0.75 and were randomly divided into 2 groups, with one group referred to as the simple drug treatment group (11 patients and drug treatment group in short) and one group referred to as the PCI+drug treatment group (12 patients and the PCI group in short). All patients accepted optimal medical therapy after surgery.
Observational indices
All patients were followed for 6 months after surgery to observe adverse cardiovascular events (sudden cardiac death [SCD], non-fatal MI, and revascularization) and recurrent angina.
Statistical analysis
Results
Baseline characteristics of study patients
The differences in gender, age, hypertension, diabetes, hyperlipemia, family history, and ejection fraction among the three groups were not statistically signifcant (P>0.05), as shown in Table 1. The differences in conventional drugs among the three groups were not statistically signifcant (P>0.05), as shown in Table 4.
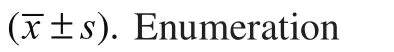
Comparisons of CAG parameters and FFR values
The differences in sites, reference vessel diameter (RVD), percentage angiostenosis, and minimum lumen diameter of vessel stenosis based on CAG among the three groups were not statistically signifcant (P>0.05), but the differences in FFR values were statistically signifcant (P<0.05). When a further analysis was performed on patients with a FFR<0.75, the difference between the PCI group and the drug treatment group by continuous comparison was not statistically signifcant (P>0.05), as shown in Table 2.
Comparisons of MACE and recurrent angina 6 months after treatment
No SCDs or MIs had occurred in any group of patients at the 6-month follow-up (P>0.05), but the incidence of revascularization differed among the 3 groups (P<0.05). The incidence of revascularization for patients in the drug treatment group among the groups with a FFR<0.75 was higher than the PCI and delayed PCI groups. The difference in recurrent angina among the three groups was statistically signifcant (P<0.05).The continued inter-group comparisons revealed that recurrent angina in the PCI group was lower than the drug treatment group (0.08% vs. 0.36%,P<0.05). The difference in recurrent angina between the PCI group among the groups with a FFR<0.75 and the delayed PCI group among the groups with a FFR≥0.75 was not statistically signifcant (0.08% vs. 0.05%,P>0.05). Recurrent angina in the drug treatment group among the groups with a FFR<0.75 was lower than the delayed PCI group among the groups with a FFR≥0.75 (0.36% vs. 0.05%,P<0.05), as shown in Table 3. In the PCI group among the groups with a FFR<0.75, 1 patient had recurrent angina and 1 patient had poor drug control; a recheck of the CAG indicated that the degree of stenosis of the original lesions was more severe than before. In the drug treatment group among the groups with a FFR<0.75, 3 patients had recurrent angina, among whom 2 had poor drug control; a recheck of the CAG indicated that the degree of stenosis of the original lesions was more severe than before and the lesions were relieved after stent implantation. In the delayed PCI group among the groups with a FFR≥0.75, 1 patient had recurrent angina and 1 patient had poor drug control, as shown in Table 4.

