Comparative study for cardiovascular risk factors of rheumatoid arthritis and osteoarthritis
Cai-Ping Yue, Ming-Xi Li, Yan Liu, Fang-Kai Li, Xiao-Ping Liu, Jun-Fu Ma, Yue-Lan Zhu, Xiu-Juan Hou*Beijing University of Chinese Medicine, Beijing, China. Beijing University of Chinese Medicine Dongfang Hospital,Beijing, China. Capital Medical University Affiliated Beijing Rehabilitation Hospital, Beijing, China. Henan Province Hospital of Traditional Chinese Medicine, HeNan, China.
Abstract Objective: To compare the difference of cardiovascular risk factors in patients with rheumatoid arthritis (RA) and osteoarthritis (OA). Methods: A retrospective analysis was performed to compare the difference of cardiovascular factors between 44 patients with RA and 36 patients with OA in terms of their gender, age, body mass index, course of disease, carotid ultrasound related indicators, homocysteine, blood lipid levels, inflammation index, echocardiographic index, etc. Results: (1) General situation: there was no significant difference between two groups in terms of gender and age (P > 0.05). However, body mass index of OA group was significantly higher than that of RA group and the course of disease of RA group was significantly longer than that of OA group (P = 0.024). (2) Laboratory index: the level of homocysteine of RA group was significantly higher than that of OA group (P = 0.002). Though there was no significant difference between these two groups in terms of total cholesterol, triglyceride, low density lipoprotein, apolipoprotein B and high density lipoprotein (P > 0.05), the level of apolipoprotein A1 of RA group was significantly lower than that of OA group (P < 0.001) and the level of lipoprotein A of RA group was significantly higher than that of OA group (P <0.001). The levels of erythrocyte sedimentation rate and C reactive protein of group RA were significantly higher than those of OA group (P < 0.001). (3) Stroke volume and ejection fraction of echocardiography of RA patients were significantly lower than those of OA patients (P = 0.022, P = 0.009). However, there was no significant difference between two groups in terms of aortic diameter, left atrial diameter, left ventricular end diastolic diameter, left ventricular end systolic diameter, left ventricular posterior wall thickness, left ventricular fractional shortening, right ventricular diameter, right atrial diameter, and interventricular septum thickness (P > 0.05). Though significant difference in carotid artery plaque incidence between the two groups was not observed (P > 0.05), the incidence of carotid artery thickening and carotid artery middle thickness were significantly different between the two groups (P < 0.001). Conclusion: The rate for the occurrence of cardiovascular events in patients with RA was higher than those with OA. Additionally,effective control of RA patients’ conditions has the potential to reduce the risk of cardiovascular events.
Key words: Rheumatoid arthritis, Osteoarthritis, Cardiovascular risk factors
Background
Rheumatoid arthritis (RA), with the primary symptom of joint dysfunction, is a chronic and systemic autoimmune disease. Compared with other diseases, patients with RA suffer from higher mortality, which is closely related to the cardiovascular accident (CVA) [1-2]. CVA accounted for 42% of deaths in RA with patients and the incidence rate of CVA in patients with RA is 3.96 times than that of normal person.
Traditional risk factors such as hypertension, diabetes and dyslipidemia do not fully explain the cardiovascular condition of RA patients and about 34% of RA with patients has carotid atherosclerosis [3, 4]. Osteoarthritis(OA) is another joint disease that has the character of articular cartilage damage. There were a few studies about the effect of OA on cardiovascular diseases (CVD).Previous studies regarding RA or OA related CVD confined to biochemical indexes such as blood lipids,blood glucose, etc. and their therapy is limited to the usage of selective COX-2 inhibitors. However, few studies aim at the effects of non-traditional risk factors on the incidence of CVD, including inflammatory indexes,related indexes of echocardiography and carotid ultrasound. Some studies have shown that RA also acts as an independent risk factor for CVD. In this study, the CVD risk factors of RA and OA were compared from these non-traditional risk factors above.
Methods
Patient
80 cases of patients with RA or OA from the Department of Rheumatology, Dongfang Hospital, Beijing University of Chinese Medicine from October 2014 to December 2016 were recruited. They were respectively accorded with the diagnostic criteria of knee OA recommended by the American Rheumatism Society or 2010 ACR/EULAR Rheumatoid Arthritis Diagnosis and Treatment Standard.All cases were excluded from other diffuse connective tissue diseases, severe hypertension, diabetes and other metabolic diseases and inflammatory reactions.
