Evaluation of therapeutic effects of self-made pelvic floor muscle rehabilitation on elderly female stress urinary incontinence
Wei Yuan
Evaluation of therapeutic effects of self-made pelvic floor muscle rehabilitation on elderly female stress urinary incontinence
Wei Yuan1, *
1Tianjin University of Sport, Tianjin 301617, China.
: Create a pelvic floor muscle rehabilitation program and explore its effects on stress urinary incontinence (SUI) in elderly women.: Pelvic floor muscle rehabilitation was created based on Kaigl experiment and pelvic floor muscle training methods. 20 elderly women aged 65-75 years with SUI were randomly recruited for 10 weeks of pelvic floor muscle rehabilitation. Self-control study was used to compare the 72-hour average frequency of urinary incontinence, the average score of urinary incontinence questionnaire-simple form (ICIQ-SF) of international urinary incontinence advisory committee, the severity index of urinary incontinence and the weight of 1 hour urine pad before and after rehibition.: After 10 weeks of pelvic floor muscle rehabilitation training, the 72-hour average frequency of urinary incontinence was 1.02 ± 0.65 times, which was not statistically different from that before training (1.25 ± 0.71,> 0.05). The score of ICIQ-SF was 5.95 ± 1.32, which was significantly lower than that before training (7.0 ± 1.38,< 0.05), and the urinary incontinence severity index was 2.75 ± 0.89, which was significantly lower than that before training (3.95 ± 1.32,< 0.01). The weight of 1 hour urine pad was 6.40 ± 2.29 g and was significantly lower than that before training (< 0.01, 8.37 ± 2.24).:Self-created pelvic floor muscle rehabilitation had the function of decreasing the quantity of urinary incontinence instead of the frequency of incontinence.
Pelvic floor muscle rehabilitation, Elderly women, Stress urinary incontinence
Self-created pelvic floor muscle rehabilitation was initially proved to have the function of decreasing the quantity of stress urinary incontinence (SUI) instead of the frequency of incontinence.
The self-created pelvic floor muscle rehabilitation training exercise, based on Kaigl experiment and pelvic floor muscle training methods, has the function of decreasing the quantity of urinary incontinence on SUI in elderly women, indicating the potential application prospects of non-drug therapy on SUI.

Introduction
The pelvic floor is a complex system composed of multi-layer musculo aponeurosis, urethra, vagina and pelvic floor muscle ligaments and nerves that close the outlet of the pelvis. Their interaction can support and maintain pelvic organs such as uterus, bladder, urethra and rectum in normal positions. Pelvic floor muscle dysfunction can cause uterine prolapse, urinary incontinence, fecal incontinence and other problems, of which urinary incontinence caused by pelvic floor muscle relaxation is a common disease among middle-aged and elderly women all over the world. Epidemiological investigations in Fujian, Wuhan and other regions of China showed that the incidence rates of urinary incontinence were 9.1%-46.5%, and the incidence rate was positively correlated with the growth of age. The incidence rate of urinary incontinence in elderly women (more than 65 years) was as high as 69% [1-3]. Urinary incontinence caused by pelvic floor muscle relaxation is detrimental to the personal hygiene and social image of elderly women. For elderly women with mobility disability or even paralysis, it will also increase the probability of bedsore, causing infection and discomfort. The problem of urinary incontinence not only affects the health of elderly women, but also attacks their self-esteem and self-confidence in life. The scores of anxiety, depression and other factors of female urinary incontinence patients, especially the elderly female patients, were higher than those of non-urinary incontinence patients [4-5]. In the long run, it will cause elderly female patients suffering from low self-esteem and even avoiding social contact.
There are no effective treatments for stress urinary incontinence (SUI). Pelvic floor muscle training combined with neuromuscular electrical stimulation (NMES) or surgery combined with drugs are mostly used. NMES and surgical treatments, such as retropubic bladder neck suspension and transvaginal bladder neck suspension, can significantly improve the symptoms and reduce the frequency of urine leaks [6]. However, the problems of them are too quick release and too short effective reaction time with many postoperative complications, which are not widely accepted. Therefore, pelvic floor muscle rehabilitation is the most widely accepted and safe treatment.
