Association of post-traumatic stress disorder and work performance: A survey from an emergency medical service, Karachi, Pakistan
Salima Kerai, Omrana Pasha, Uzma Khan, Muhammad Islam, Nargis Asad, Junaid Razzak4 Epidemiology and Biostatistics, Community Health Sciences Department, Aga Khan University, Karachi, Pakistan Community Health Sciences Department, Aga Khan University, Karachi, Pakistan
3 Psychiatry Department, Aga Khan University, Karachi, Pakistan
4 Emergency Medicine Department, Johns Hopkins University, School of Medicine, Baltimore, Maryland, USA
Association of post-traumatic stress disorder and work performance: A survey from an emergency medical service, Karachi, Pakistan
Salima Kerai1, Omrana Pasha2, Uzma Khan1, Muhammad Islam2, Nargis Asad3, Junaid Razzak41Epidemiology and Biostatistics, Community Health Sciences Department, Aga Khan University, Karachi, Pakistan2Community Health Sciences Department, Aga Khan University, Karachi, Pakistan
3Psychiatry Department, Aga Khan University, Karachi, Pakistan
4Emergency Medicine Department, Johns Hopkins University, School of Medicine, Baltimore, Maryland, USA
BACKGROUND: The purpose of the study was to explore the association between posttraumatic stress disorder (PTSD) and work performance of emergency medical services personnel in Karachi, Pakistan.
METHODS: Emergency medical service personnel were screened for potential PTSD using Impact of Event Scale-Revised (IES-R). Work performance was assessed on the basis of fi ve variables:number of late arrivals to work, number of days absent, number of days sick, adherence to protocol,and patient satisfaction over a period of 3 months. In order to model outcomes like the number of late arrivals to work, days absent and days late, negative binomial regression was applied, whereas logistic regression was applied for adherence to protocol and linear for patient satisfaction scores.
RESULTS: Mean scores of PTSD were 24.0±12.2. No association was found between PTSD and work performance measures: number of late arrivals to work (RRadj 0.99; 0.98–1.00), days absent (RRadj 0.98; 0.96–0.99), days sick (RRadj 0.99; 0.98–1.00), adherence to protocol (ORadj 1.01; 0.99–1.04) and patient satisfaction (β 0.001%–0.03%) after adjusting for years of formal schooling, living status, coping mechanism, social support, working hours, years of experience and anxiety or depression.
CONCLUSION: No statistically significant association was found between PTSD and work performance amongst EMS personnel in Karachi, Pakistan.
Emergency medical service; Karachi; Pakistan; Post-traumatic stress disorder;Stress; Work performance
INTRODUCTION
Work related stressors for people working in emergency medical service (EMS) range from exposure to critical incidents (like medical emergencies, natural disasters,and deceased children etc.) to chronic work conditions like supervisor or peer conflict, lack of support, etc.[1]Frequent and repeated exposures to these events in prehospital milieu can lead to stress reactions like posttraumatic stress disorder (PTSD).[1,2]Exposure to workrelated stressors has been found to be associated with post-traumatic stress symptoms amongst EMS.[2]Studies of PTSD among ambulance workers from developed countries (like Sweden, Canada, USA, U.K.) reports prevalence to be in range from 4% to 22%.[3–7]
Epidemiological data suggests that PTSD can have a wide range of outcomes from physical illness involving inflammatory diseases[8]to impairment in social and occupational functioning due to chronicity, comorbidity,somatization, substance abuse etc.[9]Among all consequences, work loss can be catastrophic because of its economic, social and emotional effect on individuals and families. A study by Breslau from Detroit showed that work loss among people with PTSD was higher as compared to those without any mental disorder (13.8 days vs. 1.86 days per capita per month).[10]Likewise,work loss days and loss of quality of life among European citizens increased with an increase in number of mental health disorders, where PTSD ranked top among ten physical and mental disorders associated with work days lost in one month.[11]These statistics show notable impact of PTSD on occupational functioning.Higher rate of missed working days among people with PTSD reflects potential repercussion for low income families, particularly for those who earn their livelihood through hourly wages or where an individual is the sole income provider of the family.
There is paucity of data on association of PTSD with an individual's job performance from EMS settings where vigilance and high level performance is demanded all the time and quality is judged by ability, knowledge,skills and attitude of workers.[12]Outcomes like poor performance can be more devastating in a resource scarce country like Pakistan, where those affected are from the young economically productive strata of the society. Therefore, we aim to measure the association of PTSD with work performance amongst EMS workers in Karachi, Pakistan.
METHODS
This cross-sectional study was conducted from January to June 2014 in a selected EMS setting of Karachi, Pakistan. The city consists of a network of different ambulance services that provide transport to hospitals with personnel having varying levels of training and skills. However, the study was carried out at "AMAN" EMS service in Karachi. This is the only service organization that has trained team members including doctor, nurses and technicians with lifesaving skills and equipment that provide basic and advance life support care during pre-hospital transportation.
EMS workers who have at-least three months of working experience in AMAN EMS, working in all three shift duties (morning, evening and night), and work as a fi eld staff (doctors, nurses, paramedics and drivers) were included in the study. This criterion was kept in order to have similar exposure in dealing with traumatic events.
