Prehospital response to respiratory distress by the public ambulance system in a Ukrainian city
Colin A. Meghoo, Stanislav Gaievskyi, Oleksandr Linchevskyy, Bindhu Oommen, Kateryna Stetsenko
1 Research Department, Patriot Defence, Kyiv, Ukraine
2 School of Public Health, Kyiv-Mohyla Academy, Kyiv, Ukraine
3 Clinical Hospital #17, Kyiv, Ukraine
4 Hunt Regional Medical Center, Greenville, Texas, USA
5 Center of Emergency Medical Care and Disaster Medicine, Kyiv, Ukraine
KEY WORDS: Emergency Medical Services; Dyspnea; Ukraine
INTRODUCTION
The public emergency medical services (EMS)system of Ukraine is currently receiving increased scrutiny, with an effort by the Ministry of Health to transform an expensive system that provides unknown quality of prehospital care to its population.
While a comprehensive evaluation of the effectiveness of this EMS system would address the multiple dimensions of structure, process, and outcome measurements,[1,2]good conclusions can be made from evaluating single “tracer” patient conditions.[3]
Based on the five patient conditions identified by the European Resuscitation Council that clearly benefit from immediate prehospital care,[4]we selected respiratory distress for further evaluation. Respiratory distress is a common and potentially life-threatening condition accounting for approximately one in eight EMS calls,and the manner in which this condition is addressed has been used as a basis for international comparisons across multiple EMS systems.[4,5]Additionally, a prompt response from ambulances possessing advanced life support (ALS) capabilities, has been demonstrated to confer a survival advantage.[6]
In Ukraine, most citizens use the public ambulance system as their initial entry point to the medical system for receiving urgent care. Individuals are able to dial 103 from any phone to access Emergency Medical Services (EMS) without charge. Public ambulances dispatched to these urgent calls have a mandated tenminute response time, with many ambulances having emergency physicians on board, providing physicianstaffed emergency medical services (P-EMS). Little is known about the capability of the public ambulance system in urban areas of Ukraine to respond to critical or potentially life-threatening medical conditions.
In multiple medium and large cities in Ukraine, the dispatch process has only recently been computerized.These digital accounts of all received calls provide a reliable and comprehensive source of information regarding initial call classification, response times,treatment times, field diagnoses, and patient disposition.Previously, this information was unavailable for research purposes.
METHODS
With support from the Ukrainian Ministry of Health,we were granted access to anonymized computer records from the central EMS dispatch center in Poltava, a city of 300,000 in central Ukraine. We imported data on response times, patient demographics, prehospital diagnoses, and patient outcome and disposition for the period from 01 January 2018 to 31 May 2018 into a Microsoft Excel spreadsheet Version 14.6.7 (Microsoft Corporation, Redmond, Washington, USA). Urgent calls with a coded dispatcher diagnosis of difficulty breathing were extracted. Most of the transport times were recorded automatically, although the times of arrival to the patient were entered by the ambulance team. Prehospital diagnoses were documented by the emergency physician on scene using International Classification of Diseases,10th edition (ICD-10) codes. The patient’s clinical status and disposition were entered by the treating ambulance team. We calculated ambulance response times, and field times. We extracted data on all prehospital deaths following a call of respiratory distress and calculated odds ratios to assess correlation between specific patient and call characteristics and an adverse outcome.
RESULTS
During the first five months of 2018, the EMS dispatch center at Poltava received 30,978 urgent calls. A total of 2,029 (6.5%) were coded by medical dispatchers as representing respiratory distress. Four patients were reported to be apneic at the time of the call. Five were unconscious. Thirty patients had some other altered level of consciousness.
The 2,029 patients were 41% male and 59% female.The median age was 64. The majority of the calls(97.4%) were to private residences, and most calls were within the city limits.
A medically-trained central dispatcher initiated a request for an ambulance within a median time of two minutes and 38 seconds. An Advanced Life Support(ALS) ambulance accepted the assignment electronically within a median of six seconds. The response time from dispatch of the ambulance to arrival to the patient was a median of 10 minutes and 12 seconds. All of the ALS ambulances responding to these urgent calls had an emergency physician on board. Assessment and treatment in the field was performed over a median of 33 minutes and 41 seconds.
Seventy-seven percent of patients (1,561 patients)were treated on scene and released. Twenty percent of patients (407 patients) were transported to the hospital,with 6.6% (27 patients) arriving in critical condition.Sixty-one patients (3% of total) died before arrival to the hospital.
The P-EMS team provided a coded prehospital diagnosis using the ICD-10 classification. In 1,640 patients (81.2% of total), an acute respiratory, cardiac,or neurologic condition was suspected. The remaining 19.2% of cases had unknown or miscellaneous diagnoses.Prehospital diagnoses are shown in Table 1.