Table 1. Basic information of the 3 groups
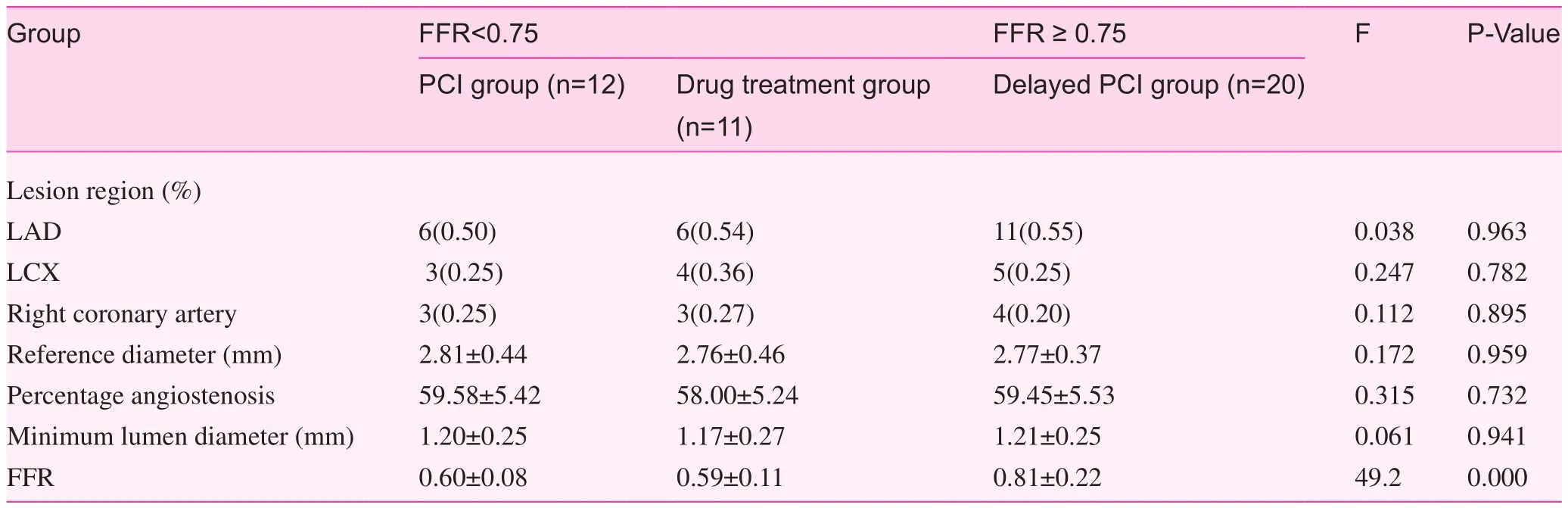
Table 2. Comparisons of CAG parameters and FFR values among the 3 groups
Discussion
FFR is defned as ratio between the maximum blood fow of the myocardium in a stenotic coronary-dominated region and the theoretical maximum blood fow which the myocardium can achieve in the same coronary artery [6]. The FFR is calculated as the ratio between the distal pressure of coronary artery stenosis (Pd) tested by a pressure wire and the aortic pressure (Pa) simultaneously tested by a guiding catheter (FFR=Pd/ Pa). Therefore, the FFR value is not subject to the infuence of blood pressure and heart rate, and has good repeatability and high accuracy, which makes the FFR feasible and reliable for clinical application [7].
The FFR has become an internationally-recognized functional index for the assessment of coronary artery stenosis.A FFR of 1 indicates normal blood vessels, while a FFR <1 indicates a vessel with stenosis. A FFR<0.75 suggests that the stenotic lesion may cause distal myocardial ischemia, thus positive intervention is recommended. A FFR>0.80 suggests the probability that distal myocardial ischemia caused by a stenotic lesion is low, thus delayed intervention and drug treatment is recommended. When the FFR is between 0.75 and 0.80, the therapeutic plan is determined based on a comprehensive assessment in combination with clinical manifestations [8].
