Comparison of the effects of moxibustion and lipid-lowering drugs for primary hyperlipidemia: a meta-analysis
Si-Yu Liu, Yan-Ru Xia, Yan-Zuo Liu, Sheng-Nan Song, Wei Xu, Bao-Jie Han, *
Comparison of the effects of moxibustion and lipid-lowering drugs for primary hyperlipidemia: a meta-analysis
Si-Yu Liu1, Yan-Ru Xia1, Yan-Zuo Liu2, Sheng-Nan Song1, Wei Xu2, Bao-Jie Han1, *
1First Teaching Hospital of Tianjin University of TCM, Tianjin 300617, China.2Tianjin University of Traditional Chinese medicine, Tianjin 301617, China.
Systematically compared the effects of moxibustion and lipid-lowering drugs on hyperlipemia.Randomized controlled trials (RCTs) published before December 2018 were all aggregated, focusing on evaluation of moxibustion and lipid-lowering drugs for hyperlipemia from PubMed, EMbase, the Cochrane Library, Web of Science, CNKI, CBM, WANFANG database and VIP databases. The quality of the included studies was assessed basing on Cochrane handbook 5.1.0, and the available data were analyzed with RevMan software (version 5.3).Totally 8 RCTs were included with 561 patients. Compared with statins, moxibustion had a better effect to reduce the total cholesterol (TC) (MD = -0.19, 95% CI: -0.24, 0.13,< 0. 001). Moxibustion also had a better effect to reduce low density lipoprotein cholesterol (LDL-C) in compared with statins and fibrates (MD = 0.20, 95% CI: 0.15, -0.25,< 0. 001), but there were no significant differences between statins, fibrates and moxibustion in lowering triglyceride (TG) (MD = -0.02, 95% CI: -0.09, 0.05,= 0.61) and High-density lipoprotein cholesterol (HDL-C) (MD = 0.03, 95% CI: 0.06, 0.13,= 0.51). While, compared with the Chinese patent medicine, there was no significant difference in the efficacy of lowering TC (MD = 0.05, 95% CI: 0.17, 0.27,= 0.67), TG (MD = -0.08, 95% CI: 0.41, 0.24,= 0.61), LDL-C (MD = -0.14, 95% CI: 0.38, 0.11,= 0.28) and HDL-C (MD = 0.11, 95% CI: 0.01, 0.22,= 0.06).Compared with statins and fibrates, moxibustion had advantages in lowering TC and LDL-C, but there was no robust evidence that moxibustion was superior to Chinese patent medicine in improving the blood lipid indexes of patients with hyperlipidemia.
Moxibustion, Hyperlipemia, Meta-analysis, Randomized controlled trial
The goal of the meta-analysis in this paper is to compare the effects of moxibustion and lipid-lowering drugs on the patients with hyperlipidemia. The results showed that the moxibustion had a more significantly effect compared with statins and fibrates on Total cholesterol (TC) and Low-density lipoprotein cholesterol (LDL-C), but the results didn't show statistically significant difference on Triglycerides and High-density lipoprotein cholesterol (HDL-C). In the comparison of adverse reactions, moxibustion had advantages. In terms of the comparison between moxibustion and proprietary Chinese medicine, it was impossible to show therapeutic differences between moxibustion and proprietary Chinese medicine in various indicators.
By systematically comparing the effects of moxibustion and lipid-lowering drugs on hyperlipemia, the authors found that moxibustion had a better effect to reduce the TC and LDL-C compared with statins and fibrates, but no advantages in lowing triglyceride level and HDL-C. While, there was no robust evidence that moxibustion was superior to Chinese patent medicine in improving the blood lipid indexes of patients with hyperlipidemia.
Introduction
Hyperlipidemia is a major risk factor for cardiovascular and cerebrovascular diseases, which can lead to coronary heart disease and ischemic stroke [1]. According to data from 2009 to 2012, over 100 million U.S. adults at the age of 20 years or above have total cholesterol (TC) levels over 200 mg/dL [2]. The increasing level of serum cholesterol will lead to an increase of 9.2 million cardiovascular events in China between 2010 and 2030 [3]. Statins are the first-line drug for hyperlipidemia, but 47% patients with high hyperlipidemia fail to satisfactorily control this condition. The most important reason is the adverse effects of the lipid-lowering drugs, which results in patient noncompliance [4]. Therefore, a substantial proportion of hyperlipidemia patients resort to complementary and alternative medicines.
Moxibustion is a traditional East Asian medical therapy that uses the heat generated by burning herbal preparations containing Artemisia vulgaris to stimulate acupuncture points [5]. Through producing various temperature levels of heat stimulation from mild skin warming to tissue damage from burning, moxibustion can yield inflammatory responses and induce vascular changes. Such inflammatory responses that affect vascular activity might have some potential of anti-oxidative stress and protection of vascular endothelium [6]. Several animal studies have demonstrated effects on hyperlipidemia following moxibustion treatment. For example, crude-herb moxibustion can regulate general and liver fat metabolism, reduce fat deposits in the liver, inhibit fatty degeneration of liver cells, and restore normal liver cell function [7]. In hyperlipidemia rats, the activation of transient receptor potential vanilloid 1-4 is related to the cholesterol-lowering effect of moxibustion [4]. The clinical researches also reported that moxibustion can down-regulate the blood lipid and blood viscosity of patients with coronary heart disease or cerebral infarction. As the systematic study of moxibustion for hyperlipidemia is lack, we conducted a meta-analysis to evaluate the effectiveness of moxibustion as a treatment for hyperlipidemia in human patients.