At present, traditional pelvic floor muscle rehabilitation training is limited to the movements of levator and pelvic floor muscle. However, the increase of abdominal pressure in elderly women is one of the causes of SUI. In order to strengthen the abdominal muscle of elderly women, coordinating abdominal breathing to adjust abdominal pressure, this study designed a set of rehabilitation exercises to enhance the pelvic floor muscle function based on Kaigl experiment and pelvic floor muscle training methods. 20 elderly women aged 65-75 years with SUI were randomly recruited for 10 weeks of pelvic floor muscle rehabilitations. Self-control study was used to compare the 72-hour average frequency of urinary incontinence, the average score of International Consultation on Incontinence Questionnaire-Simple Form (ICIQ-SF), the urinary incontinence severity index and the weight of 1hour urine pad before and after rehibition, so as to effectively improve the problem of SUI of elderly women.
Methods
Inclusion of indicators
(1) Older women aged between 65 and 75 years; (2) no accompanying symptoms such as urgency and frequency of urination; (3) according to the recommendation of the International Consultation on Urologyal Diseases on Women's Urine Time, Incontinence (4th Edition 2009), it meets the criteria for SUI: insufficient urine leaks out when abdominal pressure increases in various degrees such as laughter, cough, sneezing or walking, and stops with the cessation of actions; (4) accept the experiment voluntarily and consciously.
Exclusion indicators
(1) Patients with heart, lung, brain, liver, kidney and hematopoietic system diseases; (2) patients with urinary incontinence and pelvic floor surgery history; (3) patients with urinary system infection and organic diseases of urinary system; (4) patients taking drugs for urinary incontinence and receiving non-surgical treatment for urinary incontinence [Electroacupuncture stimulation, Pelvic floor muscle training (PFMT)] in the past two months; (5) patients with limited motor function; (6) patients with nervous system diseases or loss of consciousness.
Design and implementation of pelvic floor muscle rehabilitation
Exercise prescription design: (1) pelvic floor muscle exercise (modified PFMT): the subjects keep knees slightly apart, slightly lean forward, and natural keep levator movement for 8 beats, and then relax the waist after the body position restored for 8 beats [7]. Two eights in one group, exercise a total of four groups;(2) Kegel exercise: lie on back and bend knees with feet as wide as shoulders. Inhale at counting 1 2 3 4 and raise hips. Exhale at counting 5 6 7 8 and slowly return to the original position;(3) abdominal breathing training: the subject lies flat on the cushion with hands on abdomen. Inhales slowly counting 1 2 3 4. When inhale, the hand placed on abdomen are slightly lifted up with breath; exhales slowly at 5 6 7 8. Eight beats for one group, exercise a total of four groups; (4) abdominal muscle training I: turn with feet as wide as shoulders, holding a 1kg dumbbell (replaced by a 1.5 L mineral water bottle filled with water) in both hands behind the neck; turn the upper body to one side, when counting 1, 2 back to the original position, counting 3 back to the same side, counting 4 back to the original position. The second eight beats are a twist in the other direction. The two eight beats form a group of four;(5) abdominal muscle exercise II: bend knees and sit up, lie flat on back, bend legs, put arms behind neck and hold neck, keep shoulders about 35°off the ground with the command, and then return to the starting position. When counting 1, shoulders off the ground, counting 2 back to the original position, counting 3 shoulders off the ground, counting 4 back to the original position, and so on. Two eights in one group, exercise a total of four groups;(6) levator ani muscle exercise: the subjects sit on stools with feets crossed. Place hands flat on thighs and sit down alternately. Stand up alternately for one group at a time and repeat for 4 groups [8]; (7) repeat abdominal breathing training, adjust breathing and relax;(8) cough after getting up in the morning and buttock collection training: subjects cough gently after getting up, tighten buttocks and close anus. This method alternately relaxes or contracts and repeats 6-10 times; (9) when urinating, interrupt 2-3 times, so as to train the function of urethral sphincter.
The subjects can listen to soothing music when exercise to increase their exercise initiative.
Implementation of exercise prescription The subjects performed pelvic floor muscle rehabilitation 4 times a week for about 20 minutes each time. The subjects were reminded to train every other day by experimenter. The subjects were followed up by telephone.