Table 3. Comparison of MACE and recurrent angina 6 months after treatment among the 3 groups

Table 4. Comparison among the 3 groups with respect to drug application during the hospital stay and after 6 months of treatment
The DEFER study [9] involved a 5-year follow-up after PCI given to patients with a single stenotic vessel, the purpose of which was to evaluate the appropriateness of performing PCI on stenotic lesions without functional signifcance. The study enrolled 335 patients with coronary borderline lesions, but without evidence of ischemia and divided the patients into 2 groups (a PCI group and a delayed PCI group). In the delayed PCI group, PCI treatment was delayed and only drug treatment was given for a FFR≥0.75, and the patients were designated as the “defer group.” For a FFR<0.75, PCI was performed and the patients were designated as the “reference group.” In the PCI group, for a FFR≥0.75, PCI was performed and the patients were designated as the “perform group.”For a FFR<0.75, the patients were designated as the “reference group.” The prognosis among the defer, reference, and perform groups was compared. Clinical follow-up included the survival rate without cardiac events during the 5 years, and the results showed that the 5-year survival rate without cardiac events in the defer group was highest, followed by the perform and reference groups. The incidence of death and MI was 3.3% in the defer group, 7.9% in the perform group, and 15.7% in the reference group. For a FFR≥0.75, PCI treatment was much riskier and the survival rate was higher with respect to death and MIs. The study [9] showed that delayed PCI treatment for coronary borderline lesions in patients with a FFR≥0.75 is safe and feasible; specifcally, the annual risk for cardiac death or MI was <1% and would not be decreased by stent implantation. Therefore, intervention on myocardial ischemia-free coronary artery stenosis is futile; FFR plays a guiding role in determining whether or not coronary artery stenosis results in distal myocardial ischemia.
In addition to the above studies, using a FFR<0.75 as the standard for borderline lesions inducing myocardial ischemia, a series of studies [10—13] re-explored the guiding signifcance of this index in interventional therapy. One retrospective study [11] followed 100 patients who underwent delayed PCI (18±13 months) with a FFR>0.75, and the results showed that 2 died of non-cardiovascular events, 90 had no coronary events, and the average Canadian Cardiovascular Society (CCS) angina grading dropped from 2.0±1.2 to 0.7±0.9 (P<0.05), which indicated that it was safe to consider a FFR>0.75 as the boundary to defer PCI. Another prospective study [12] observed 107 patients with borderline coronary lesions as demonstrated by CAG, but without apparent myocardial ischemia on myocardial radionuclide imaging, among whom 92 were in the FFR≥0.75 group and 15 were in the FFR<0.75 group; an intergroup CAG indicated no apparent difference between the two groups with respect to severity of stenosis and no intervention treatment was conducted for patients in the 2 groups. At the 1-year follow-up evaluation, the incidence of patients in the FFR<0.75 group was higher than the FFR≥0.75 group (27% vs. 9%,P<0.05). The study confrmed that a FFR≥0.75 was also reasonable for delaying revascularization in multiple vessels with borderline lesions.
In addition, a FFR in the range of 0.75—0.80 remains a“grey area,” and a detailed and comprehensive assessment on coronary arterial conditions is required before making a decision on clinical treatment. Indeed, it is unclear whether or not PCI treatment is benefcial to improve prognosis in patients with a FFR between 0.75 and 0.80 [14]. A number of FFR-related studies have implied that physicians are more inclined to set a FFR of 0.80 [15, 16] as the cut-off value for deferring PCI. For 34 patients with a FFR between 0.75 and 0.80 who had not undergone vascularization treatment, the 1-year incidence of adverse cardiovascular events was 21% [16].