Information
General conditions: Age, sex, body mass index (BMI),course of disease and therapeutic drugs.
Laboratory examination: Homocysteine (HCY), blood lipid related indexes, erythrocyte sedimentation rate (ESR)and C-reactive protein (CRP).
Ultrasound examination: Carotid ultrasound and echocardiography.
Statistical analysis
SPSS 17.0 software was used for statistical analysis. The measured data were expressed by mean ± standard deviation (± s), and the count data were expressed as frequency or rate. If the measured data were the normal distribution, the t test was used. If the measured data were the non-normal distribution, the rank sum test was used,and the count data using chi-square test. P < 0.05 was considered statistically significant.
Result
Baseline data
A total of 80 patients were enrolled, including 44 cases of patients with RA in which 34 persons for females and 10 persons for males as well as 36 cases of patients with OA in which 29 persons for females and 7 persons for males.There was no significance in gender and age between two groups (P > 0.05).The group of OA was significantly higher than the group of RA in the BMI (P = 0.018).However, the course of disease of RA group was longer than that of OA group(P = 0.024) (Table 1).
Comparison of the level of HCY and blood lipid
The level of HCY of RA group was significantly higher than that of OA group (P = 0.002). There was no significance difference between two groups in total cholesterol (TC), triglycerides (TG), low density lipoprotein (LDL), apolipoprotein B (Apo B) and high density lipoprotein (HDL) (P > 0.05). Apolipoprotein A1(ApoA1) of the RA group was significantly lower than that of the OA group (P < 0.001) while lipoprotein A (Lp A) was significantly higher than that of OA group (P <0.001). (Table 2)
Comparison of inflammation index
The RA group was significantly higher than the OA group in ESR and CRP (P < 0.001) (Table3).
Comparison of cardiac ultrasonographic indicators
The two groups in terms of aortic dimension (AD), left atrial diameter (LAD), left ventricular end diastolic pressure (LVD), left ventricular end systolic dimension(LVSD), left ventricular posterior wall thickness (LVPW),fraction shortening (FS), right ventricular internal dimension (RVID), right atrial diameter (RAD),interventricular septal thickness (IVST) showed no significant difference (P > 0.05). However, ejection fractions (EF) and stroke volumein (SV) of RA group were significantly lower than those of OA group (P =0.009, P = 0.022) (Table 4).
Comparison of carotid ultrasound
There were 14 cases (31.8%) without plaque, 26 cases(59.1%) with multiply plaque and 4 cases (9.1%) with single patch in RA group as well as 10 cases (27.8%)without plaque, 17 cases (47.2%) with multiply plaque and 9 cases (25.0%) with single patch in OA group,suggesting no significant difference between the two groups (P > 0.05). However, there were obvious differences in the terms of incidence rate of carotid intimamedia thicking, including 31 cases (70.5%) with carotid artery thickening and 13 cases (29.5%) with normal in RA patients as well as 23 patients (63.9%) with carotid artery middle-thickness thickening and 13 patients(36.1%) with normal in OA patients (P < 0.001) and carotid intimamedia thickness (IMT) of two groups (P =0.023) (Table 5).
