Clinical observation on electroacupuncture at four sacral points for overactive bladder syndrome
Li Rui-zhi (李瑞芝), Luo Jun-jing (羅珺璟)
Gonghexin Road Community Health Service Center of Jing’an District, Shanghai, Shanghai 200072, China
Overactive bladder syndrome (OAB) is a common disorder in middle-aged and older women. The frequent occurrence and long duration of OAB bring inconvenience to the patients. Under the instruction of Prof. Wang Si-you in Shanghai Research Institute of Acupuncture and Meridian[1-2], we treated 80 OAB cases with electroacupuncture (EA) at four sacral points and compared them with 40 cases treated with the conventional medication. The report is given as follows.
1 Clinical Materials
1.1 Diagnostic criteria
With symptoms of urinary urgency and frequency,incontinence and lower abdominal discomfort;repeated negative results in urine culture, routine urinalysis revealed no obvious abnormality; without organic lesions in the urogenital system or pelvic organs.
1.2 Inclusion criteria
Conforming to the above diagnostic criteria; female patients aged between 50-70 years; signed an informed consent form.
1.3 Exclusion criteria
Not conforming to the inclusion criteria; with serious cardiovascular, pulmonary, liver, kidney or hemopoietic system disorders; with mental diseases; patients who were afraid of acupuncture treatment and failed to cooperate with the treatment.
1.4 Drop-out, elimination and termination criteria
Drop-out criteria: patients who quitted or failed to follow the treatment course of their own accord.
Elimination criteria: patients who did not follow the experiment protocol or used other treatment privately.
Termination criteria: occurrence of serious adverse events or complications or rapid aggravation of symptoms.
1.5 Statistical method
All data were collected by Microsoft Excel 2003 and analyzed with SPSS version 15.0 software.Measurement data conforming to normal distribxutionwere described as mean ± standard deviation (±s),paired samplet-test was used for intra-group comparison, and independent samplet-test was used for between-group comparison; data not conforming to normal distribution was described as mean (the first quartile, the third quartile) [M (Q1, Q3)], Wilcoxon rank-sum test was used for intra-group comparison, and Mann-Whitney U test was used for between-group comparison. Between-group comparison of ranked data was done by Mann-Whitney U test. APlevel less than 0.05 indicated a statistical significance.
1.6 General data
A total of 120 female patients in our center were included between July 2014 and December 2015.Patients were allocated into a treatment group of 80 cases and a control group of 40 cases on a voluntary basis. In comparisons of the age, duration and symptom score before treatment, the differences were not statistically significant (allP>0.05), showing that the two groups were comparable (Table 1).
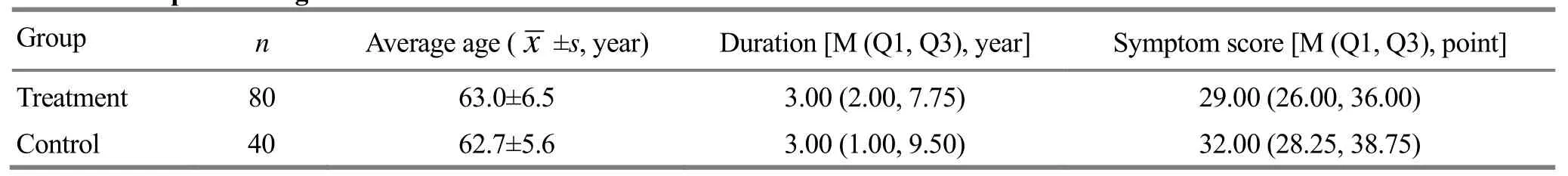
Table 1. Comparison of general data
2 Treatment Methods
2.1 Treatment group
Points: Four sacral points. The upper two points were located bilateral to the sacrococcygeal joint, while the lower two points were located 0.5 cun bilateral to the tip of the coccyx.