Points for attention in exercise prescription implementation
(1) Before the experiment, confirm again that the subject has no cardiovascular and cerebrovascular diseases such as heart disease and hypertension. Educate the subjects, inform all subjects of the significance and purpose of the experiment itself, and ensure that each subject participates in the experiment voluntarily; (2) ensure that the training posture of the subject is correct and in place, and can independently complete the training of pelvic floor muscle rehabilitation except for items with auxiliary protection; (3) at the beginning of the experiment, the amount of exercise can be slightly reduced and gradually increased after one week of training; (4) items that need protection (for example, the exercise ball training of the subjects) must be carried out in an environment that ensures the safety of the subjects and the surrounding people; (5) in the experiment, nitroglycerin preparations such as quick-acting heart-saving and reserpine are prepared for cardiovascular; cerebrovascular drugs to prevent physical discomfort and accidents caused by changes in exercise quantity and exercise intensity of elderly subjects during exercise; (6) communicate well with the elderly subjects and encourage them to finish the exercise within the specified time, measurement and frequency. If they feel uncomfortable and unwilling to train, they can stop the experiment and let the subjects adjust; (7) prevent older people from increasing their physical activity by themselves. Once happen, the experimenter should immediately stop; (8) always ask the subject if they are unwell and have muscle or joint pain. If discomfort and pain occurred, the experimenter should look for the factors causing pain, and adjust the exercise prescription in time; (9) revision of exercise prescription:the experimenter should communicate with the subject on a daily or regular basis to find out the deficiencies in the experiment or where the subject feels uncomfortable, so that the experiment can proceed better.
Experimental tools
ICIQ-SF, urinary incontinence severity index, urine pad, electronic scales.
Main outcome measurements
The outcome measurements are the followings: (1) 24-hour average frequency of urine leakage: 72-hour average frequency of urine leakage divided by 3 is the 24-hour average frequency [9]. (2) ICIQ-SF Score. (3) Urinary Incontinence Severity Index Questionnaire: the product of the frequency of leaking urine and the amount of urine leaking [9]. (4) The weight of 1 hour urine pad: the amount of urine in the urine pad in 1 hour is measured to assess the severity of the urinary incontinence. The scheme is recommended by International Urinary Control Society. Before the experiment, ensure that each subject has no urine. The subjects drank 550 mL of mineral water after preparation and rested for about 1 hour after drinking. After the rest, let the subjects jog for 30 meters, and move up the steps from the second floor of the 1st corridor, lifting the heavy objects placed on both sides of the body. After the above exercise, the subjects went to the toilet to replace sanitary napkins and put them in disposable bags for the experimenter to weigh and record the data. ① weight gain of urine pad < 1 g indicates basic dryness; ② urine pad weight gain > 1 g is positive. Mild urinary incontinence: 1 hour’s leakage < 2 g. Moderate urinary incontinence: 2 g ≤ 1 hour’s leakage < 10 g. Severe urinary incontinence: 10 g ≤ 1 hour’s leakage < 50 g. Very severe urinary incontinence: 1 hour’s leakage ≥ 50 g.
Statistical analysis
The measurement data are expressed by the mean plus or minus standard deviation (`x ± s), and the mean comparison between the two groups is tested by two independent samples: Pairedtest was used to compare the mean of self-control before and after. Fisher test was used to compare the percentages of the two groups. SPSS 18.0 was used to collate and analyze the collected data, and the difference was statistically significant (< 0.05).
Results
Implementation and revision of exercise prescription
Twenty elderly female subjects were recruited (average height 161.10 ± 4.69 cm; the average body weight was 56.25 ± 6.73 kg. The average Body Mass Index (BMI) was 21.63 ± 2.07. The average age was 67.40 ± 4.48 years, all of them had a history of childbirth and met the diagnostic criteria for stress urinary incontinence. According to the feedback from the subjects, the exercise ball training in the pre-experimental prescription is not easy to implement. As the improvement rate of urinary incontinence can be improved by 70% by pelvic floor muscle exercise, which is an indispensable core training for SUI, the exercise ball training was changed to Kegel exercise. As during anal movement, alternating hands on both legs, alternating from sitting to standing, makes some subjects feel discomfort in the knee joint, the anal movement was reduced to two groups, and the anal movement was assisted during the inhalation of abdominal breathing.