The FAME trial [17] compared the effcacy of FFR-guided PCI with CAG-guided PCI in CAD patients with multiple vessel lesions. Between January 2006 and September 2007, 1005 patients with multiple vessel lesions were included from 20 centers in Europe and the United States for PCI surgery. All patients had multiple vessel lesions (at least 2 branches of the 3 main coronary arteries had a diameter stenosis ≥50%) based on CAG and were considered to need PCI surgery.The patients were randomly divided into a CAG-guided PCI group and a FFR-guided PCI group. PCI was conducted for all lesions indicated by CAG in the CAG-guided PCI group, while in the FFR-guided group, the FFR was measured for all lesion-compromised coronary arteries and PCI was conducted on patients with a FFR≤0.8. The study endpoint was the 1-year incidence of MACE, including compound events of death, MIs, and revascularization. The secondary endpoint events included operative time, dose of contrast agent, and use of stents. The 1-year follow-up results showed that FFR-guided PCI could improve the therapeutic effect on patients; the incidence of MACE decreased by 30% in the FFR-guided PCI group and the number of stents placed in each patient decreased from 2.7 to 1.9. The material cost for each surgery was reduced by 11%. The dose of contrast agent was also reduced signifcantly, but the operative time was not extended. To understand the long-term clinical benefts, the FAME study released results from the 2-year follow-up and showed that the incidence of death and MI decreased by 34% in the FFR-guided PCI group and the incidence of MI dropped by 37% when compared to the CAG-guided PCI group [18]. Among the 513 lesions with delayed intervention, only 1 induced a MI and only 10 clearly progressed, requiring revascularization. These fndings affrmed the safety of performing delayed intervention for a FFR>0.8. The FAME study further showed a defect with respect to CAG; the measurement of FFR showed that among lesions with stenosis between 50% and 70% based on CAG, one-third of patients with ischemia were neglected. Moreover, among the lesions with a stenosis >70% based on CAG, 20% patients without ischemia were excessively treated. Among patients with 3-branch lesions based on CAG, measurement of FFR showed that only 14% had 3-branch lesions, 43% had 2-branch lesions, 34% had 1-branch lesions, and 9% of patients had no ischemia-induced changes.
The FAME II trial [19] was a prospective, multicenter, randomly-controlled clinical study that compared the clinical therapeutic effect on patients between FFR-guided PCI and optimal medical therapy (OMT), and observed the effcacy of using OMT to treat stable coronary heart disease. The participants of the study were patients with stable coronary artery disease who had 1-vessel, 2-vessel, or multiple-vessel lesions based on CAG and planned to undergo drug-eluting stent (DES) implantation. The FFR was measured in all patients, and patients with a FFR>0.8 were placed in the “register group” and treated with OMT. The patients with a FFR<0.8 were placed in the random “reference group” and distributed to the PCI+OMT and OMT groups with a 1:1 ratio. Clinical therapeutic effects were followed for 1 month, 6 months, 1 year, 2 years, 3 years, 4 years, and 5 years. The interim analysis results released by EuroPCR in 2012 showed that the FFR-guided PCI group had a risk reduced (>7-fold) due to the revascularization at admission and a risk reduced by (>11-fold) due to the emergency revascularization at readmission. When compared with the Clinical Outcome Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) [20], the FAME II trial provided new insight into the superiority of using FFR-guided coronary artery intervention. The COURAGE trial did not use a FFR measurement technique and did not demonstrate a difference between PCI+OMT and OMT based on clinical results. The FAME II trial overturned the results from the COURAGE trial in 2007 and proved that the effect of PCI+OMT was superior to that of simple OMT treatment, which not only relieved the symptoms, but also reduced MACE under the premise that the PCI was performed with the guidance of the FFR.
The FAME III trial [21] compared the long-term effcacy of FFR-guided PCI and CABG. The previous SYNTAX study [22] showed that CABG effcacy was better than PCI for high-risk patients whose SYNTAX was >33. However, after FFR functional SYNTAX scoring [23], 32% of the patients were re-divided from the original high-risk group into lower risk groups. Specifcally, 23% of the high-risk group was redivided into the medium-risk group and 15% into the low-risk group; 59% of the medium-risk group was re-divided into the low-risk group. By selecting the ischemic lesions with functional signifcance through FFR screening, then comparing the results of PCI and CABG, the groups were divided more precisely. The FAME III trial study compared the difference in long-term effcacy of FFR-guided PCI and CABG in patients with two- or three-vessel lesions (including the proximal segment of anterior descending branch or the left main artery), and it is believed that the results of this study will provide a more robust basis for the high-risk patients in the selection of PCI/ CABG strategies.
As shown in the analysis of this study, the FFR value was measured to determine whether or not to include PCI treatment; there was no increase in adverse cardiovascular events in the short term, and PCI treatment served as a better guide. Further, the results of the current trial, which are in agreement with several clinical trial results of these above-mentioned clinical trials as well as this study have demonstrated that FFR has a role in guiding interventional treatment of coronary artery disease.
