Effectiveness of complex decongestive therapy in management of breast cancer associated lymphedema
Ting-Ting Li,Zhen-Dong Zheng,Yue-Hai Ma,Qiu-Hua Li,Zhao-Zhe Liu*Department of Oncology,Cancer Center of People’s Liberation Army,General Hospital of Northern Theater Command,Shenyang City, Liaoning Province, P.R.China. Department of Oncology, The Second hospital of Liaoning University of Chinese Medicine,Shenyang City,Liaoning Province,P.R.China.
*Correspondence to: Dr. Zhao-Zhe Liu, Department of Oncology, General Hospital of Northern Theater Command, No. 83 Wenhua Road,Shenhe District,Shenyang City,Liaoning Province 110016,P.R.China.E-mail:lzz_summer@126.com.
Abstract
Keywords:Complex decongestive therapy,Lymphedema,Breast cancer,Effective time
Highlights
The study assesses the edema relief effects of complex decongestive therapy in patients with breast cancer associated lymphedema after axillary lymph node dissection. The results found that there were differences in progress of circumference difference among the patients with different degrees of lymphedema and the effects of patients with severe initial edema(>5 cm increased)last longer.
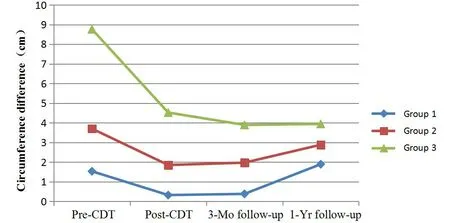
Figure 1 Distribution of circumference difference at study time points. Group 1, mild lymphedema;group 2,moderate lymphedema;group 3,severe lymphedema.
Background
Breast cancer-related lymphedema (BCRL) is one of the most common complications of axillary lymph node dissection (ALND) and subsequent radiotherapy.The incidence of BCRL is about 24% [1]. BCRL is a chronic disease characterized by hydrops in subcutaneous tissues. Over time, the severity of hydrops can develop from mild swelling to severe edema with adipose tissue fibrosis leading to hardening of the extremity [2, 3]. Survival with BCRL may experience substantial pain, feeling heavy and uncomfortable, limited shoulder movement, muscular weakness, and an increased risk of infection [1, 4, 5].These all lead to dysfunction, limited activity and participation, followed by psychosocial distress and poor quality of life[1,6,7].
Lymphedema treatment includes elevation,compression garments, pneumatic pumping, massage,diuretics and micro-surgical reconstruction. Complex decongestive therapy (CDT) is the most commonly used and recognized best method for the treatment of lymphedema[8,9],including manual lymph drainages,sequential gradient pump, low-stretch bandaging,exercises and skin care [10]. Many studies have described the effects of CDT on lymphedema patients,and these studies have reported a reduction in edema after CDT without showing how long the beneficial effect lasted. The long-term effect of CDT on upper extremity lymphedema is little-known. Also, several studies have suggested that the main determinant of treatment success is the initial degree of lymphedema,no matter the treatment time [11, 12]. However, these studies did not show the duration of the benefit based on the initial degree of lymphedema. Therefore, we conducted this retrospective assessment to investigate the long-term effect of CDT on lymphedema extremity circumference reduction, especially considering the grade of lymphedema. Patients were divided into three groups based on the initial degree of lymphedema, and the differences in the degree of lymphedema between the three groups were investigated.
Materials and methods
Patients
A retrospective review was performed for patients who received complex decongestive therapy for upper limb lymphedema following mastectomy of General Hospital of Northern Theater Command from May 2017 to May 2018. The inclusion criteria of this study were as follows, (1) unilateral upper extremity lymphedema after ALND for breast cancer; (2) fully participated in CDT 5 times per week for at least 4 weeks; (3) clinical follow-up over 1 year after CDT.The exclusion criteria were as follows, (1) tumor recurrence during follow-up;(2)other vascular disease of extremity; (3) heart or kidney disease. In our study,patients with sentinel lymph node biopsy were excluded, because of patients undergoing sentinel lymph node biopsy had less common severe lymphedema, which reduced the duration of CDT and leads to inadequate follow-up.Finally,58 patients were enrolled in this study.