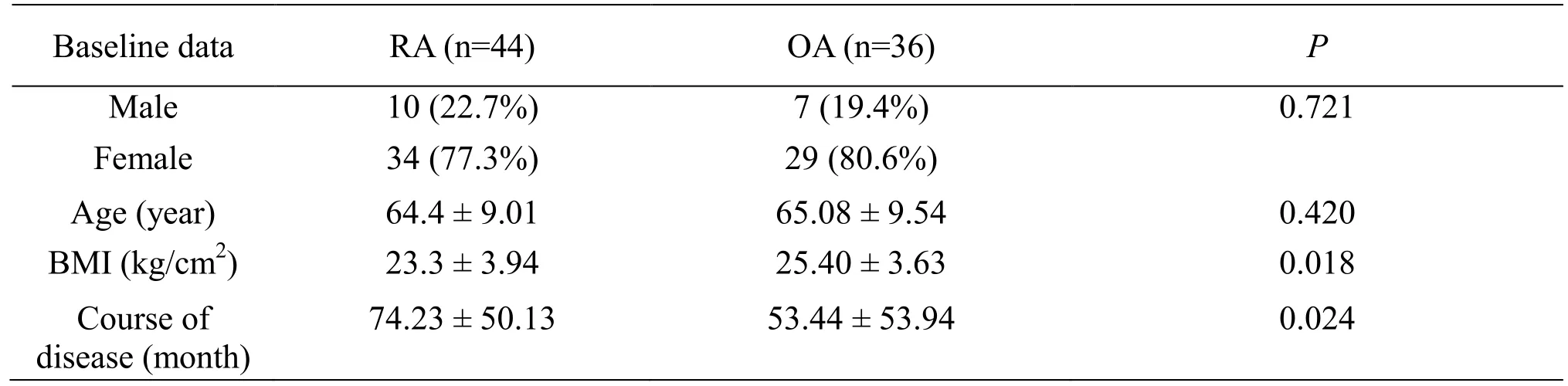
Table 1 Comparison of baseline data
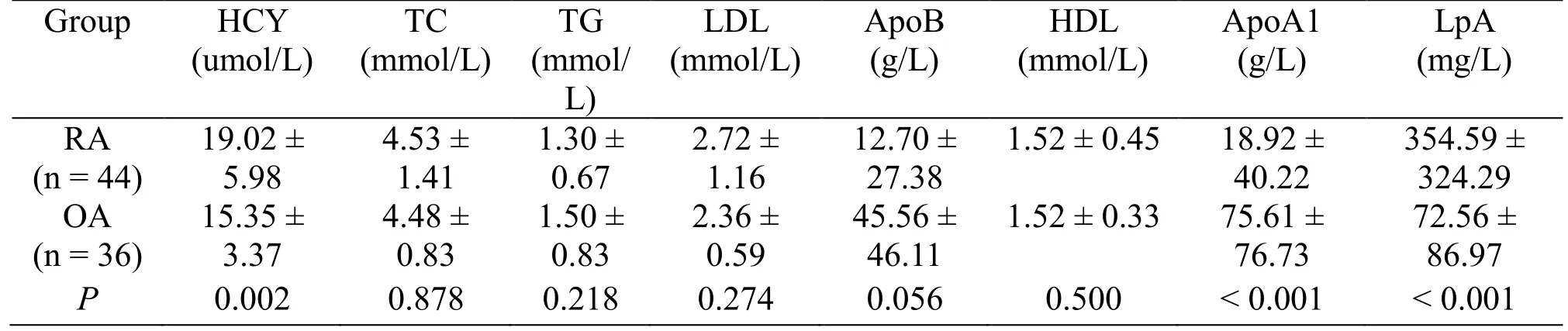
Table 2 Comparison of the level of HCY and blood lipid
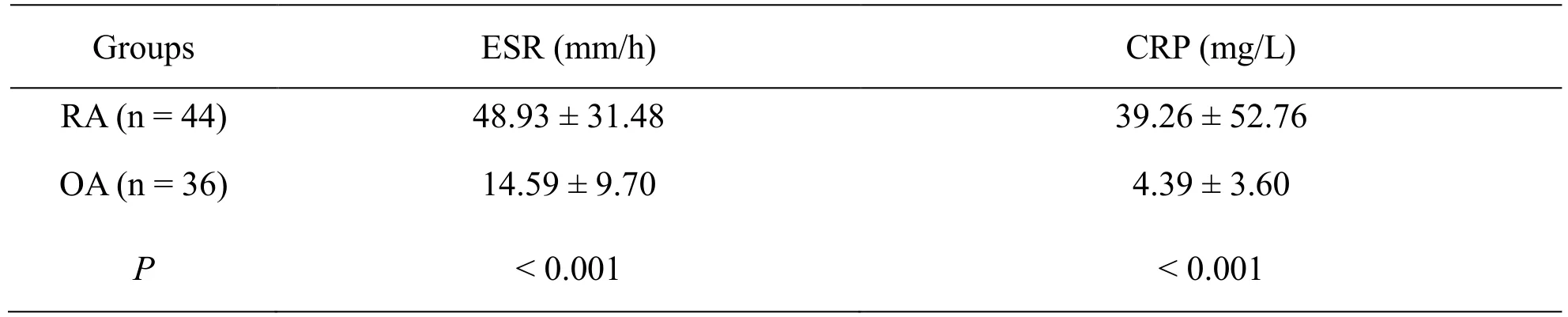
Table 3 Comparison of ESR and CRP
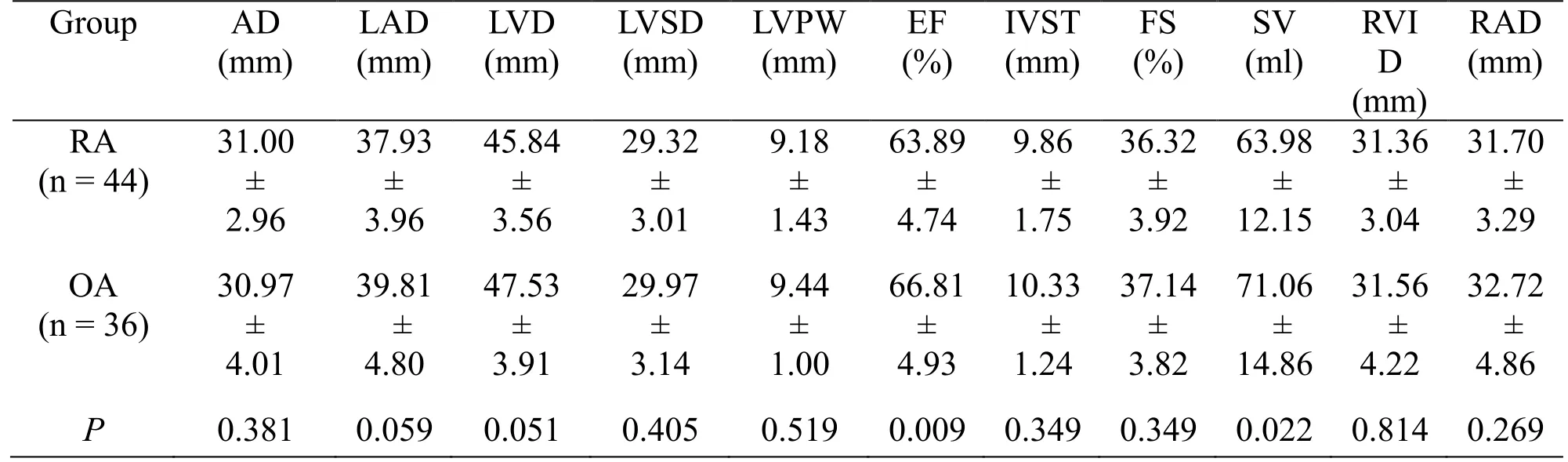
Table 4 Comparison of cardiac ultrasonography
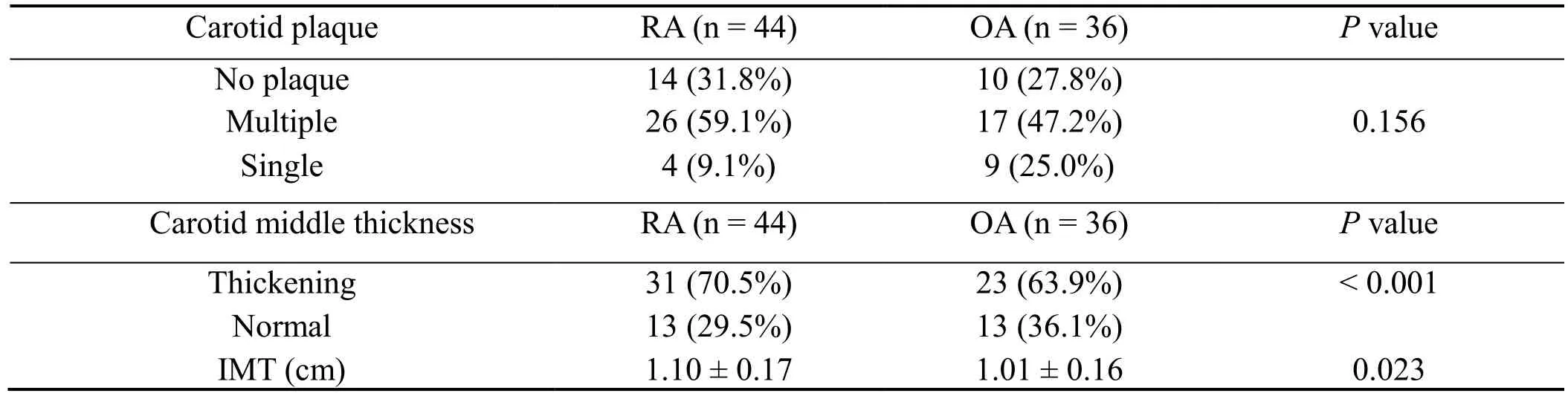
Table 5 Comparison of carotid ultrasound related indicators
Discussion
In recent years, a large number of studies have shown that RA was a risk factor for CVD, but the mechanism remains unknown. Studies have shown that RA is an independent risk factor for atherosclerosis [5].Cardiovascular risk factors for RA include traditional risk factors such as smoking, alcohol consumption, obesity,lipids, hypertension, diabetes, etc. and other non-traditional risk factors including inflammation and the usage of anti-inflammation drugs. Traditional risk factors are the primary risk factors for RA with CVD.However, the influence of non-traditional risk factors on CVD is unclear. Maybe the long-term chronic inflammatory response of RA and the usage of COX-2 inhibitors are involved in the occurrence of CVD. This study explores the possible cause from the following aspects.
Gender, age, course of disease and BMI