Materials and methods
Search strategy
Randomized controlled trials (RCTs) published before December 2018 were all aggregated, focusing on evaluation of moxibustion and lipid-lowering drugs for hyperlipemia from PubMed, EMbase, the Cochrane Library, Web of Science, CNKI, CBM, WANFANG database and VIP databases. The literature search formula for PubMed was as follows: hyperlipemia OR hyperlipaemias OR hyperlipidemia OR lipidemia OR lipemia OR dyslipidemia OR dyslipoproteinemias and moxibustion OR moxabustion. For Chinese databases, the following search terms were used: hyperlipidemias OR hyperlipemia OR hyperlipidemia OR lipidemia OR lipemia OR dyslipidemia OR dyslipoproteinemias OR blood lipid and moxibustion. References of retrieved papers are also searched.
Inclusion and exclusion criteria
The inclusion criteria for our study were as following: (1) RCTs in which only moxibustion was administered to patients; all included studies should use lipid-lowering agents (Chinese patent medicine or medicine such as statins and fibrates) or no treatment as a control; (2) Eligible trials had to include adult participants meeting the National Cholesterol Education Programmed diagnostic criteria of hyperlipidemia (measure twice under normal diet within 2 weeks, TC ≥ 5.72 mmol/L or triglyceride ≥ 2.26 mmol/L with or without high-density lipoprotein ≤ 1.04 mmol/L); (3) the outcome measures were representative. Exclusion criteria include: (1) excluded secondary causes such as hypothyroidism, familial hypercholesterolemia, diabetes mellitus, liver or kidney diseases; (2) cases where moxibustion was combined with other therapies were excluded; (3) the experimental results were ambiguous or unreliable.
Quality assessment
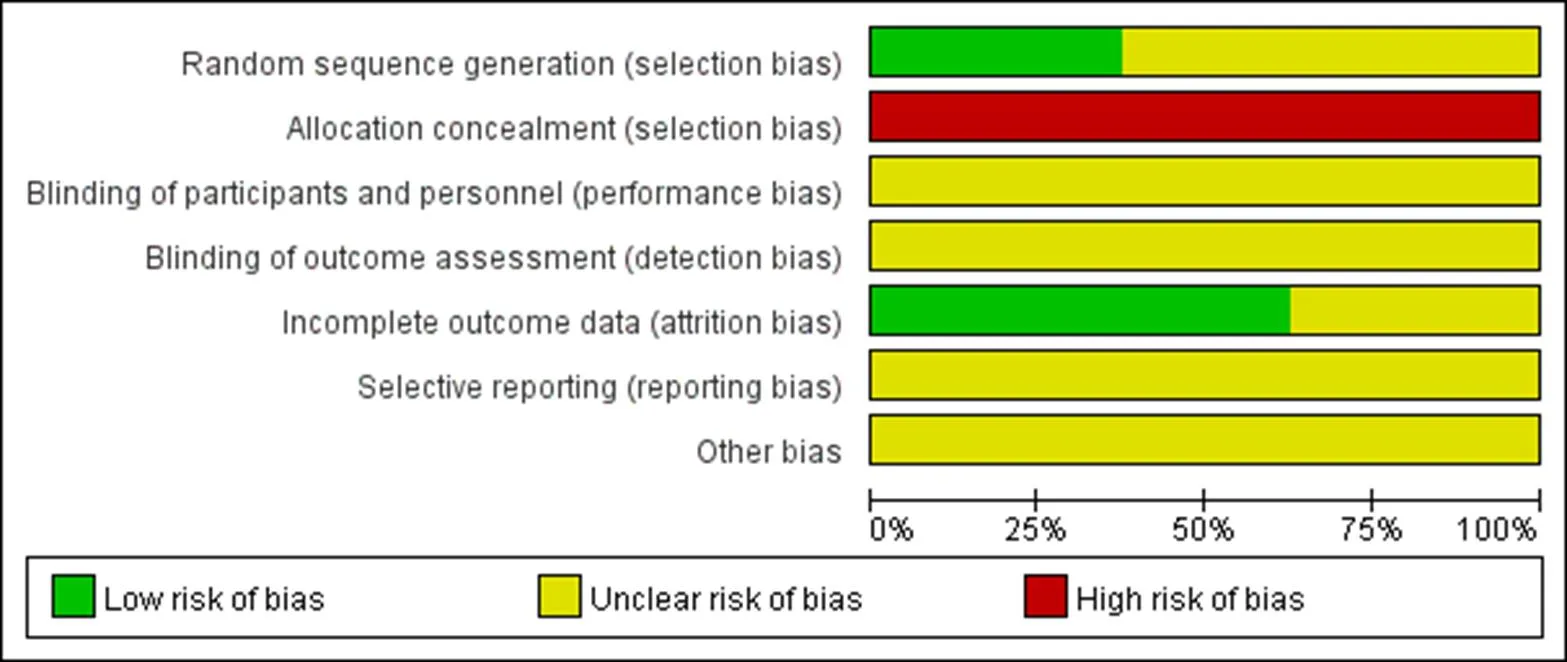
Literature screening was performed independently by two researchers. A third researcher was consulted for disagreements. We evaluated the quality of the studies in terms of the quality criteria in the Cochrane Handbook for systematic review of interventions, version 5.10 [8]. The bias risk assessment tool included seven aspects: (1) random sequence generation; (2) allocation concealment; (3) blinding of participants and personnel; (4) blinding of outcome assessment; (5) incomplete outcome data; (6) selective reporting; (7) other bias.