The following clinical features were obtained by chart review: patient’s sex, age, lymphedema site,surgery type, whether received radiation or chemotherapy, the time between operation and the onset of lymphedema, chronicity of lymphedema, and arm circumferences.
Complex decongestive therapy
All patients were treated with CDT. Treatments consisted of an intensive circumference reduction phase, followed by a maintenance phase to stabilize extremity circumference. In the intensive circumference reduction phase, at least two certified skilled physical therapists completed a four-week CDT program, five times per week. Each session consists of a 30-minute manual lymph drainage, sequential gradient pumps, multiple compression wraps of low-tension compression bandages, specific therapeutic exercises,and skin care[13,14].
The purpose of the first phase was to obtain substantial circumference reduction [15]. After four weeks of CDT program, patients completed the self-management phase at home. Patients were taught self-massage,self-bandaging and therapeutic exercises.In addition, it was recommended to use bandages for more than 18 hours at least three times a week.
Circumferences measurement
Upper extremity circumference was measured at five levels using a soft tape: metacarpophalangeal joints, 5 cm above wrist joint, 10 cm below lateral epicondyle 10 cm above lateral epicondyle and axilla.The patients were supine with the arms at the sides of the body and elbows straight, then the circumference measurements were taken. Two measurements were made and their mean values were used. The difference of each circumference was calculated at all five levels. The position with the largest difference was taken as the observation index.
A method for determining the unilateral extremity lymphedema severity was based on the circumference difference between the affected and unaffected extremities (hereinafter referred to as circumference difference). The American Physical Therapy Association used circumference differences to assess the severity of lymphedema, which were classified as mild (<3 cm increased) in circumference difference,moderate (3-5 cm increased) or severe (> 5 cm increased) [16]. According to the pre-CDT lymphedema grading, patients were divided into three groups:group 1, mild lymphedema; group 2,moderate lymphedema;and group 3,severe lymphedema.
Statistical analysis
Statistical analysis was performed using SPSS version 21.0 for Windows. Continuous variables with normal distribution were presents as mean ± standard deviation (SD). Inter-group difference was compared using Chi-square test for categorical variables and one-way analysis of variance test for continuous variables.The pre-CDT data were used as the baseline and compared with post-therapy data by paired-samples T test. A value of P < 0.05 was considered significant.
Results
Descriptive characteristics
Table 1 shows the patients’ baseline characteristics.Fifty-eight patients were enrolled in this study,including 1 male. The average age was 57.7 ± 10.8 years. There were 19 cases (32.8%) of left arm lymphedema and 39 cases (67.2%) of right arm lymphedema. All patients had breast cancer surgery with ALND: 49 cases (84.5%) underwent modified radical mastectomy and 9 cases (15.5%) underwent breast conserving surgery.
When the patients were classified according to circumference difference between affected and unaffected extremity, 13 patients (22.4%) were placed in group 1 (<3 cm increased), 19 patients (32.8%)were placed in group 2 (3-5 cm increased) and 26 patients (44.8%) were placed in group 3 (>5 cm increased). The main clinical characteristics of the three groups of patients are compared in Table 2. The mean time from surgery to the lymphedema onset was 14.7 months in group 1, 18.1 months in group 2 and 16.5 months in group 3,with no statistically significant difference (P = 0.831). However, there was a significant difference in the lymphedema chronicity between these groups (P <0.001). The chronicity of lymphedema was 1.96 ± 1.76 years in group 1, 4.66 ±2.56 years in group 2 and 10.65±5.84 years in group 3.There were no statistically significant differences among the three groups in age (P = 0.072),chemotherapy (P = 0.518), radiotherapy (P = 0.458),type of surgery (P = 0.99), and affecting of the dominant arm (the dominant arm of all patients was right)(P=0.899).