Under certain circumstances, FFR was overrated because hyperemic reaction to the drug was poor in patients with severe left ventricular hypertrophy. Another example demonstrates that patients with ST segment elevation MIs should not have a FFR measured within 5 days of the MI. Therefore, when making treatment decisions, a comprehensive assessment of the clinical condition of the patient should be made in combination with relevant examinations. We also look forward to more high-quality clinical research to provide additional evidence for the better application of coronary FFR examinations.
FFR is currently an internationally-recognized functional indicator to evaluate coronary artery stenosis, and because of its features, FFR has high accuracy and repeatability. In the current study, the measured FFR values were taken as the gold standard for grouping, which affrmed the guiding role of FFR in the treatment of critical coronary lesions. The current trial had some limitations. Due to the small sample size and short follow-up time, the trial has not been extended. The number of domestic studies which have been conducted in this segment of cardiology is small, thus the application of FFR in interventional treatment needs further study. FFR can achieve functional complete revascularization and avoid unnecessary stenting, and hence we believe the application of FFR in China will become increasingly widespread.
Confict of interest
The authors declare no confict of interest.
1. Stone GW, Ellis SG,Cox DA, Hermiller J, O’Shaughnessy C, Mann JT, et al. One-year clinical results with the slow-release, polymer-based, paclitaxel-eluting TAXUS stent: the TAXUS-IV trial. Circulation 2004;109:1942—7.
2. Pijls NH, Van Son JA, Kirkeeide RL, De Bruyne B, Gould KL. Experimental basis of determining maximum coronary, myocardial, and collateral blood fow by pressure measurements for assessing functional stenosis severity before and after precutaneous transluminal coronary angioplasty. Circulation 1993;87(4):1354—67.
3. Kern MJ, Samady H. Current concepts of integrated coronary physiology in the catheterization laboratory. J Am Coll Cardiol 2010;55:173—85.
4. Zhang ZH, Yi Z, Wang B. Comparative analyses on assessment of coronary artery disease by fractional fow reverse under adenosine stress and ATP stress. Chin J Clinic 2012;6:61—4.
5. Luo YW, Zhang YC, Zhang XL, Gao YC, Chen F. Analysis on clinical experience in intervention of fractional fow reverse in coronary artery. J Clin Radiol 2011;30:1811—5.
6. Pijls NH, De Bruyne B, Peels K, Van Der Voort PH, Bonnier HJ, Bartunek J Koolen JJ et al. Measurement of fractional fow reserve to assess the functional severity of coronary-artery stenoses. N Engl J Med 1996;334:1703—8.
7. Melikian N, Cuisset T, Hamilos M, De Bruyne B. Fractional fow reserve-the infuence of the collateral circulation. Int J Cardiol 2009;132:e109—10.
8. Christou MA, Siontis GC, Katritsis DG, Ioannidis JP. Meta-analysis of fractional fow reserve versus quantitative coronary angiography and non-invasive imaging for evaluation of myocardial ischemia. Am J Cardiol 2007;99:450—6.
9. Pijls NH, van Schaardenburgh P, Manoharan G, Boersma E, Bech JW, van’t Veer M, et al. Percutaneous coronary intervention of functionally non-signifcant stenosis: 5-year follow-up of the DEFER Study. J Am Coll Cardiol 2007;49:2105—11.
10. Bech GJ, De Bruyne B, Pijls NH, de Muinck ED, Hoorntje JC, Escaned J, et al. Fractional fow reserve to determine the appropriateness of angioplasty in moderate coronary stenosis: a randomized trial. Circulation 2001;103:2928—34.
11. Lindstaedt M, Spiecker M, Perings C, Lawo T, Yazar A, Holland-Letz T, et al. How good are experienced interventional cardiologists at predicting the functional signifcance of intermediate or equivocal left main coronary stenoses? Int J Cardiol 2007;120:245—61.