Data extraction
Two reviewers performed the data extraction independently. Information about first author, year of publication, demographic characteristics of the participants, age and sex of the participants, sample size (treatment group and control group), course of treatment, therapeutic method, outcome indicators were recorded.
Statistical analysis
We used RevMan 5.3 software (ver. 5.3 RevMan, Copenhagen, Denmark) for all the statistical analyses [9]. The odds ratio (OR) of data was calculated for dichotomous variables, and the mean difference (MD) with 95% confidence intervals (CI) is calculated for continuous variables. We apply the fixed effect model for homogeneity (> 0.1, I2> 50%), and the random effect model when heterogeneity was significant (≤ 0.1, I2≤50%) if clinical or methodological heterogeneity did not exist.
Results
Study description
A total of 570 articles were identified, with 420 remained after deleting the duplicate. 378 articles were excluded according to the inclusion criteria after screening the titles and abstracts. Ultimately, 8 studies 10-17 were included for our analysis with 561 patients (Figure 1). All these RCTs were conducted in China and published in Chinese. Table 1 summarized the basic information of these RCTs.
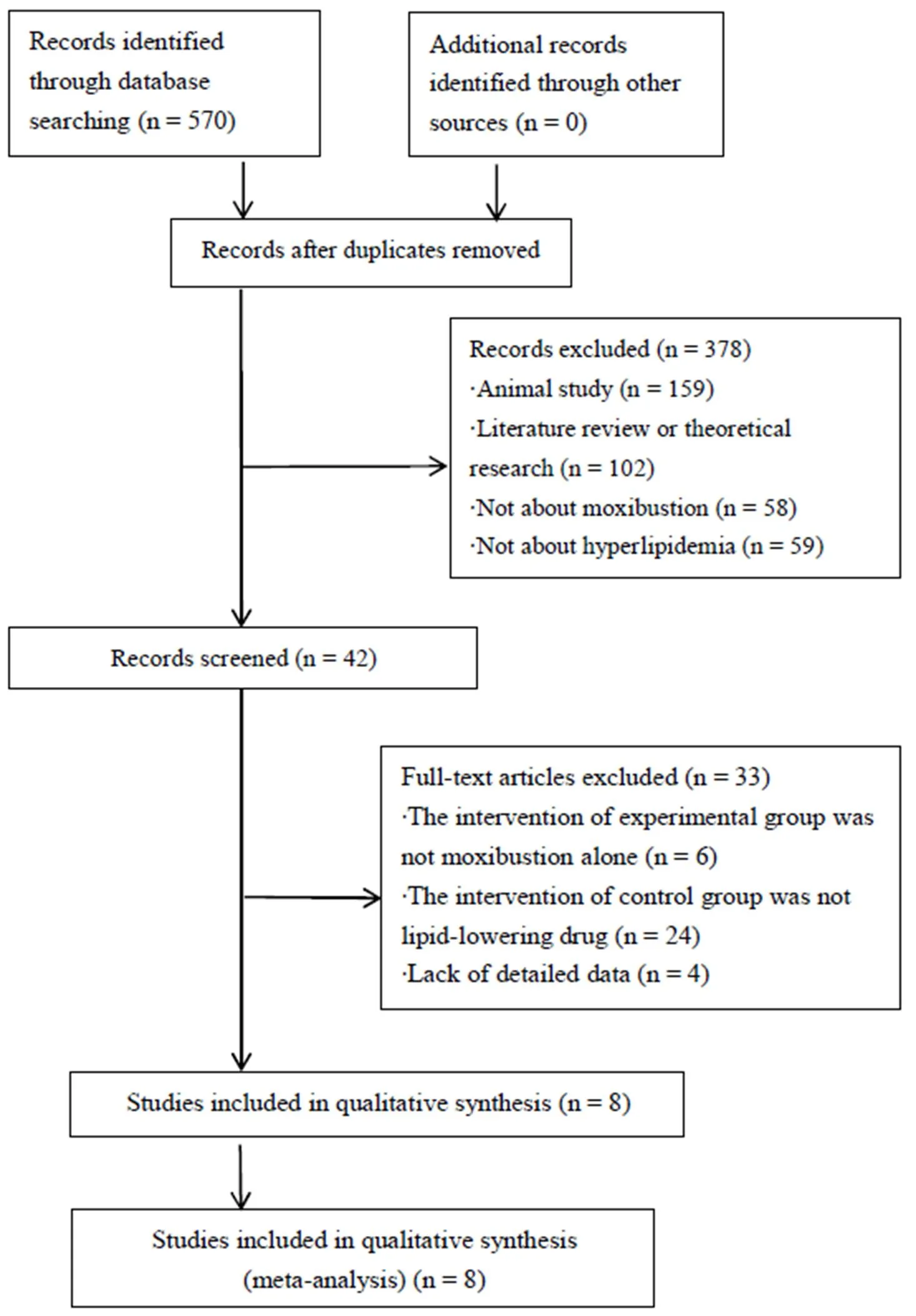
Figure 1 Flow diagram of studies considered for inclusion
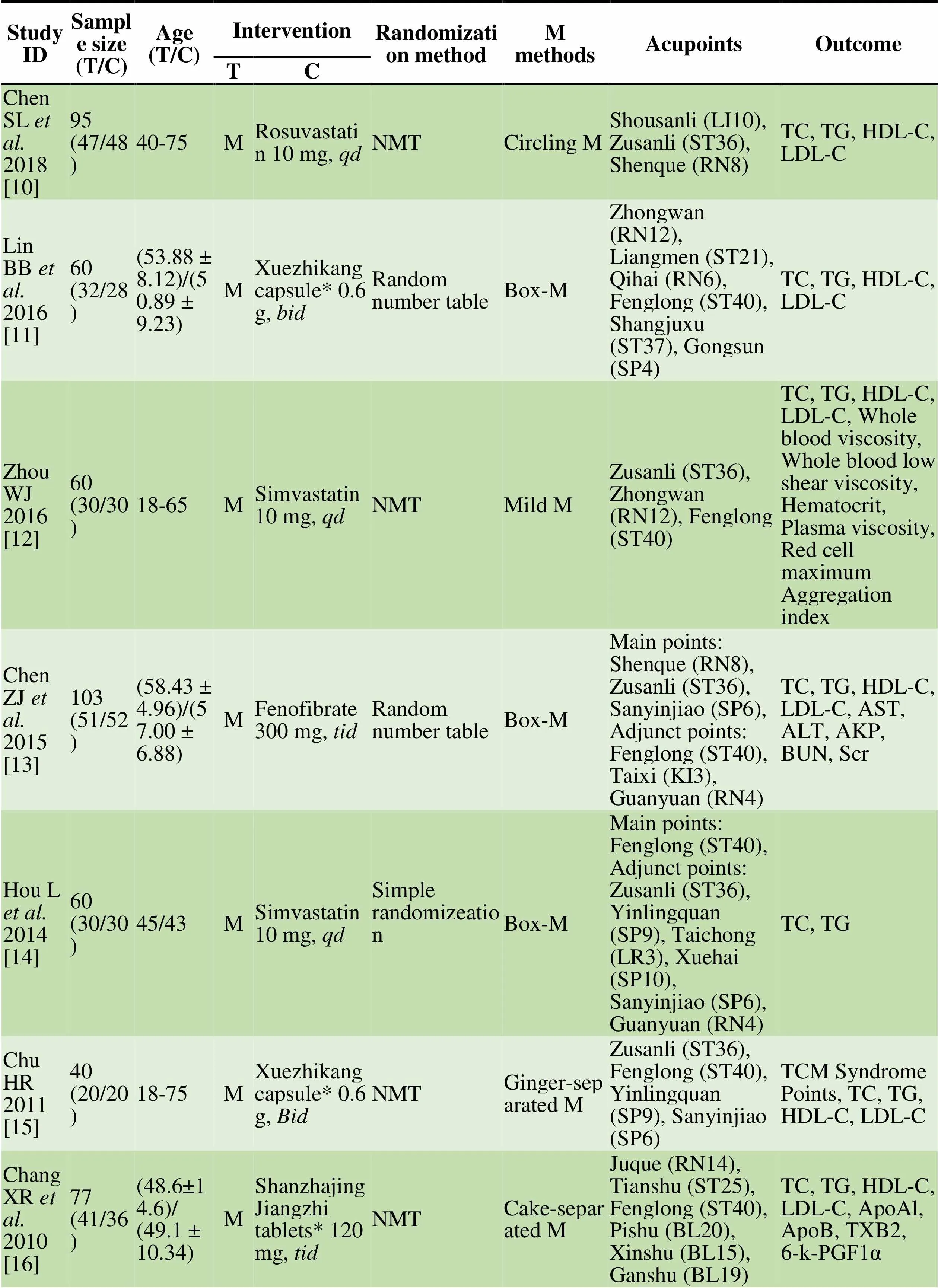
Table 1 Summary of characteristics in studies included