Studies have shown that the incidence of RA and OA in female were higher than those in male, in which estrogen maybe responsible for the protective effect on RA and OA[6-9]. This study also showed that most patients suffering from RA and OA are female, which is consistent with previous findings. There was no significant difference between the two groups in age and gender. The results of this study also showed that the course of disease of RA group was significantly longer than that of OA group, the underlying mechanism maybe that the young people are more prone to suffer from RA and in the situation of long-term chronic inflammation. In addition, high level of BMI increases the risk of CVD in the general population.However, for the patients with RA, the lower BMI, the higher risk of cardiovascular. The specific mechanism may be related to the RA patients’s cachexia characterized by decreased muscle mass and increased fat due to the chronic and progressive inflammatory response[10]. As showed in this study, BMI of OA patients was significantly higher than that of RA patients.
HCY and blood lipid levels
HCY can be used as an independent risk factor for coronary atherosclerotic heart disease [11]. It can result in CVD by increasing platelet aggregation or affect the function of endothelial cytoskeletal rearrangements and then destroy vascular endothelial cells [12-13]. However,homocystinemia is common in RA with patients.Compared with healthy people, the serum HCY level is significantly elevated in patients with RA, which is positive correlated with the activity of RA [14]. After exposure to treatment, the serum HCY level of patients was reduced, exhibiting the protective effect against CVD.
Dyslipidemia, one of the risk factors of CVD, is more common in RA patients, with the characteristics of high levels of TC, LDL, and Lp A as well as low levels of HDL and ApoA1 [15]. Nasr et al. found that Lp A is an independent risk factors of atherosclerosis. It has the potentials to destroy vascular endothelium in a concentration-dependent manner. The mechanism may be related to the process of inflammatory reaction in patients with RA. In this study, Lp A of RA patients was significantly higher than that of OA patients. ApoA1, one of the important components of blood lipids, is synthesized in the liver. Studies have shown that RA patients have significantly lower ApoA1 levels compared with those of the normal group and its mechanism may be related to liver damage caused by inflammation and antirheumatic drugs, which is consistent with the results of our previous study [16]. There is also emerging evidence that abnormal lipid metabolism in RA patients,with the primary character of high-density lipoprotein reduction, is closely related to the activity of RA disease[17]. However, the level of TC, TG, LDL, ApoB and HDL showed no significant differences between the group of RA and the group of OA in the present study.Maybe the small sample size and the medication history of patients should be responsible for it. RA patients include in this study were given anti-rheumatic drugs that have the regulatory effect on blood lipid [18].