Comparison of indexes before and after experiment
After 10 weeks of pelvic floor muscle rehabilitation, the 24-hour average urinary incontinence frequency was not statistically significant before and after the experiment [1.25 ± 0.71 vs 1.02 ± 0.65, (> 0.05)]. The score of ICIQ-SF, urinary incontinence severity index, and the weight of 1h urinary pad were significantly improved after the experiment. The score of ICIQ-SF decreased [7.0 ± 1.38 vs 5.95 ± 1.32 (< 0.05)], the urinary incontinence severity index decreased [3.95 ± 1.32 vs 2.75 ± 0.89 (< 0.01)], and HPTV decreased [8.37 ± 2.24 vs 6.40 ± 2.29 (< 0.01)], all with statistical significance (Table 1, Figure 1).
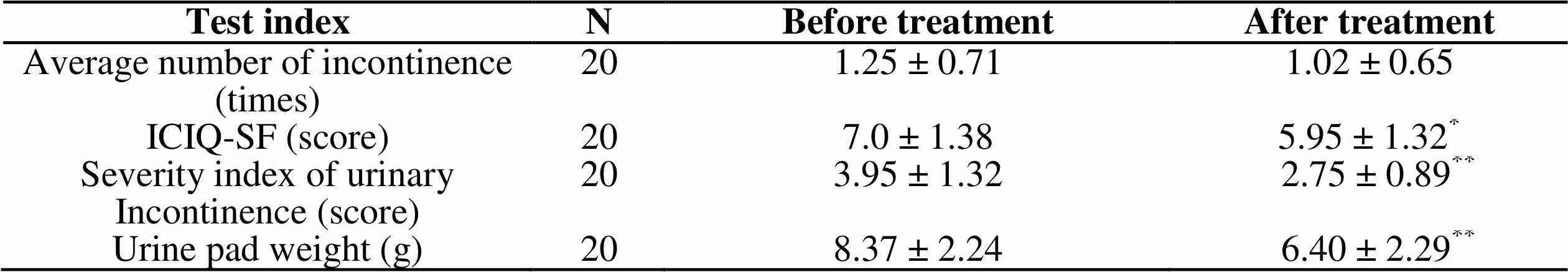
Table 1 Comparison of indexes of elderly female SUI subjects before and after experiment (`x ± s)
Note: ICIQ-SF, International Consultation on Incontinence Questionnaire-Simple Form. Compared with before the experiment,*< 0.05,**< 0.001
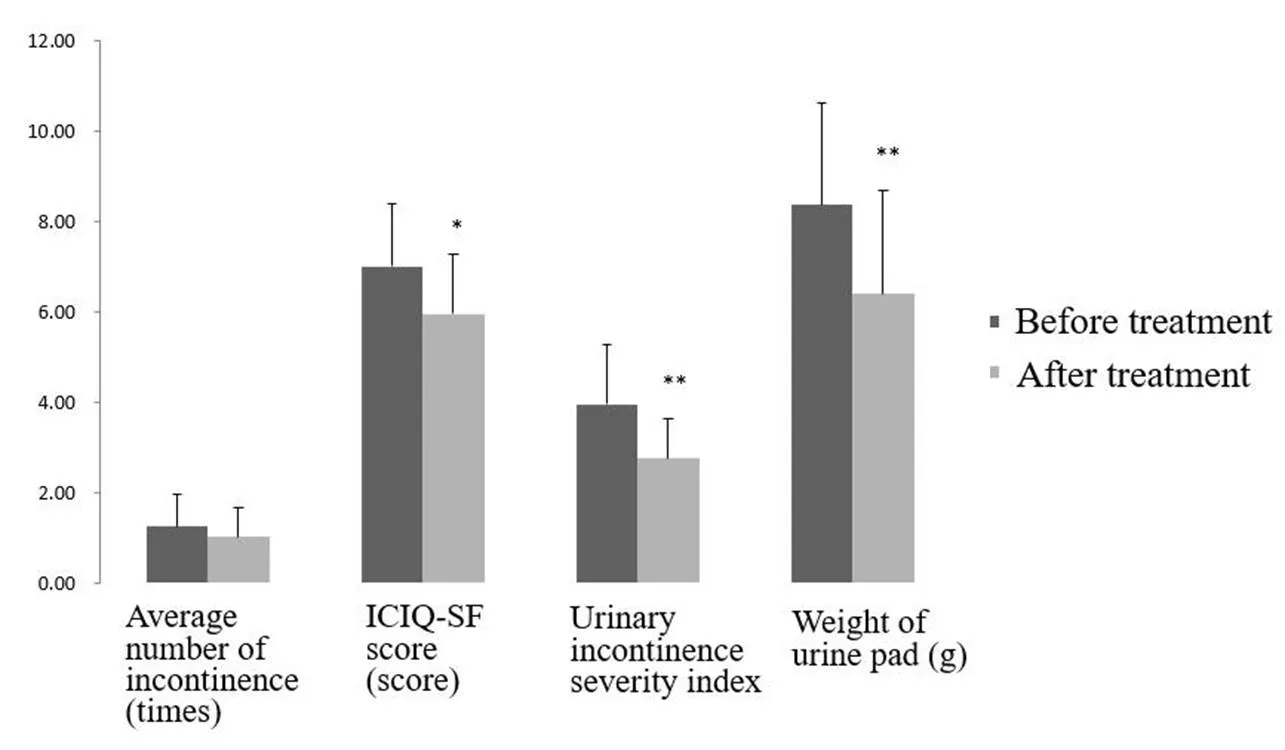
Figure 1 Comparison of indexes of elderly female SUI subjects before and after experiment
Note: ICIQ-SF, International Consultation on Incontinence Questionnaire-Simple Form. Compared with before the experiment,*< 0.05,**< 0.001.
Discussion
The strength of female pelvic floor muscles, urethral resistance and normal anatomical position of organs determine the urinary control function of women. The self-made pelvic floor muscle training exercises mainly improve the stress urinary incontinence problem from the muscle strength of the pelvic floor muscles. At the same time, the abdominal pressure and abdominal muscle training are used to improve the abdominal pressure of the elderly women. Comparing the data before and after the experiment, it was found that the 10-week pelvic floor rehabilitation exercises had no significant improvement on the average 24-hour frequency of urinary leakage. But the reduction of the ICIQ-SF score, urinary incontinence index and the weight of 1h urinary pad proved that the pelvic floor muscle rehabilitation had the function of decreasing the quantity of urinary incontinence instead of the frequency of incontinence.