Notes: T/C, Treatment group/control group; M/F, Male/female; TC, Total cholesterol; TG, Triglycerides; LDL-C, Low-density lipoprotein cholesterol; HDL-C, High-density lipoprotein cholesterol; AST, Aspartate aminotransferase; ALT, Alanine aminotransferase; AKP, Alkaline phosphatase; BUN, Blood urea nitrogen; Scr, Serum creatinine; ApoA1: apolipoprotein A-1; ApoB, Apolipoprotein B; TXB2, Thromboxane B2; 6-k-PGF1α, 6 - ketone - prostaglandin F1α; NMT, Not mentioned; M, Moxibustion; *, Chinese patent medicine.
Quality assessment
A quality assessment of the eight RCTs is summarized in Figure 2 and 3. All studies emphasized the use of randomization, but only three of them [11, 13, 14] described detailed randomization methods. None of them reported either the allocation concealment or blinding methods. Three studies [10, 12, 13] reported missed cases but none of them use the intention-to-treat analysis (ITT). Selective reporting was unclear due to the unattainability of the research programs. Other biases could not be determined in the absence of sufficient evidence.
Effects on outcome indicators
TC All the 8 RCTs [10-17] compared the effects of lowering TC between the treatment and control groups with 555 patients. Three were comparative studies of moxibustion and Chinese patent medicine, and four were comparative studies of moxibustion and statins. In the subgroup where moxibustion was used as experimental group, Chinese patent medicine was used as control, meta-analysis did not show a significant difference in lowering TC between the treatment and control groups (MD = 0.05, 95% CI: -0.17, 0.27,= 0.67), while moxibustion had a more obvious effect on reducing TC compared with statins (MD = -0.19, 95% CI: -0.24, -0.13,< 0. 001). One study was a comparative study of moxibustion and Fenofibrate, and there was no statistical significance in the reduction of total cholesterol (MD = 0.11, 95% CI: -0.36, 0.58,= 0.64, Figure 4).