Methods:For the two upper sacral points, a long needle of 0.4 mm in diameter and 100 mm in length was inserted perpendicularly to a depth of 3.0-3.5 cun at each point, and then the needle was adjusted to transmit needle sensation to urethra and anus. For the two lower sacral points, a long needle of 0.4 mm in diameter and 100 or 125 mm in length was inserted obliquely to the lateral side (ischiorectal fossa) to a depth of 3.0-4.5 cun at each point, and the needle sensation was transmitted to urethra. When the sensation arrived at the targeted area, G6805 EA device was connected with continuous wave, 2 Hz in frequency,and a comfortable degree in intensity. Each treatment lasted for 60 min. During the treatment, the stimulation should radiate to urethral and periurethral area. The treatment was given 3 times a week, and the therapeutic evaluation was done after 6 consecutive weeks of treatment. If patients had obvious symptoms alleviation before the end of the whole course, the treatment could terminate in midway, and the data were recorded at the termination point and used as the statistical data.
2.2 Control group
Patients in the control group received M-receptor antagonist, oral administration of tolterodine tartrate,4 mg each time and once a day for 6 consecutive weeks.
3 Therapeutic Efficacy Evaluation
3.1 Observation items
The Symptom score was graded according to the Bristol lower urinary tract symptoms questionnaire before and after treatment[3-4]. Main items included daily frequency, urinary frequency, urgency, incomplete emptying, hesitancy, straining, urethra discomfort or pain, lower abdominal discomfort and frequency of leakage during urgency. Rating was based on the severity of symptom. The score of each item ranged from 0 to 5 points. The highest total score was 45 points.The higher the score, the severer the symptom.
3.2 Criteria of therapeutic effect
Symptom score reduction rate = (Symptom score before treatment - Symptom score after treatment) ÷Symptom score before treatment × 100%.
Cure: After treatment, Symptom score was 0 or the symptom score reduction rate was 100%.
Marked effect: Symptom score reduction rate ≥75%,but <100%.
Effective: Symptom score reduction rate ≥50%, but<75%.
Invalid: Symptom score reduction rate <50%.
3.3 Results
There were 3 cases whose symptoms all disappeared after 10 treatments in the treatment group, so their clinical data were calculated into statistical analysis.There were no drop-out cases in the control group.
3.3.1 Clinical efficacy
After 6 weeks of treatment, the total effective rate was 82.5% in the treatment group, versus 50.0% in the control group, and the difference in the total effective rate between the two groups was statistically significant(P<0.05), indicating a better effect in the treatment group (Table 2).
3.3.2 Symptom score evaluation
After 6 weeks of treatment, the intra-group changes in the symptom scores were statistically significant in both groups (bothP<0.01); the symptom score in the treatment group was lower than that in the control group, showed a statistical significance (P<0.01),indicating that the improvement of symptom score was better in the treatment group than that in the control group (Table 3).
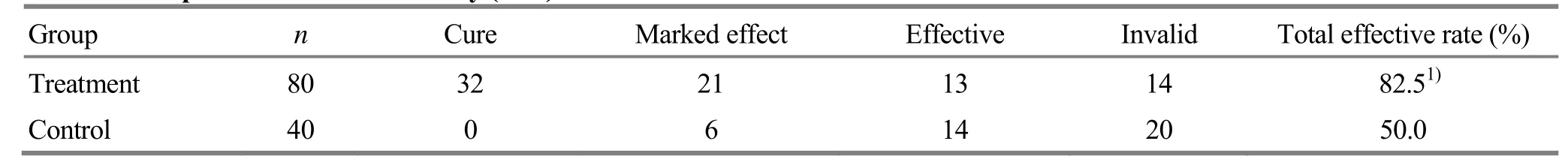
Table 2. Comparison of clinical efficacy (case)

Table 3. Comparison of symptom score [M (Q1, Q3), point]
4 Discussion
OAB refers to a series of symptoms characterized by lower urinary tract irritation (symptoms may include urinary frequency, urgency, difficult urination and superior pubic discomfort) without the presence of bacteriuria or other organic lesions in bladder and urethra. OAB has manifestations similar to urinary tract infection, which has symptoms of lower urinary tract irritation, while the laboratory and pathological examinations of urine, bladder and urethra reveal no obvious abnormality. According to its clinical manifestation, it belongs to qi strangury, fatigue strangury and difficult urination in traditional Chinese medicine. The location of OAB is the kidney and bladder,and nearly all patients show symptoms of kidney deficiency, including frequent, urgent urination and low back soreness. The frequent occurrence and long duration of symptoms gravely impact patients’ quality of life.