PTSD measurement
Diagnostic and Statistical Manual of Mental disorders(DSM IV) criteria is used for defining PTSD which classifies PTSD as an anxiety disorder that occurs after exposure to a traumatic event.[13]In response, person exhibits intense fear, helplessness or horror.[13]For PTSD screening, a standardized tool, Impact of Event Scale-Revised (IES-R) developed by Weiss and Marmer was used.[14]It is based on three symptom cluster: avoidance,intrusion, and hyper-arousal based on criteria B, C and D of DSM IV.[13,14]It is a 22-item scale, response on each item represents the distress over event happened in past one week over a likert scale from zero to four, with zero representing the event never happened and four representing the event happened more than quite a bit.[14]Psychometric analysis of IES-R showed that a cut-off score of 33 had a diagnostic eff i ciency of 88%, sensitivity 91%, specificity 82%, positive predictive value 90%,and negative predictive value 84%.[15]Evaluation of the Urdu version of IES-R in Pakistan, showed satisfactory convergent validity and good reliability (cronbach's alpha 91.6% for internal consistency between Urdu and English version).[16]The scale has been used by Ehring et al[17,18]in their studies for PTSD screening in similar population in Pakistan; cronbach's alpha for their studies were more than 90%.
Work performance measurement
Individual employee work performance was assessed through organizational record by using personnel data.For comprehensive assessment of an individual's work performance, five measures i.e. number of late arrivals to work, number of days absents, number of sick days,adherence to protocol and patient satisfaction were assessed (Table 1 for description of these variables).Days absent from work, number of sick days and number of late arrivals to work were measured as distinct variables characterizing work performance because it was hypothesized that people who are stressed may come in late or call in absent or get sick more frequently as compared to their counterparts. Moreover, it was also postulated that those who are stressed might not be able to perform well which leads patients to be less satisfied.Questions for patient satisfaction survey was adopted from EMS department in Ohio, USA.[19]Questions were translated and adapted to local context. Adherence toprotocol is a task-based performance measure and was differently used for driver and medical personnel (doctors,nurses and paramedics). Adherence to protocol for drivers was measured as the number of vehicle crashes per month. Sub-variables for adherence to protocol for medical personnel are specified in Table 2. This task performance measure is assumed to be predictive of cognitive ability which tends to get disrupted during periods of stress. These variables have been adopted from the quarterly report card published from 12 National Health Service (NHS) Ambulance Trusts in U.K. and from 2007 consortium of US metropolitan municipalities'EMS medical directors.[20,21]
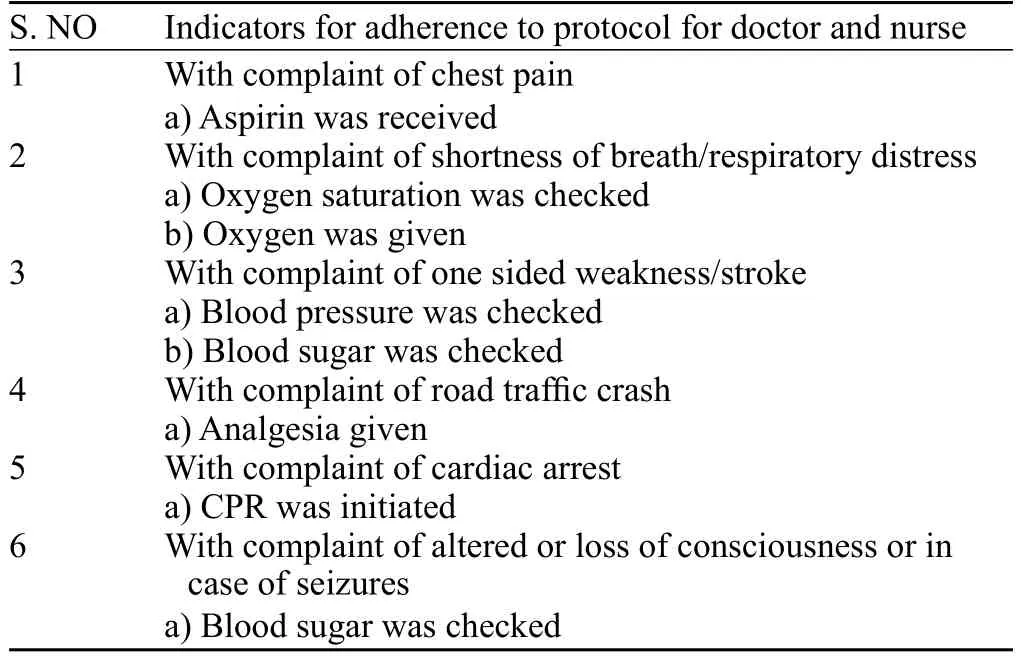
Table 2. Sub-variables for adherence to protoco
The time period for evaluating individual performance in this study was taken as three months. The three months was derived from human resource policy of probationary period for new job commencement which assumes that three months provides sufficient time to evaluate an individual's performance.