Triglycerides (TG) All the 8 RCTs [10-17] reported the comparison of TG between the treatment and control groups. The subgroup where statins and fibrates were used as the control (I2= 52%,= 0.08) fails the heterogeneity test. After removing RCT by Hou, the heterogeneity was acceptable (I2= 0%,= 0.47). The results showed that the difference in efficacy was not significant (MD = -0.02, 95% CI: -0.09, 0.05,= 0.61). It also shows there was no statistically significant difference between moxibustion and Chinese patent medicine (MD = -0.08, 95% CI: -0.41, 0.24,= 0.61, Figure 5).
LDL-C We included seven RCTs [10-13, 15-17] which compared moxibustion with drug on LDL-C with 495 patients involved in total. Four were comparative studies of statins, fibrates and moxibustion, three were comparative studies of moxibustion and Chinese patent medicine. Our results show that moxibustion was more effective than statins and fibrates (MD = 0.20, 95% CI: 0.15, 0.25,< 0.00001). The results did not show statistically significant difference between moxibustion and Chinese patent medicine, either (MD = -0.14, 95% CI: -0.38, 0.11,= 0.28, Figure 6).
HDL-C We included seven RCTs [10-13, 15-17] which compared moxibustion with drug on HDL-C with 495 patients in these studies. The meta-analysis showed significant heterogeneity in the subgroup where statins and fibrates were used as the control (I2= 85%,= 0.0002). The trials passed the heterogeneity test after we removed RCT by Wei (I2= 0%,= 0.83), which may be relevant to publication bias. The results did not show statistically significant difference between moxibustion and lipid-lowering drugs, either (Chinese patent medicine group MD = 0.11, 95% CI: -0.01, 0.22,= 0.06; statins and fibrates group MD = 0.03, 95% CI: -0.06, 0.13,= 0.51, Figure 7).
Discussion
Lowering blood lipid levels is one of the bases for the treatment and prevention of major clinical cardiovascular and cerebrovascular diseases. Statins as highly effective drugs, are associated with increased risk of myopathy, transaminase and diabetes for some patients. The application of proprietary Chinese medicines is a new clinical practice for avoiding adverse reactions of statins, but it cannot replace statins at present. Moxibustion is a kind of external treatment of traditional Chinese medicine, which has less adverse reactions. However, as approaches of complementary and alternative medicine (CAM), their acceptance by the mainstream medical community is often limited due to the lack of robust evidence and the differences in the philosophy adopted [27].