The pathogenesis of OAB still remains unclear. Li LK,et al[5]held that the storage and voiding of urine was directly influenced by pelvic floor muscles. Zhao L,et al[6]considered that OAB should be related to maldevelopment or degeneration of micturition center.When patients are affected by inducing factors, the elevated central nerve sensitivity or hyper-function can give rise to urinary symptoms. Research has shown that symptoms of OAB are also related to functional changes in pelvic muscles and nerves[7].
Various treatments have been developed for OAB at present. Behavior training has the advantages of low risk and good adaptability, but it requires patients to take large quantity of time and effort to reach the best therapeutic effect. Main Western medications, including M-receptor antagonist, estrogen, calcium antagonist and antidepressant, have the risk of adverse effect to impact the quality of life. Sacral neuroregulation is an invasive therapy and it causes infection easily. Surgery is also not widely accepted by patients for its traumatic nature. Traditional Chinese medicine therapy, such as acupuncture has a certain effect on OAB, but because of the individual difference, it is hard to form an uniformed therapeutic schedule[8-12].
Li WQ,et al[13]held that multiple pathogenic factors may coexist in OAB patients, including local anatomical abnormalities, low estrogen level, unstable bladder and mental stress. By comparison, the therapeutic effect of surgery treatment in restoring local anatomy and urethral morphology plus oral administration of tolterodine tartrate was superior than surgery alone or oral intake of medicine alone.
Meng P,et al[14]held that acupuncture had an obvious therapeutic effect on OAB. In the aspect of modern research, the optimal acupoints selection and treatment frequency are essential factors to achieve a good long-term effect.
Wang AC,et al[15]compared the clinical effect of three different methods on OAB, including bio-feedback assisted pelvic floor muscle training and electrical stimulation. The results showed that electrical stimulation had the best effect in relieving symptoms.Chen YL,et al[16]compared the clinical efficacy of electroacupuncture and manual acupuncture in treating female urethral syndrome. After treatment, the cure rate was higher in the electroacupuncture group. They further speculated that acupuncture could modulate sympathetic and parasympathetic nerves through nervous reflex, and then the interaction between bladder detrusor and urethral sphincter could be regulated to achieve the normal urine storage and voiding. Li LK,et al[17]believed that nerve and muscle stimulation could convert into electrical impulses, and further activated sympathetic nerve while inhibited parasympathetic nerve, thereby decreasing the intensity of bladder muscle contraction. That was the mechanism of electrical stimulation to pelvic floor muscles.
In this study, we used electroacupuncture at four sacral points to treat OAB. Such method was a combination of long needle acupuncture technique and electrical nerve stimulation approach in Western medicine. During the treatment, a sensation of obtaining qi should be kept around local tissue to conduct meridian qi to the affected region, and thus to regulate qi transformation function of bladder[18].Compared with conventional acupuncture, this method can directly stimulate pudendal nerve during treatment.During acupuncture, the needle tip can directly reach the vicinity of pudendal nerve. With electrical stimulation, sensory fibers of pudendal nerve can be stimulated to inhibit micturition reflex and overactivity of detrusor, and therefore can alleviate clinical symptoms.
The results showed that the therapeutic effect of electroacupuncture at four sacral points was superior to that of oral medicine. Compared with conventional acupuncture, this method is characterized by selection of few acupoints, convenience and good repeatability,and thus it is worth popularization.
Conflict of Interest
The authors declared that there was no potential conflict of interest in this article.
Acknowledgments
This work was supported by Medical Scientific Research Program of Jing’an District, Shanghai (上海市靜安區(qū)醫(yī)學(xué)科研課題, No. 2014zy05).
Statement of Informed Consent
Informed consent was obtained from all individual participants or their relatives in this study.
Received: 13 August 2017/Accepted: 15 September 2017
[1] Wang SY, Zhang SJ, Zhao L. Long-term efficacy of electrical pudendal nerve stimulation for urgencyfrequency syndrome in women. Int Urogynecol J, 2014,25(3): 397-402.
[2] Wang SY, Chen GM, Cui YJ, Zhang SJ, Zhang GF.Curative effect of special acupuncture techniques on female urethral syndrome and its relationship with the course of treatment. J Acupunct Tuina Sci, 2003, 1(3):19-21.