Both pelvic floor muscle functional exercise and Kegel exercise can increase the muscle strength of pelvic floor muscle through muscle contraction exercise and promote the nervous system regulation over pelvic floor muscle. Abdominal muscle exercise can reduce abdominal fat accumulation, promote intestinal peristalsis, effectively reduce intra-abdominal pressure, maintain constant intra-abdominal pressure and reduce bladder pressure. Global Posture Remodeling based on muscle chain theory can use posture adjustment to avoid muscle retraction and compensatory stretching during stretching, so as to correct imbalance and achieve organ reconstruction [7].
SUI is closely related to pelvic floor muscle function. Some studies have found that, integral posture remodeling exercise can help restore normal breathing movement and diaphragm function, improve abdominal muscle function, correct the position of spine and pelvis, and finally improve pelvic floor muscle function [8]. Many Pilates movements or yoga movements can improve the structure of the spine, dominate the whole-body muscle movements, and enhance the muscle strength of the core muscles, thus improving the function of pelvic floor muscles. Meanwhile, Fozzattidivided 52 females into pelvic floor muscle exercise group and whole posture remodeling exercise group. It was found that after 3 months of experimental intervention, the number of urine leakage and the amount of urine pad were significantly reduced, and the score of pelvic floor function and King health questionnaire were both improved, but the frequency of urine leakage in the whole posture remodeling exercise group was more significantly reduced [7]. Therefore, the abdominal muscle strength training and abdominal breathing exercises in this experiment should be increased in measurement, and combined with other exercises such as core muscle strength training to improve the deficiency that the pelvic floor muscle rehabilitation scheduled in this experiment has no significant difference in the number of urine leaks in the elderly female patients with stress urinary incontinence.
There were some shortcuts in this research. Due to the small sample size, the reliability of the conclusion is poor. Different times of urination may affect the outcome of pelvic floor muscle training. BMI plays a vital role in the recovery of pelvic floor muscles after pregnancy [10]. In the experiment, there is no monitoring of the body weight of the subjects after exercise and no analysis of the effect of BMI on the intervention. The experimental period of this experiment is only 10 weeks. Further experiments and exploration are needed on the effect of pelvic floor muscle rehabilitation on SUI in the longer term and the effective peak period.