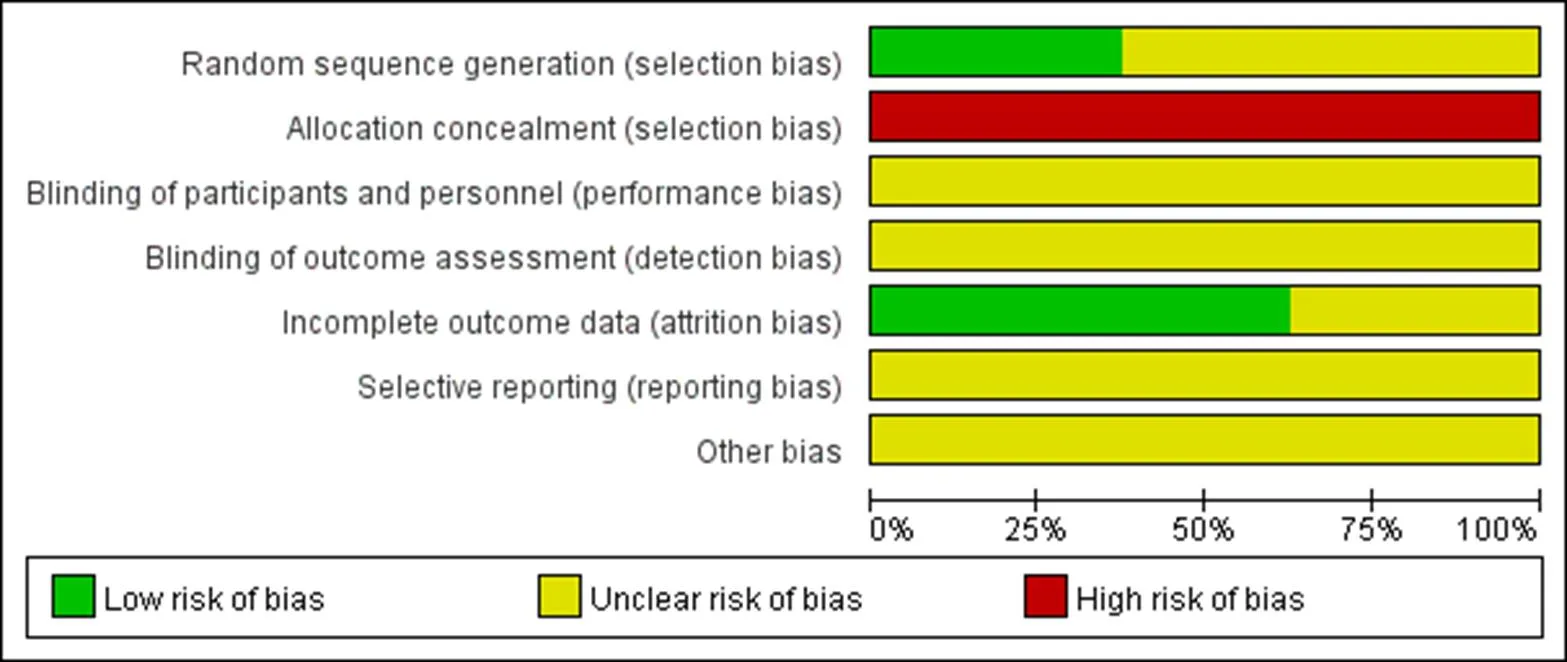
Figure 2 Assessment of risk of bias
Figure 3 Each risk of bias domain for each included study
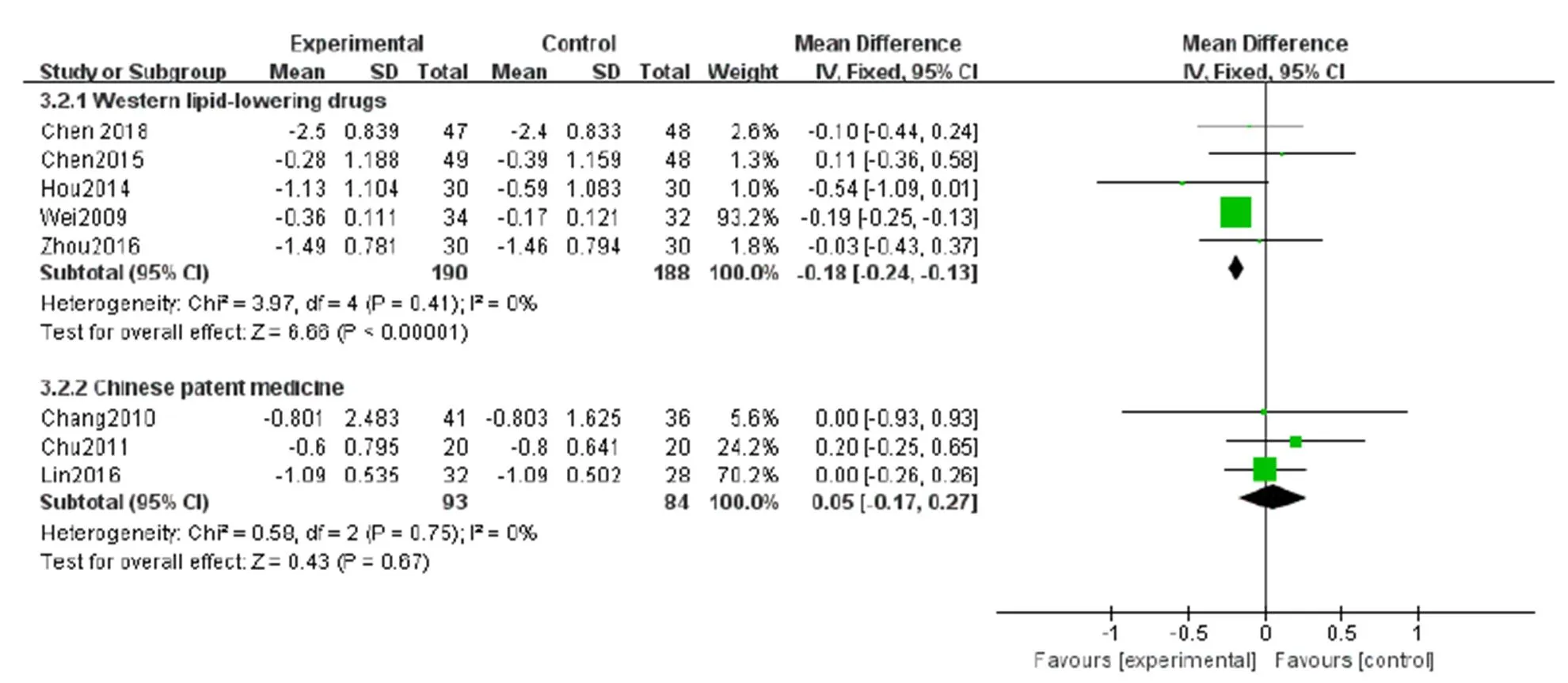
Figure 4 Meta-analysis on TC
Figure 5 Meta-analysis on TG
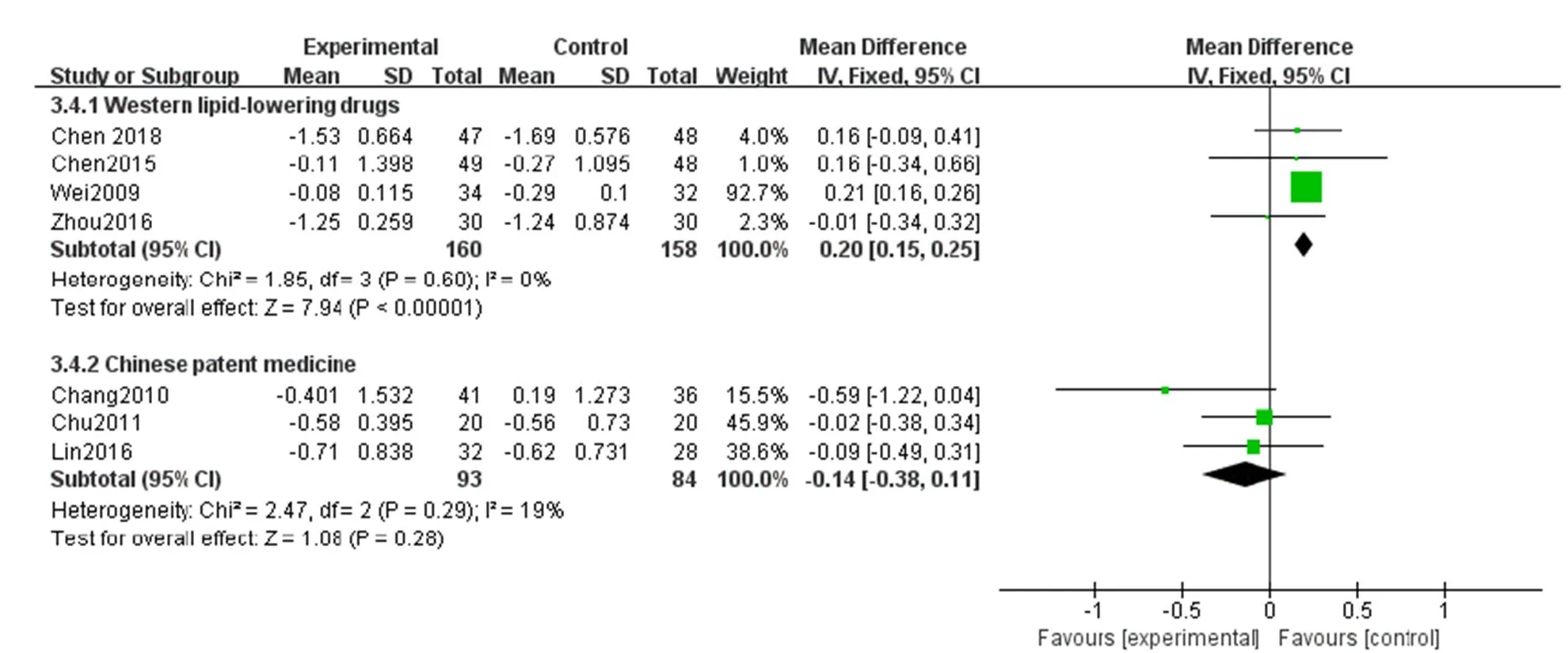
Figure 6 Meta-analysis on LDL-C
Figure 7 Meta-analysis on HDL-C
The goal of the meta-analysis in this paper was to compare the effects of moxibustion and lipid-lowering drugs on the patients with hyperlipidemia. The results of the eight studies showed that the moxibustion had a more significant effect compared with statins and fibrates on TC and LDL-C, but the results did not show statistically significant difference on TG and HDL-C. In the comparison of adverse reactions, moxibustion had advantages. In terms of the comparison between moxibustion and proprietary Chinese medicine, it is impossible to show therapeutic differences between moxibustion and proprietary Chinese medicine in various indicators.
The limitations and suggestions are as follows: (1) Only eight studies were included in the analysis. The included RCTs showed a medium-to-high bia. More high-quality, large-sample studies are needed to obtain more robust results. (2) Only three of the included studies described randomized methods in detail. Therefore, researchers should report all these methods in detail for the reliability of the results. (3) The risk mainly comes from the allocation of hidden and blind methods, which may lead to unclear research results. Blinding is difficult to achieve due to the operation characteristics of moxibustion. However, the research is supposed to use the method of allocation concealment to ensure the randomness of the study and report the process in detail in the study. (4) Because of the lack of long-term follow-up, long-term efficacy cannot be determined, which should be amended. (5) Different moxibustion methods in the experimental group and different lipid-lowering drugs in the control group may interfere with the analysis results. For different lipid-lowering drugs, we divided them into different subgroups for separate analysis according to drug categories. In view of the consistent principle of different moxibustion methods, they were not grouped for analysis, but it may lead to errors in the analysis results.