Covariates
Data on other variables were also collected, which presume to modify the relationship between exposure and outcome. Data on socio-demographic profile,occupational factors, personal and family history of stress were collected. In addition, coping styles were assessed by Brief-COPE (coping inventory)[22]and social support was assessed by Multi-Dimensional Scale of Perceived Social Support (MSPSS) which identifies the sources of support from family, friends, and significant others.[23]Furthermore, CAGE-AID (Cut-down,Annoyed, Guilty, and Eye-opener- adapted to include drugs) questions were used for screening of addiction to common substances[24]and AKUADS (Aga Khan University Anxiety and Depressions scale) was used for screening anxiety and depression.[25]
Data collection
Data collection was done in two phases. First phase was PTSD screening. Data on PTSD was collected on field sites by conducting in-person interviews by trained data collectors. Lists of people working in AMAN EMS were obtained from the field supervisors.Those who fulfilled the eligibility criteria and gave consent were included in the study. The second phase was data collection on work performance measures.For work performance measures (i.e. late comings,number of days absent and number of sick days), data was retrieved from institution attendance records which was maintained manually. Emergency call record forms were used to collect data on adherence to protocol and patient satisfaction. For collection of data on adherence to protocol for doctors, nurses and paramedics, relevant information from emergency call record forms was extracted on basis of customized questionnaire for all emergencies dealt 24/7 in three months' time. These record forms were also the source to get patient's contact information in order to conduct patient satisfaction surveys. The patient satisfaction survey was performed on a telephone call before which a verbal consent was taken from patient or next of kin who have utilized the ambulance service. Three attempts were made to establish contact in case the initial attempt to call was unsuccessful.The recall time of the survey call was utmost of seven days. Driving safety data for drivers was collected from fleet manager. Ethical approval was taken from Ethics Review Committee of Aga Khan University (2757-CHSERC-13). A written informed consent was also sought.
Sample size
A minimum of 468 individuals were required,in order to detect a minimum difference of 4 points(standard deviation of 11.5 points) in work performance of EMS personnel with and without PTSD, with power of 80% and alpha 5%. Total population working at AMAN EMS at the time of study was 536, which was very near to our calculated sample size. Therefore, all individuals fulf i lling inclusion criteria were invited to participate in the study.
Statistical analysis
Data were double entered in a tailored Microsoft Access database form. For statistical analysis STATA version 12 was used (Copyright 1985–2011 Stata Corp LP). All P values were two tailed with 0.05 as accepted level of significance. In order to examine data, exploratory data analysis methods were used.
Data reduction techniques were used in order to track work performance of individual employees. Data on late arrivals, days absent and days sick were treated as rare discrete events per three months' time period. We used negative binomial regression for these variables because data was over-dispersed and assumption of equality of the mean and variance was not met. Crude and adjusted rate ratios with corresponding 95% conf i dence intervals were reported. Data on patient satisfaction and adherence to protocol was converted into percentage scores in order to reduce variation in denominator. After scale examination, adherence to protocol was dichotomized in order to give meaningful interpretation. Logistic regression was used to model adherence to protocol:crude and adjusted odds-ratios (OR) with corresponding 95% confidence intervals were used for reporting.Linear regression was used for patient satisfaction score.Crude and adjusted beta coeff i cients with corresponding 95% confidence intervals were reported. Interaction,confounding and multi-collinearity was assessed. Model adequacy checks were performed for each model.
RESULTS
Information on 507 participants is included in final analysis (Figure 1).
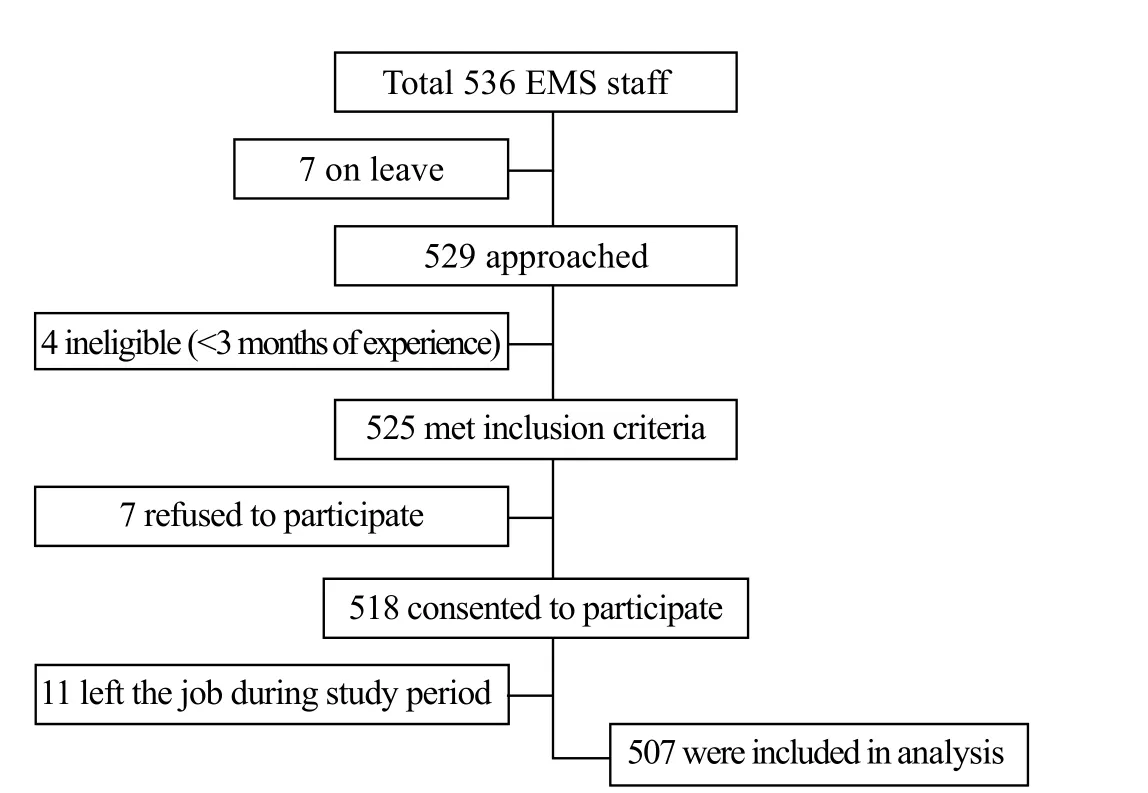
Figure 1. Study flow diagram.