Circumference difference
The mean values of circumference difference before CDT, right after CDT, 3 months and 12 months follow-up were shown in Table 3 and Figure 1. The circumference difference before and right after CDT,and 3 months follow-up in all the three groups showed a decreasing trend.
In group 1, the circumference difference decreased significantly from pre-CDT to post-CDT (P <0.001),which at 3-months follow-up, started to increase (P =0.011 compared with the value right after CDT),with a result at the 1-year follow-up in that we got an even higher value than the pre-CDT one (P = 0.175). The changing tendency of circumference difference in group 2 was similar to that in group 1. But the circumference difference at 1-year follow-up was significantly lower than the value right after CDT(P=0.002).
In group 3, the circumference difference decreased greatest at 3-months follow-up, and tended to increase at 1-year follow-up (P=0.74 compared with the value of 3-months-follow-up). At the time of post-CDT, 3 and 12 months follow-up, the differences were significantly lower than pre-CDT (P <0.001 for all).However, there was no significant increase in circumference difference in group 3 compared to pre-CDT during the maintenance phase.
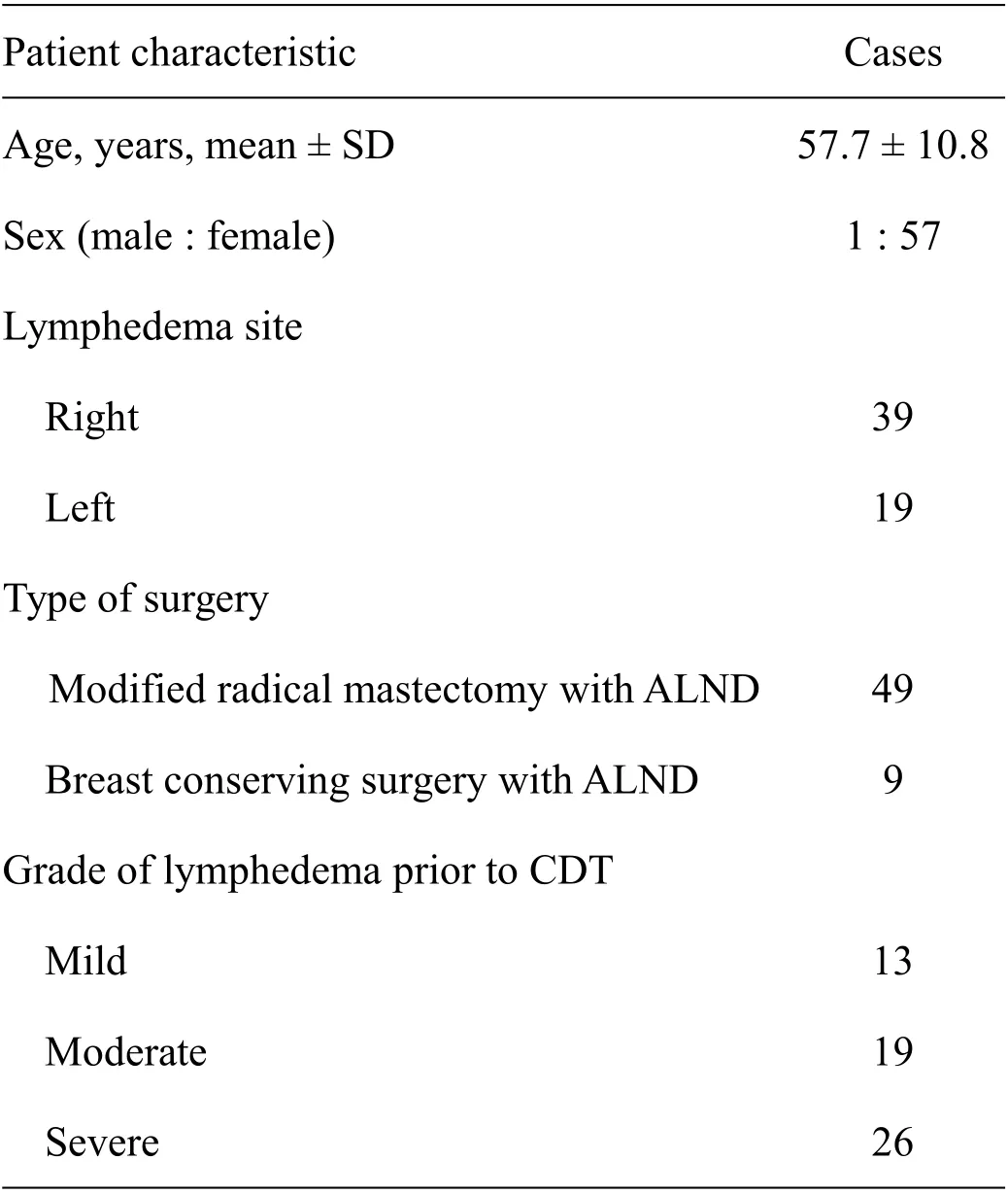
Table 1 Patients’baseline characteristics(n=58)