Conclusion
Compared with statins and fibrates, moxibustion has advantages in lowering TC and LDL-C, but there is no robust evidence that moxibustion is superior to Chinese patent medicine in improving the blood lipid indexes of patients with hyperlipidemia. Meanwhile, it has the advantage of less adverse reactions. However, the small sample size and low quality of the RCTs reduce the credibility of this meta-analysis. Therefore, RCTs with more rigorous designs, larger samples, and long-term follow-up are required to further identify the long-term efficacy of moxibustion on hyperlipidemia.
1. Nelson RH. Hyperlipidemia as a risk factor for cardiovascular disease. Primary Care 2013, 40: 195-211.
2. Jellinger PS, Handelsman Y, Rosenblit PD,American association of clinical endocrinologists and American college of endocrinology guidelines for management of dyslipidemia and prevention of cardiovascular disease. Endocrine Practice 2017, 23: 1-87.
3. Moran A, Gu D, Zhao D,Future cardiovascular disease in china: markov model and risk factor scenario projections from the coronary heart disease policy model-china. Circ Cardiovasc Qual Outcomes 2010, 3: 243-252.
4. Malloy MJ, Kane JP. Hyperlipidemia and Cardiovascular Disease. Curr Opin Lipidol 2012, 23: 591-592.
5. Tietge UJ. Hyperlipidemia and cardiovascular disease: inflammation, dyslipidemia, and atherosclerosis. Curr Opin Lipidol 2014, 25: 94-95.
6. Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults. Executive summary of the third report of the national cholesterol education program expert panel on detection, evaluation, and treatment of high blood cholesterol in adults. JAMA 2001, 285: 2486-2497.
7. Liu AM, Wu QH, Guo GC,. Statins: adverse reactions, oxidative stress and metabolic interactions. Pharmacol Ther 2019, 195: 54-84.
8. Chen S, Guo SN, Wang J,Effectiveness of moxibustion for allergic rhinitis: protocol for a systematic review. BMJ Open 2015, 5: e006570.