Table 3. Characteristics of study participants, n (%)
Table 3 describes the socio-demographic profile of study participants. Out of 507 participants, 37 (7.3%)were doctors, 202 (39.8%) were nurses, 211 (42.6%)were drivers and the rest 57 (11.2%) were paramedics.All field staff members were male. The minimum age of EMS workers was found to be 22 years and maximum 53 years with most of them 336 (66.2%) having age in between 26–35 years. The majority of the participants were married and living with family. Average years of experience of EMS participants were 4±1 year/s and worked for 47.2±6.5 hours on average per week. Of note,most of them had an average monthly income from PKR 10 000 to 50 000 (USD 100–500). A total of 174 (34.3%)study participants reported use of substances like tobacco and betel nut. There were no social drinkers. The majority of the participants predominantly have problem focused coping with stress which is considered to be adaptive and constructive. Also, the majority of participants perceived to have social support of their family as ref l ected by highest average scores 22.6±4.8. Only 82 (16.1%) reported to have family history of psychiatric illness and only 27 (5.3%)reported to use medication to relieve stress. Moreover, 111(22%) of the participants were found to have PTSD while 28.8% had anxiety and depression on screening. The mean score for PTSD on IES-R in the study population was 24.0±12.2. The mean score for anxiety and depression on AKUADS was 15.6±8.2. Among those who have PTSD,68 (46.6%) also had co-morbid anxiety and depression on screening (data not shown).
Figure 2 depicts the distribution of outcome variables i.e. number of late arrivals to work, number of days absent, days sick, adherence to protocol and patient satisfaction on basis of PTSD.
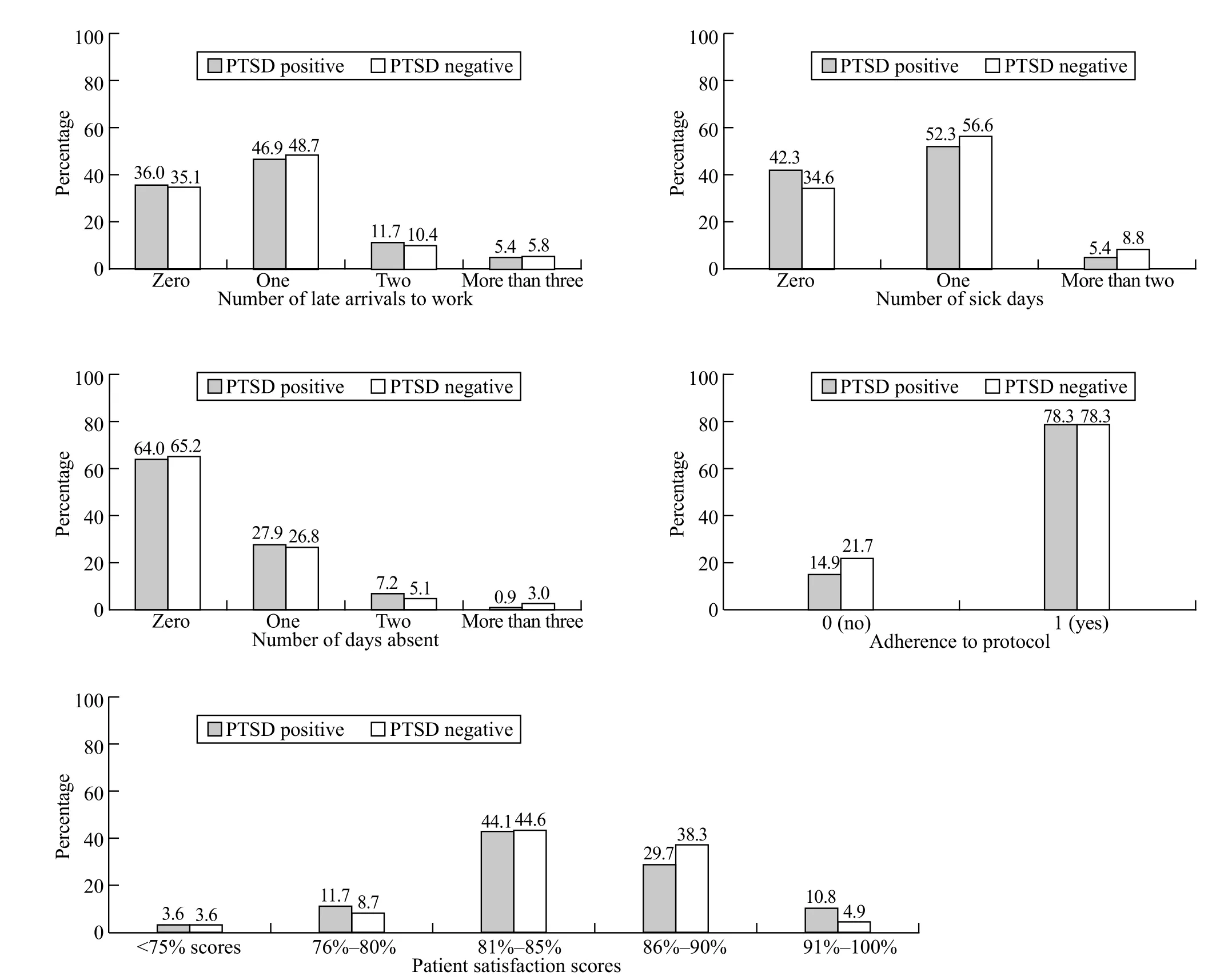
Figure 2. Bar graph for work performance variables.