12. Stone GW, Maehara A, Lansky AJ, de Bruyne B, Cristea E, Mintz GS, et al. A prospective natural-history study of coronary atherosclerosis. N Engl J Med 2011;364:226—35.
13. Ntalinis A, Sels JW, Davidavicius G, Tanaka N, Muller O, Trana C, et al. Fractional fow reserve for the assessment of nonculprit coronary artery stenoses in patients with acute myocardial. JACC Cardiovasc Interv 2010;3:1274—81.
14. Koo BK, Park KW, Kang HJ, Cho YS, Chung WY, Youn TJ, et al. Physiologic evaluation of the provisional side branch intervention strategy for bifurcation lesions using fractional fow reserve. Eur Heart J 2008;29:726—32.
15. Lindstaedt M, Yzazr A, Gerning A, Fritz MK, Holland-Letz T, Mügge A, et al. Clinical outcome in patients with intermediate or equivocal left main coronary artery disease after deferral of surgical revascularization on the basis of fractional fow reserve measurements. Am Heart J 2006;152:e1—9.
16. Legalery P, Schiele F, Seronde MF, Meneveau N, Wei H, Didier K, et al. One-year outcome of patients submitted to routine fractional fow reserve assessment to determine the need for angioplasty. Eur Heart J 2005;26:2623—9.
17. Tonino PA, De Bruyne B, Pijls NH, Siebert U, Ikeno F, van’ t Veer M, et al. Fractional fow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med 2009;360:213—24.
18. Pijls NHJ, Fearon WF, Tonino PAL, Siebert U, Ikeno F, Bornschein B, et al. Fractional fow reserve versus angiography for guiding percutaneous coronary intervention in patients with multivessel coronary artery disease: 2-year follow-up of the FAME Study. J Am Coll Cardiol 2010;56:177—84.
19. De Bruyne B, Pijls NH, Kalesan B, Barbato E, Tonino PA, Piroth Z, et al. Fractional fow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med 2012;367:991—1001.
20. Boden WE, O’Rourke RA, Teo KK, Hartigan PM, Maron DJ, Kostuk WJ, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 2007;356:1503—16.
21. Carr JA, Walt PE, Nakayama J, Fu YH, Corfeld V, Brink P, et al. FAME 3: A novel from of progressive myoclonus and epilepsy. Neurol 2007;68:1382—9.
22. Ong AT, Serruys PW. The synergy between percutaneous coronary intervention with TAXus and cardiac surgery (SYNTAX) study design, rationale, and run-in phase. Am Heart J 2006;151:1194—204. 23. Nam CW, Mangiacapra F, Entjes R, Chung IS, Sels JW, Tonino PA, et al. Functional SYNTAX score for risk assessment in multivessel coronary artery disease. J Am Coll Cardiol 2011;58:1211—8.
Affliated Hospital of Traditional Chinese Medicine, XinJiang Medical University, XinJiang 830000, China
Xuekun Shi
Affliated Hospital of Traditional Chinese Medicine, XinJiang Medical University, XinJiang 830000, China
E-mail: ruick0709@163.com
21 May 2014; Accepted 25 August 2014
 Family Medicine and Community Health2014年3期
Family Medicine and Community Health2014年3期
- Family Medicine and Community Health的其它文章
- Preparation of a questionnaire for disease knowledge-attitudepractice awareness of patients with remitted schizophrenia based on a structural equation model
- Association between esophageal cancer in middle-aged and elderly patients and body mass index and waist-to-hip ratio
- Relationship between obstructive sleep apnea-hypopnea syndrome (OSAHS) and liver fbrosis
- Relationship between fbroblast growth factor 21 and thyroid stimulating hormone in healthy subjects without components of metabolic syndrome
- Family Medicine and Community Health
- Family Medicine and Community Health COCHRANE UPDATES & NICE GUIDELINES