9. Duan L, Zhao GZ, Ji B,Effect of crude-herb moxibustion on blood lipids in rats with dyslipidemia. J Tradit Chin Med Sci 2014, 1: 140-147.
10. Sun X, Li XW. Experimental study of the treatment of fatty liver by Tianjiu Therapy in rats. J Beijing Univ TCM 2001, 12: 48-50, 68.
11. Wang YS, Wang SC, Zhang JB,Effects of different moxibustion treatments on the expression of local Cx43 in hyperlipernia rats and correlationship with blood lipid -regulation. Li Shizhen Med Materia Medica Res 2012, 23: 1548-1549.
12. Su FF, Gao JY, Wang GY,Effects of moxibustion at 45 ℃ on blood lipoids and serum level of ox-LDL and NO in rats with hyperlipidemia. Chin Acupunc Moxibustion 2019, 39: 180-184.
13. Wang GY, Wang LL, Xu B,. Effects of moxibustion temperature on blood cholesterol level in a mice model of acute hyperlipidemia: role of TRPV1. Evid Based Complement Alternat Med 2013, 11: 1-7.
14. Jiang JF, Wang XJ, Wu XJ,Analysis of factors influencing moxibustion efficacy by affecting heat-activated transient receptor potential vanilloid channels. J Tradit Chin Med 2016, 36: 255-260.
15. Wang Y, Zhong MR, Wsng Q,Effect of thunder-fire moxibustion on blood lipid and hemorheology in patients with coronary heart disease undergone interventional treatment. Shanghai J Acupunc Moxibustion 2015, 34: 1056-1058.
16. Cui YJ, Cui PX, Geng LQ,Effect of moxibustion on blood lipid level in patients with cerebral infarction complicated with hyperlipidemia. J Sichuan Tradit Chin Med 2016, 34: 169-171.
17. Higgins JPT, Altman DG, Sterne JAC. Assessing risk of bias in included studies. Cochrane handbook for systematic reviews of interventions version 5.1.0. Cochrane Collaboration, 2011.
18. The nordic cochrane centre TCC. RevMan, computer program. Version 5.3 DB/CD. Copenhagen, Denmark: 2014.
19. Chen SL, Zhang L. Effect of moxibustion on blood lipid in patients with coronary heart disease. Heilongjiang Medicine Pharmacy 2018, 41: 69-70.
20. Lin BB, Chen YY. Treatment of 32 cases of hyperlipidemia with compound medicine moxibustion. Fujian J Tradit Chin Med 2016, 47: 21-22.
21. Zhou WJ. Effect of platelet derived growth factor BB on hyperlipidemia by healthful moxibustion. Anhui University Tradit Chin Med, 2016.
22. Chen ZJ, Wu ZC, Wang JJ,Clinical observation on 49 cases of hyperlipidemia treated by moxibustion based on syndrome differentiation. J Tradit Chin Med 2015, 56: 1935-1938.
23. Hou L, Niu YB. Clinical study on the treatment of hyperlipidemia by dialectical acupoint selection. China Foreign Med Treatment 2014, 33: 4-5.
24. Chu HR. Observation on the therapeutic effect of ginger-separated moxibustion on hyperlipidemia, China association of acupuncture-moxibustion 2011, 44: 9.
25. Chang XR, Yan J, Yi SX,Clinical research on cake-seperated moxibustion treating patients with hyperlipemia. Chin Archives Tradit Chin Med 2010, 28: 8-10.
26. Wei HQ, Ding CH, Zhang Q,Clinical observations on moxibustion treatment for hypedipemia. Shanghai J Acupunc Moxibustion 2009, 28: 698-699.
27. Liu M, Zhang Q, Jiang S,Warm-needling acupuncture and medicinal cake-separated moxibustion for hyperlipidemia: study protocol for a randomized controlled trial. Trials 2017, 18: 310.
RCTs, Randomized controlled trials; TC, Total cholesterol; TG, Triglycerides; LDL-C, Low-density lipoprotein cholesterol; HDL-C, High-density lipoprotein cholesterol; AST, Aspartate aminotransferase; ALT, Alanine aminotransferase; AKP, Alkaline phosphatase; BUN, Blood urea nitrogen; Scr, Serum creatinine; ApoA1: Apolipoprotein A-1; ApoB, Apolipoprotein B; TXB2, Thromboxane B2; 6-k-PGF1α, 6 - ketone - prostaglandin F1α.
Liu SY, Xia YR, Liu YZ,Comparison of the effects of moxibustion and lipid-lowering drugs for primary hyperlipidemia: a meta-analysis. TMR Non-Drug Therapy 2019, 2(3): 85-94.
Chang Liu
10.12032/TMRND201902015
The authors declare that there is no conflict of interests regarding the publication of this paper.
*Corresponding to: Bao-Jie Han, Department of Acupuncture & Moxibustion, First Teaching Hospital of Tianjin University of TCM, Tianjin 301617, China. E-mail: hbj0909@163.com
- TMR Non-Drug Therapy的其它文章
- Exploring the characteristics of acupoints in the treatment of stroke with complex network and point mutual information method
- Advances in the application of acupuncture in military first aid
- Evaluation of therapeutic effects of self-made pelvic floor muscle rehabilitation on elderly female stress urinary incontinence
- Acupuncture combined with modern rehabilitation therapy for post-stroke flaccid paralysis
- An effective and easy to insist on self-made pelvic floor muscle rehabilitation for the elderly women with stress urinary incontinence