Tables 4–8 show regression output for each of five outcome variables. Table 4 models the log of expected ratio of rate of late arrivals as function of predictor variables. It shows that PTSD is not associated with late arrivals to work (RRadj 0.99; 95%CI 0.98–1.00). On the other hand, the rate of late arrivals increases by 4%for each extra year of formal schooling. Also years of experience and working hours per week, increase the number of late arrivals by 17% and 2% respectively.In contrast, those who have the social support of their family are less likely to arrive late at work (RRadj 0.97;95%CI 0.94–0.99).
Table 5 shows estimated crude and adjusted rate ratios for days absent from work. It shows that participants who have PTSD, are less likely to remain absent from work (RRadj 0.98; 95%CI 0.96–0.99). On the other hand, the number of days absent increase by 78% for those who live alone if other variables like working hours per week, social support of family, anxiety and depression are kept constant. Likewise, days absent from work increase by 8% if a person has dysfunctional coping, which is a destructive and maladaptive way to cope with problems.
Table 6 reports estimated rate ratios for number of sick days. It shows that those who have PTSD, have only 1% tendency to call in sick which is very minimal. This infers that sick calls are not related to PTSD. Moreover,for every year increase in age, sick day call increases by 2% . Similarly, sick days increase by 38% for those who live alone without their families.
Table 7 models odds ratios for adherence to protocol.It indicates that employee adherence to protocol is not affected by their PTSD score (ORadj 1.01; 95%CI 0.99 to 1.04), while adherence to protocol decreased by 11%with increase in age. Increase in years of experience and formal schooling showed increase compliance to protocols by 48% and 39% respectively.

Table 4. Negative Binomial Regression for late arrivals to work (n=507)
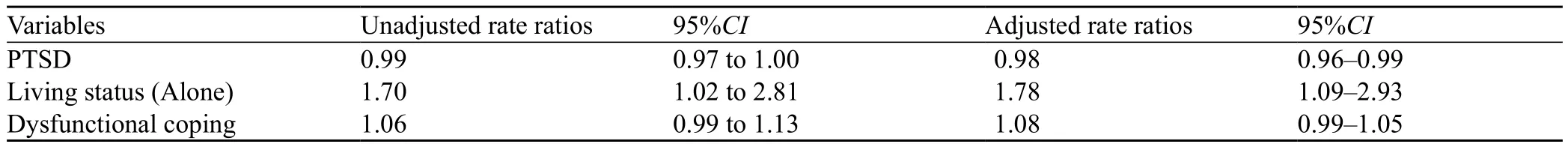
Table 5. Negative Binomial Regression for days absent from work (n=507)
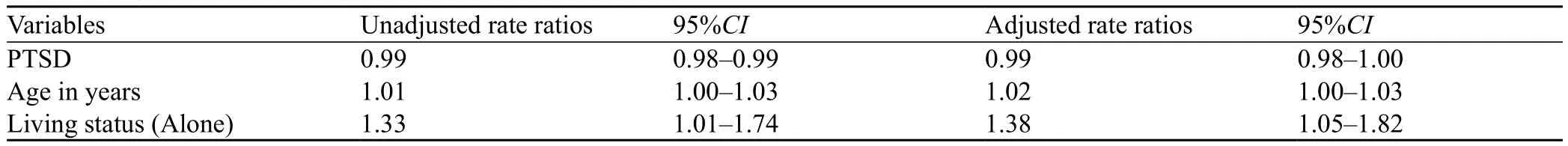
Table 6. Negative Binomial Regression for sick days ( n=507)
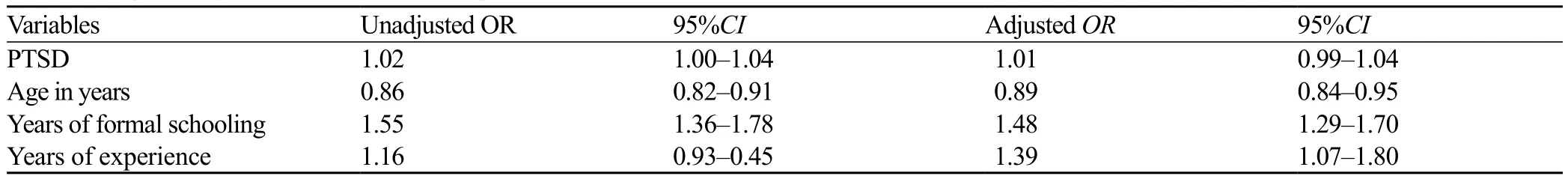
Table 7. Logistic regression for adherence to protocol (n=332)
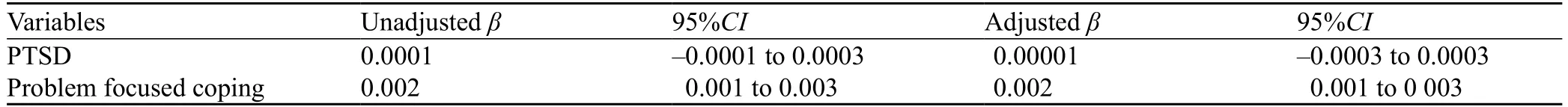
Table 8. Linear regression for patient satisfaction (n=502)
Table 8 estimates crude and adjusted beta coeff i cients for patient satisfaction. It highlights that there is no association of PTSD with patient satisfaction. Moreover,those employees who used problem focused coping strategy to deal with challenging situations provide higher patient satisfaction by 0.2%.