Indicators of inflammation
Atherosclerosis is characterized by chronic inflammation and immune disorders. Inflammatory cells can lead to endothelial dysfunction and contribute to the reduction of arterial elasticity. As one of the main indicators of disease activity in RA patients, the elevated level of CRP can be regard as the key predictor of carotid atherosclerosis. The underlying mechanism maybe that CRP is capable of promote the expression of vascular endothelial cell surface adhesion factor, the secretion of monocyte chemotactic factor, and the aggregation of inflammatory cells by which accelerating the generation of foam cells[19-20]. Another study suggests that low level of CRP caused by the body's low-grade inflammatory response is responsible for the dysfunction of vascular endothelial[21]. Yu Shui Lian et al. found that the CRP levels of patients with early RA were significantly higher than those of normal people and positive correlation with BMI,blood pressure and other cardiovascular risk factors,indicating that down-regulation on inflammatory response in RA patient at early stage can effectively reduce the risk of CVD [22]. Besides, ESR is another index for evaluating the activity of RA, and is also involved in the progression of atherosclerosis. In this study, inflammatory index in RA patients were significantly higher than those in OA patients, which is consistent with results of previous studies that long-term chronic inflammation response could increase the incidence of cardiovascular events in patients with RA.
Echocardiography
Cardiac echocardiography is the imaging method for evaluating cardiac function. To evaluate cardiac function and structure, AD, LAD, LVD, LVSD, left ventricular short axis, SV, RVID, right atrial and interventricular septum thickness etc. were tested. Among them, the EF is related to the contractility of the myocardium, the stronger the myocardial contractility is, the greater the EF gets.
In a clinical report of 93 RA with patients, the incidence rate of left ventricular systolic and diastolic dysfunction was significant, accompanying with right ventricular diastolic dysfunction, systolic wall thicken and the decrease of myocardial compliance, suggesting that regular usage of echocardiography is helpful for the early detection of cardiac function impairment in patients with RA [23]. Guangxia Li et al. found that patients with RA were prone to suffer from atherosclerosis and high-frequency ultrasonography is suitable for the prediction, early diagnosis and guidance of clinical treatment in RA patients with atherosclerosis [24].
In the present study, there was no significant difference between the two groups in terms of AD, LAD, LVD,LVSD, LVPW, left ventricular short axis shortening,RVID, RAD, IVST, EF and SV. The small size sample and the limitation of study scope may be responsible for it.In addition, the included RA patients were all given the anti-rheumatism drugs that have a preventive effect on RA patients with CVD [25]. However, the EF and SV of RA patients were significantly lower than that of OA patients, which may be one of the causes of CVA and may be related to elevated blood HCY and the chronic inflammatory state.
Ultrasonographic aspects of carotid artery
The occurrence of carotid atherosclerosis is earlier than coronary artery atherosclerosis. Carotid atherosclerosis can involve the systemic circulation of large and moderate arteries and result in CVD [26]. The carotid artery color doppler ultrasonic examination can effectively reflect the severity of carotid atherosclerosis and provide some reference for predicting CVD [27]. It was found that both ESR and CRP were closely related to carotid atherosclerosis, and the incidence of atherosclerosis was higher than that of the healthy, which may be related to vascular endothelial injury caused by inflammatory reaction. This study also showed that there were differences between IMT and carotid thickening in patients with RA or OA respectively. However, more clinical trials with large sample are required to further explore it.
Conclusion
In summary, this study initially showed that patients with RA or OA have differences in cardiovascular risk factors.Serum HCY, Lp A, and inflammatory index of RA patients increase, while ApoA1 level decrease. There were also differences between RA and OA in EF, SV,carotid thickening and IMT, which further confirm that RA patients have higher CVD than OA patients.Therefore, monitoring the non-traditional cardiovascular risk factors of patients with RA helps to reduce the CVD.
- TMR Non-Drug Therapy的其它文章
- Acupuncture therapy in a patient with radial nerve injury
- Prone-positioned upside-done arch exercise, a kind of lumbodorsal muscles training,curbs the progression of lumbar disc bulge
- The beneficial effects of non-drug therapy on osteoarticular disease
- The clinical progress and potential mechanism of massage therapy on knee osteoarthritis
- TMR Non-Drug Therapy: the modernization of non-drug therapy