Vaginal dumbbells can be used as a test index for SUI to obtain more objective feedback effect, but vaginal dumbbells should pay special attention to disinfection problems, few inadvertent infections will occur, and the cost is expensive, so it is not acceptable. A large number of literatures have found that pelvic floor muscle functional exercise is the most important way to improve pelvic floor muscle function. Other functional training, such as abdominal muscle strength strengthening training, and abdominal breathing training can improve abdominal pressure, which has a benign superposition on the impact of elderly women's stress urinary incontinence. It is hoped that the pelvic floor muscle rehabilitation programmed in this experiment can be well known and practiced by more elderly women and thus improve the SUI problems. If there is an opportunity, more precise instruments such as vaginal dumbbells can be used to test the experimental results in future experiments, and yoga or Pilates movements acceptable to the elderly can be studied to further improve the creation of pelvic floor muscle rehabilitation.
Conclusion
The 10-week self-created pelvic floor muscle rehabilitation training exercise can significantly reduce the severity index of urinary incontinence, improve the good self-feeling of elderly women with stress urinary incontinence, and reduce the impact of SUI on daily life. The pelvic floor muscle rehabilitation training exercise is easy to implement, safe and harmless, and worthy of promotion in elderly women.
1. Song YF. Epidemiology and treatment of female urinary incontinence. Chin J Obstet Gynecol 2004, 8: 63-65.
2. Duan JH, Yang Y, Wu SL,A survey on the incidence of urinary incontinence in Beijing. J Beijing Med Univ 2000, 1: 80-81.
3. Song YF, Li YQ, Xu B,Analysis of the incidence of urinary incontinence in female community in fuzhou city. Chin J Obstet Gynecol 2004, 4: 44-46.
4. Yuan Q. A survey on the knowledge and attitude of community nurses about urinary incontinence. Nursing Res 2006, 25: 2287-2288.
5. Hong GY. Mental health status and nursing intervention of elderly female patients with urinary incontinence. International J Nursing 2006, 3: 215-217.
6. Liu F. Evaluation of the effect of pelvic floor electrical stimulation combined with functional exercise in the treatment of SUI in elderly women. China Med Pharmacy 2015, 14: 177-179.
7. Cammu H, Nylen V, Amy JJ. A 10-year follow-up after Kegel pelvic floor muscle exercises for genuine stress urinary incontinence. BJU International 2001, 85: 35-39.
8. Ying XY. Surgical management of SUI in elderly women. Pract Geriatr 2016, 4: 268-271.
9. Zhang SW. Comparison of efficacy of electroacupuncture and PFMT combined with solina in the treatment of moderate and severe mixed incontinence in women. Nanjing Univer Chin Med 2015, 45: 24-26.
10. Price N, Dawood R, Jackson S. Pelvic floor exercise for urinary incontinence: a systematic literature review. Maturitas 2010, 67: 34-40.
BMI, Body Mass Index; ICIQ-SF, International Consultation on Incontinence Questionnaire-Simple Form; SUI, Stress urinary incontinence; NMES, Neuromuscular electrical stimulation; PFMT, Pelvic floor muscle training.
Yuan W. Evaluation of rehabilitation effect of pelvic floor muscle rehabilitation on elderly female stress urinary incontinence. TMR Non-Drug Therapy 2019, 2(3): 72-77.
Chang Liu
10.12032/TMRND201902014
The authors declare that there is no conflict of interests regarding the publication of this paper.
*Corresponding to:Wei Yuan, No.16 Donghai Road, West Tuanbo New Town, Jinghai District, Tianjin 301617, China. E-mail: 1016885856@qq.com.
- TMR Non-Drug Therapy的其它文章
- Exploring the characteristics of acupoints in the treatment of stroke with complex network and point mutual information method
- Comparison of the effects of moxibustion and lipid-lowering drugs for primary hyperlipidemia: a meta-analysis
- Advances in the application of acupuncture in military first aid
- Acupuncture combined with modern rehabilitation therapy for post-stroke flaccid paralysis
- An effective and easy to insist on self-made pelvic floor muscle rehabilitation for the elderly women with stress urinary incontinence