DISCUSSION
The study findings suggest an insignificant association between PTSD and worker's performance amongst EMS personnel in Karachi, Pakistan. This finding is in contrast with data reported from high income countries which indicates significant association of PTSD with work productivity loss. A study from New York showed significant association of PTSD with low quality of work days in people who witnessed the world trade center incident.[26]Detroit survey of trauma reports significant work loss of 11.4 (SE 0.6) days per capita in people with PTSD[10]and 2.4 (SE 1.06) days in full time workers from Australia.[27]These statistics reflect considerable variation in emotional reaction of stress on job performance. We believe our study results differ from these countries because of the difference in population and context. This study population solely comprises of EMS personnel working in pre-hospital setting from an urban metropolitan city which is home to people belonging to diverse ethno-linguistic backgrounds and culture. Family structure and cohesion, social support particularly of family and relatives, and problem focused coping (planning, seeking advice, actively seeking solutions) can be thought of as plausible factors enrooted in this culture and found in a greater extent of this study population as well that might have helped people to adapt to the wears and tears of tough occupational life.This phenomenon of resiliency needs to be explored in our EMS setting and requires further research. Moreover,part of the resiliency can be seen in personality traits of EMS workers which help EMS personnel to get self-selected into this profession. Qualitative inquiry is required to explore perceptions and feelings like willingness to go to work and readiness to carry out job responsibilities. These factors help the people stay on work despite adversities etc.
It was also observed in our study setting that personnel belonging to low and middle income families cannot afford to compromise on their work life since they are the only bread earner of the family and barely make ends meet. This behavior can be understood by taking into consideration psychology of scarcity which helped them positively adapt to their environment and perform well by focusing or tunneling their view. Literature shows that behaviors that appear harmful in the long-run in fact enable resilience and coping in the short-term.[28,29]Besides, it was observed that punitive outcomes such as salary deduction for absenteeism impaired performance at work. Consequently, people with adverse mental health are still coming for work to provide food for their families. Evidence shows that scarcity and low subjective status triggers narrowing of focus to process immediate and concrete information only, resulting in decisions that are "here and now".[29]These behaviors are assumed to be manifested as consequences of poverty and appears to be ecologically rationale in their context.[28]However,the displacement effect of stress on family and social life needs to be explored in this context.
Pakistan has some labor laws but there exist a lacunae in implementation of these laws to protect the workers from work place risks and hazards.[30]Also, the state falls short to fulfill the commitment for social protection and security to citizens.[31]This indicates the underprivileged state of workers in the country leaving employees unprotected to face the perils of occupational life.
AMAN Ambulance is a tiered ambulance service with a third of ambulances classified as advanced life support and 2/3rd as basic life support. Doctors and nurses with advance life support (ALS) training were deployed only on the ALS ambulances. When the service first began in 2008, ALS ambulances had physicians in the ambulances. In 2010, driven by diff i culty in recruiting physicians for ambulance service jobs, the service started to transition from doctors to nurses with ALS training,which is evident by their smaller number at the time of the study. At that time, doctors in ambulances were used primarily for critical care transport.
Work performance data has many utilities from an organization to individual standpoint. Researchers in the fi eld of organizational psychology are still grappling with the issues for assessing individual performance,which has no single answer. We have examined work performance measures used in various contexts and we attempted to synthesize different dimension that makes up the construct which is one of the approach to describe individual performance.[32]We did not attempt to assign score and weight to work performance variables.Transforming these five performance measures into a composite score requires another study and was out of the scope of this work and seems to be counterproductive in interpreting results. We used personnel level data from organizational records which are observable,countable, discrete data that prevents bias of subjective evaluation.[32]But the results may be affected by criterion contamination or deficiency which may occur due to factors beyond the control of individuals.[32]While there is need to assess the construct validity of these measures of work performance based on organizational records that were used. During information collection for work performance from emergency call record forms, we have assumed that all the information documented was correct and this is ref l ected by almost excellent agreement rates between treatment that was documented and recalled by patients (kappa agreement >0.8).