[3] Jackson S, Donovan J, Brookes S, Eckford S, Swithinbank L, Abrams P. The Bristol female lower urinary tract symptoms questionnaire. Br J Urol, 1996, 77(6): 805-812.
[4] Weiss JM. Pelvic floor myofascial trigger points: manual therapy for interstitial cystitis and the urgency-frequency syndrome. J Urol, 2001, 166(6): 2226-2231.
[5] Li LK, Song B, Jin XY. An experimental study on the influence of electrical pelvic floor stimulation to the goats’urethral function. Zhonghua Miniao Waike Zazhi, 2002,23(5): 307-308.
[6] Zhao L, Wang SY. Treatment frequency and long-term efficacy observation on electric pudendal nerve stimulation for stress urinary incontinence. J Acupunct Tuina Sci, 2013,11(3): 177-180.
[7] Xiong ZA, Zhu X, Chen SX, Chen ZJ, Zhang XJ, Li JH.Clinical observation on electrical stimulation on pelvic floor muscle on female urethral syndrome. Zhonghua Wuli Yixue Yu Kangfu Zazhi, 2005, 27(4): 213.
[8] Zhou Y, Ma Y. Syndrome differentiation and treatment of urethral syndrome. Shijie Zhongyiyao, 2015, 10(11): 1741-1744.
[9] Chai XH. Treatment of female urethral syndrome by‘Guifu Dihuang pill’ and ‘prostat tablet’ in 115 cases.Shanghai Zhongyiyao Zazhi, 2012, 46(10): 55-56.
[10] Jiao AG. Clinical observation on treating 90 cases of female urethral syndrome with Qingxin Lianzi Yin.Zhongyi Linchuang Yanjiu, 2014, 6(13): 95-97.
[11] Liu QH, Chen Y. Effects of integrated traditional Chinese and Western medicine for treating elderly female noninfectious urethral syndrome in 31 cases. Chongqing Yixue,2012, 41(14): 1366-1367.
[12] Chen ZW, Wang DJ, Yuan AQ. Therapeutic observation of acupuncture at Jiaji (EX-B 2) points plus pelvic floor muscle exercises for postpartum stress urinary incontinence.Shanghai Zhenjiu Zazhi, 2017, 36(3): 308-311.
[13] Li WQ, Zheng XM, Zhang L, Yang QS, Zheng H. The efficacy of different methods in treatment of female urethral syndrome. Yixue Xinzhi Zazhi, 2007, 17(1): 25-26.[14] Meng P, Wang SY. Research progresses on acupuncture for overactive bladder syndrome. Hunan Zhongyi Zazhi, 2014,30(1): 126-128.
[15] Wang AC, Wang YY, Chen MC. Single-blind, randomize trail of pelvic floor muscle training, biofeedback-assisted pelvic floor muscle training, and electrical stimulation in the management of overactive bladder. Urology, 2008,63(1): 61-66.
[16] Chen YL, Ha LF, Cen J, Huang QR, Hou WG, Gao ZQ.Comparative observation on therapeutic effects of electroacupuncture and manual acupuncture on female urethral syndrome. Zhongguo Zhen Jiu, 2005, 25(6): 425-426.
[17] Li LK, Song B, Zhang XH, Jin XY. Effect of pelvic floor stimulation on the bladder function in goats. Zhonghua Mixiao Waike Zazhi, 2000, 21(2): 738-740.
[18] Wang SY, Chen GM, Li LH. Study of ‘four sacral needles’therapy on female stress incontinence. Shanghai Zhenjiu Zazhi, 2006, 25(5): 15-17.
 Journal of Acupuncture and Tuina Science2018年3期
Journal of Acupuncture and Tuina Science2018年3期
- Journal of Acupuncture and Tuina Science的其它文章
- Influence of acupuncture on pulmonary function of patients with asthma: a review
- Observation on lower-reinforcing and upperreducing acupuncture method for hyperplasia of mammary gland and its influence on estradiol and progesterone
- Clinical observation on electroacupuncture plus hydro-acupuncture for low back pain caused by compression fractures
- Observation on clinical efficacy of warm needling therapy for chronic lumbar strain
- Observation on clinical effects of acupuncture plus external medicine application forcervical radiculopathy
- Effect of acupoint sticking at Shenque (CV 8) for preventing spleen-stomach disharmony caused by venous analgesia pump