Odds ratios were calculated to assess the impact ofseveral individual variables to a fatal outcome (Table 2).Age over 60 and a report of altered mental status at the time of the ambulance call were both associated with a significant increase in the likelihood of prehospital death (OR8.75 [95%CI3.16-24.21] and 34.18 [95%CI15.39-75]), respectively.
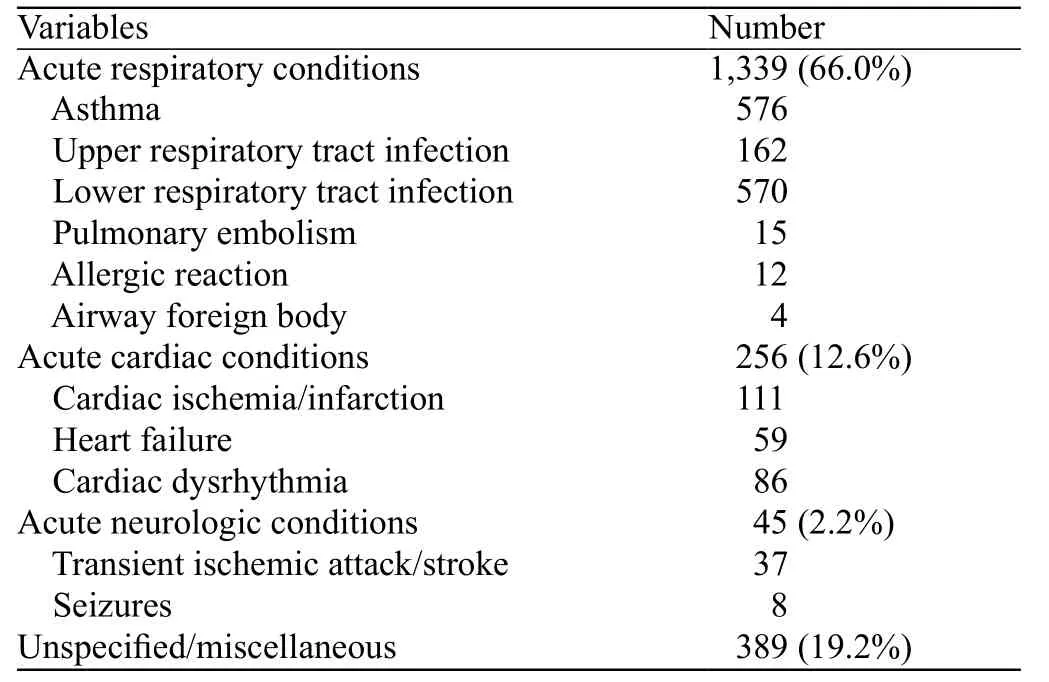
Table 1. Prehospital diagnoses in 2,029 patients with a complaint of respiratory distress in Poltava, Ukraine
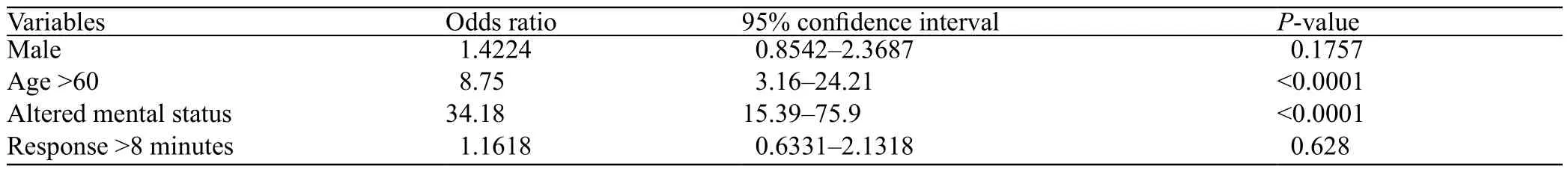
Table 2. Odds ratio of variables as predictors of death for patients with complaints of respiratory distress
DISCUSSION
Response times
Ambulance response times have long been used as a surrogate measure of quality of prehospital care.[7]In many circumstances, including ST-segment elevation myocardial infarction[8]and out-of-hospital cardiac arrest,[9]lessening the time of arrival of ALS-trained personnel is beneficial.
Mandated response times among 14 European countries for the highest urgency calls range from 8 minutes (Spain and United Kingdom) to 20 minutes(Czech Republic).[10]By Regulation #1119 promulgated in 2012 by the Cabinet of Ministers of Ukraine, all calls to the public EMS system have a mandated response time of 10 minutes or less in urban areas, and 20 minutes or less in rural areas. The global evidence for response time as a worthy metric of effective prehospital care is not compelling, though speedy arrival of ambulance, coupled with effective diagnosis and treatment may contribute to improved outcomes in select medical conditions.