Limitations
For assessment of PTSD, clinician based diagnostic assessment is considered the gold standard but, due to limitation of resources, the screening tool (IES-R)was used which could have led to non-differential misclassif i cation of exposure that could have inf l uenced our results towards null. However, comparison of groups on basis of PTSD was internal i.e. based on exposure gradients; as no external population was selected which prevents confounding in estimates. The Cronbach's alpha for IES-R and AKUADS in our study sample was more than 0.80 which gives the evidence that scales were behaving reliably in the study.
We also suspect under-reporting due to the stigma attached to mental health problems, which might have led to under-estimation of PTSD symptoms in the study.Moreover, there is a possibility of length bias sampling;those who have symptoms for a long time would have been captured by the screening tool whereas those who spontaneously recovered from PTSD or left the job due to PTSD might have been left out of sampling. Other possible limitations include the use of CAGE-AID for screening alcohol and other drug use. This is a blunt tool on which possible responses are yes and no only.It can only give an idea about substance use but not about intensity or specific drug use. Also, there might be a problem of social desirability bias whereby people respond in a socially acceptable manner. However,the interviewer was unknown to the respondent; they were independent people who have no affiliation to the participating institution or with its mission or employees.Interviews were conducted in a private close room. No person from the institution has access to the logs of the participant other than the interviewers.
Generalizability is limited because this study was conducted in one institution where personnel were well trained and have the necessary lifesaving equipment to support life, so the findings should be interpreted with caution. However, we tried our best to use robust statistical techniques to obtain our estimates. Model adequacy checks were also found to be satisfactory.
Studies related to mental health are scanty in our part of the world. EMS is a relatively new concept in the Pakistani society and empirical research on EMS are also very few. Hence, studies assessing impact of mental health conditions on work life are very critical to assess here. To the best of our knowledge, this is perhaps one of the very few studies relating PTSD to work performance amongst EMS in low and middle income country like Pakistan.
CONCLUSION
Within our limitations, we can conclude that there is no association of post-traumatic stress with work performance measured by the number of late comings,number of days absents, number of sick days, adherence to protocol, and patient satisfaction in this setting.
ACKNOWLEDGMENT
I would like to acknowledge Dr. Eric Schneider for statistical analysis and AMAN EMS service for their support and participation in the study.
Funding: This work is partially supported through the Johns Hopkins-Pakistan International Collaborative Trauma and Injury Research Training program (grant number 2D43- TW007-292)from the Fogarty International Center of the United States, National Institutes of Health. The content is solely the responsibility of the authors and does not represent the views of Fogarty or NIH. This work is partially supported from department of Community Health Sciences, Aga Khan University, Karachi, Pakistan
Ethical approval: Ethical approval was taken from Ethics Review Committee of Aga Khan University (2757-CHS-ERC-13). A written informed consent was also sought.
Conflicts of interest: Funders have no role in study design,conduct or analysis of the study. Authors are responsible solely for the content and writing of paper.
Contributors: SK, OP conceived the idea, design the work,perform analysis and interpreted the data; MI assisted in analysis; UK, JR and NA helped conduct of study and assisted in interpretation of data; UK, MI, NA helped in drafting the work and revising it critically for important intellectual content; JR Final approval of the version to be published; all authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
1 Donnelly E, Siebert D. Occupational risk factors in the emergency medical services. Prehosp Disaster Med.2009;24(5):422–9.
2 Donnelly E. Work-related stress and posttraumatic stress in emergency medical services. Prehosp Emerg Care.2012;16(1):76–85.
3 Jonsson A, Segesten K, Mattsson B. Post-traumatic stress among Swedish ambulance personnel. Emerg Med J. 2003;20(1):79–84.
4 Misra M, Greenberg N, Hutchinson C, Brain A, Glozier N.Psychological impact upon London Ambulance Service of the 2005 bombings. Occup Med (Lond). 2009;59(6):428–33.
5 Mishra S, Goebert D, Char E, Dukes P, Ahmed I. Trauma exposure and symptoms of post-traumatic stress disorder in emergency medical services personnel in Hawaii. Emerg Med J.2010;27(9):708–11.
6 Sterud T, Ekeberg O, Hem E. Health status in the ambulance services: a systematic review. BMC Health Serv Res. 2006;6:82.
7 Bennett P, Williams Y, Page N, Hood K, Woollard M, Vetter N.Associations between organizational and incident factors and emotional distress in emergency ambulance personnel. Br J Clin Psychol. 2005;44(Pt 2):215–26.
8 Boscarino JA. Posttraumatic stress disorder and physical illness:results from clinical and epidemiologic studies. Ann N Y Acad Sci. 2004;1032:141–53.
9 Breslau N. Outcomes of posttraumatic stress disorder. J Clin Psychiatry. 2001;62 Suppl 17:55–9.
10 Breslau N, Lucia VC, Davis GC. Partial PTSD versus full PTSD:an empirical examination of associated impairment. Psychol Med. 2004;34(7):1205–14.
11 Alonso J, Angermeyer M, Bernert S, Bruffaerts R, Brugha T,Bryson H, et al. Disability and quality of life impact of mental disorders in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand Suppl. 2004;(420):38–46.