Diagnoses
Provisional diagnoses made by the P-EMS team in the field showed a predominance of cardiac and pulmonary etiologies. Generally good concordance between prehospital and hospital-based diagnoses in the setting of respiratory distress has been reported.[11]Unusual in this data was the rarity of chronic obstructive disease exacerbation (ICD-10 code J44.1) compared with other studies,[5,12]suggesting that these patients may have been given other diagnoses.
Treatments
While specific prehospital treatments for these callers with respiratory distress is unknown, clinical resolution is suggested, as only 20% of patients required transportation to the hospital. In the report by Fischer,greater training and experience of ALS unit personnel was associated with improved patient status as measured by normalized respiratory rate and improvements in pulse oximetry readings.[4]These P-EMS units employed more intensive drug therapy and higher rates of prehospital intubation. Christenszen et al[13]showed short-term mortality benefit for patients with acute respiratory disorders when the responding ambulances were staffed with anesthesiologists.N
on-conveyance
Seventy-seven percent of patients in this study were treated on scene and not transported to hospital. By comparison, in the multi-city Canadian study by Stiell,less than 2% of patients that contacted EMS services for a complaint of respiratory distress were released without being taken to hospital.[6]A systematic review of 67 studies reporting non-conveyance rates for a variety of initiating medical complaints identified a wide variation of non-conveyance across multiple countries of 3.7%-93.7%.[14]Multiple potential factors can account for this variation in hospital transport rate, including low medical acuity, high patient refusal rates, high professional competency, treatment protocols that allow for home treatment, low litigation, and viable referral options to other non-acute health care facilities.
The high non-conveyance rate in Ukraine in instances of initial complaints of respiratory distress likely reflects the general approach of Ukrainian ambulance care that adheres to a “treat and release”practice, common in post-Soviet states. In that system,medical respondents to urgent ambulance calls include some combination of feldsher, which is a midlevel provider in primary care/emergency care, and emergency physician. This ambulance crew has a high expectation of being able to manage most conditions at the caller’s house, with basic diagnostic skills and medications. In this system, only the severely sick patient or those who do not respond to initial treatment would be transported to the hospital. This can be more akin to the concept of community paramedicine in which treatment at home for acute exacerbations of chronic conditions can be managed from a mobile platform.
Out of hospital deaths
The prehospital mortality rate in this study was three percent. This statistic included all four of the apneic patients, and four out of five of the unconscious patients.Nine out of the 10 patients with known or suspected out-of-hospital cardiac arrest (OHCA) also died, with some overlap with the prior two groups. It is unrecorded whether patients died prior to ambulance arrival, during treatment in the field, or during transport to the hospital.The multi-city Canadian study by Stiel et al[6]reported a prehospital mortality rate of 1.2%, but excluded patients with OHCA on the arrival of EMS.
The pre-arrival performance of bystander cardiopulmonary resuscitation (CPR) or defibrillation is unknown. A study from Lebanon reported on 271 patients over a 5-year period with OHCA.[15]In that study, bystander CPR rates were 4.4%, survival to hospital admission was 15.9%, and survival to discharge from the hospital was 4.8% .
EMS response times within 11 minutes of bystander CPR administration or within 13 minutes of bystander defibrillation has been correlated with improvements in neurologically intact survival.[9]In our study, a response time of greater than 8 minutes was not associated with an increased risk of death following a complaint of respiratory distress.
ACKNOWLEDGEMENTS
We acknowledge the invaluable support of the World Health Organization, the Ministry of Health of Ukraine,and the non-governmental organization, Patriot Defence,in the completion of this study.
Funding:The study was supported by a consultancy contract from the World Health Organization.
Ethical approval:Not required for this study.
Conflicts of interest:One of our co-authors, OL, is a practicing trauma surgeon, but also serves as the current Deputy Minister of Health for Ukraine.
Contributors:CM proposed the study and wrote the first draft.All authors read and approved the final version of the paper.
 World journal of emergency medicine2019年1期
World journal of emergency medicine2019年1期
- World journal of emergency medicine的其它文章
- Information for Readers
- World Journal of Emergency Medicine
- Venous thromboembolism in the emergency department: A survey of current best practice awareness in physicians and nurses in China
- The use of outcome feedback by emergency medicine physicians: Results of a physician survey
- Rapid sequence induction (RSI) in trauma patients:Insights from healthcare providers
- Comparison between intravenous morphine versus fentanyl in acute pain relief in drug abusers with acute limb traumatic injury