12 Sasser S VM, Kellermann A, Lormand JD. Prehospital trauma care systems. Geneva: World Health Organization, 2005.
13 Diagnostic and statistical manual of mental disorders: DSM-IVTR: American Psychiatric Association; 2000.
14 Weiss DS. The Impact of Event Scale: Revised. In: John P. Wilson CCS-KT, editor. Cross-Cultural Assessment of Psychological Trauma and PTSD: Springer Science & Business Media; 2007.
15 Creamer M, Bell R, Failla S. Psychometric properties of the Impact of Event Scale - Revised. Behav Res Ther.2003;41(12):1489–96.
16 Tareen MS, McDowell C, Naqvi K, Bashir A, Keenan P, Rehman Au, et al. The evaluation of an Urdu version of Impact of events scale - revised (UIES-R). International Psychiatry. 2012;9(1).
17 Razik S, Ehring T, Emmelkamp PM. Psychological consequences of terrorist attacks: Prevalence and predictors of mental health problems in Pakistani emergency responders.Psychiatry Res. 2013;207(1–2):80–5.
18 Ehring T, Razik S, Emmelkamp PM. Prevalence and predictors of posttraumatic stress disorder, anxiety, depression, and burnout in Pakistani earthquake recovery workers. Psychiatry Res.2011;185(1–2):161–6.
19 Bernard A, Lindsell C, Handel D, Collett L, Gallo P, Kaiser K, et al. Postal survey methodology to assess patient satisfaction in a suburban emergency medical services system: an observational study. BMC Emerg Med. 2007;7:5.
20 Myers JB, Slovis CM, Eckstein M, Goodloe JM, Isaacs SM,Loflin JR, et al. Evidence-Based Performance Measures for Emergency Medical Services Systems: A Model for Expanded EMS Benchmarking: A Statement Developed by the 2007 Consortium US Metropolitan Municipalities' EMS Medical Directors. Prehospital Emergency Care. 2008;12(2):141–51.
21 Deborah Shaw ANS. Report on National Ambulance Service Clinical Performance Indicators. UK: National Health Service NHS, 2012.
22 Carver CS. You want to measure coping but your protocol's too long: consider the brief COPE. Int J Behav Med. 1997;4(1):92–100.
23 Dahlem NW, Zimet GD, Walker RR. The Multidimensional Scale of Perceived Social Support: a conf i rmation study. J Clin Psychol. 1991;47(6):756–61.
24 Brown RL, Rounds LA. Conjoint screening questionnaires for alcohol and other drug abuse: criterion validity in a primary care practice. Wis Med J. 1995;94(3):135–40.
25 Karmaliani R, Bann CM, Pirani F, Akhtar S, Bender RH,Goldenberg RL, et al. Diagnostic validity of two instruments for assessing anxiety and depression among pregnant women in Hyderabad, Pakistan. Health Care Women Int. 2007;28(6):556–72.
26 Boscarino JA, Adams RE, Figley CR. Worker productivity and outpatient service use after the September 11th attacks: Results from the New York City terrorism outcome study. Am J Ind Med. 2006 Aug;49(8):670–82.
27 Lim D, Sanderson K, Andrews G. Lost productivity among full time workers with mental disorders. J Ment Health Policy Econ.2000;3(3):139–46.
28 Sendhil Mullainathan aES. Scarcity: Why having too little means so much. New York: Macmillan; 2013.
29 Sheehy-Skeffington J. Decision-making up against the wall:A framework for understanding the behavioural dimension of low socioeconomic status. In: S. Oishi & A. Uskul (Eds), The Socioeconomic Environment and Human Psychology. Oxford:Oxford University Press.
30 Mohammed F. Protecting Pakistani Laborers Post-Eighteenth Amendment: Recognizing Rights after the Devolution of Power. Loyola University Chicago International Law Review.2012;9(2):265.
31 Sayeed A, editor Social Protection in Pakistan: Concept,Situation Analysis and the Way Forward. Proceedings of a Joint Seminar Organized by the Planning Commission, ILO and UNDP on Employment-based Poverty Reduction Strategy for Decent Work in Pakistan Pakistan Institute of Development Economics Islamabad; 2004.
32 Viswesvaran C. Assessment of individual job performance:A review of the past century and a look ahead. Handbook of Industrial, Work and Organizational Psychology. 2001;1:110–26.
Accepted after revision April 15, 2017
Salima Kerai, Email: salima.kerai@aku.edu
World J Emerg Med 2017;8(3):214–222
10.5847/wjem.j.1920–8642.2017.03.009
October 28, 2016
 World journal of emergency medicine2017年3期
World journal of emergency medicine2017年3期
- World journal of emergency medicine的其它文章
- Emergency department procedural sedation for primary electrical cardioversion — a comparison with procedural sedations for other reasons
- The presenting and prescribing patterns of migraine in an Australian emergency department: A descriptive exploratory study
- Comparison of ultrasound-measured properties of the common carotid artery to tobacco smoke exposure in a cohort of Indonesian patients
- Validating a point of care lactate meter in adult patients with sepsis presenting to the emergency department of a tertiary care hospital of a low- to middle-income country
- Can patients with non-convulsive seizure be identif i ed in the emergency department?
- Study on the development and usage of a cardiopulmonary resuscitation time point recorder