Discussion
This study investigated effects and safety of CDT on edema reduction after ALND in patients with breast cancer-related lymphedema. The patients were divided into three groups according to the difference of circumference between the affected and unaffected extremity before CDT. The different results in three groups were investigated.
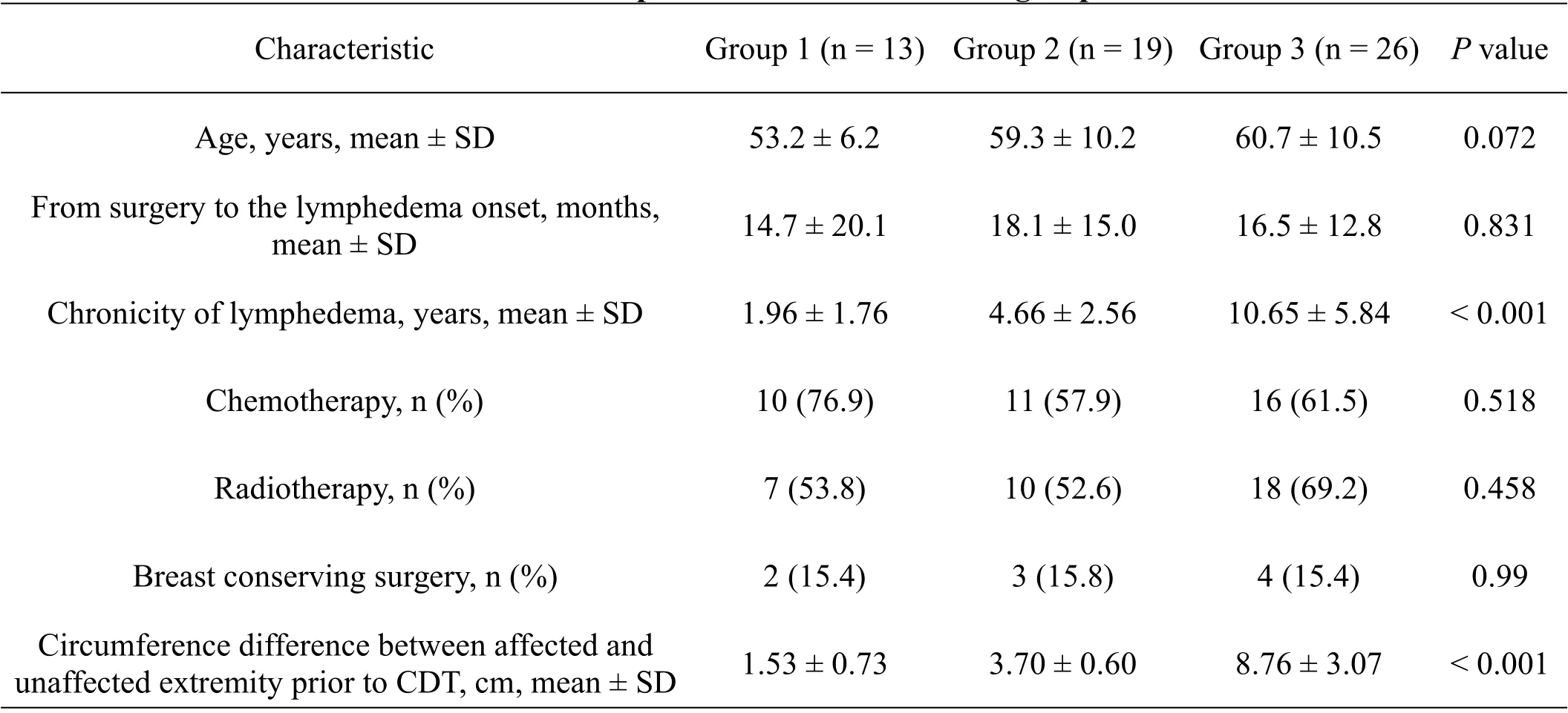
Table 2 Comparisons between the three groups
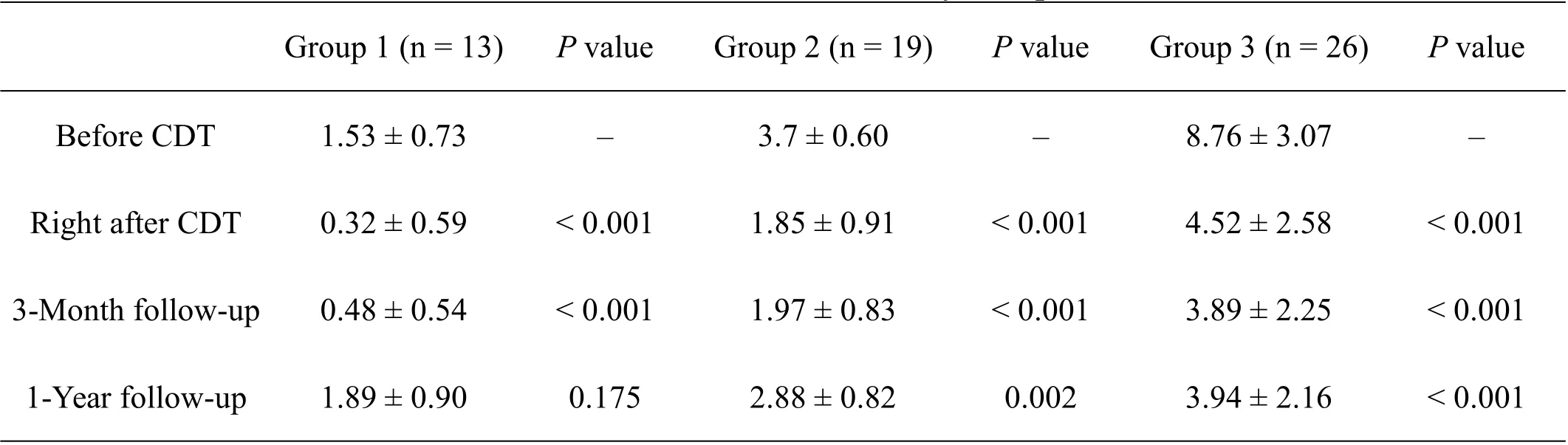
Table 3 Circumference difference at study time points(cm)
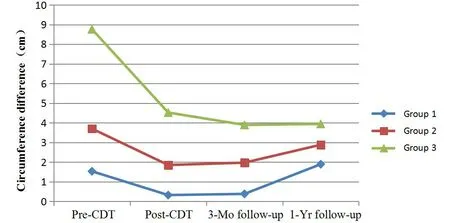
Figure 1 Distribution of circumference difference at study time points. Group 1, mild lymphedema; group 2,moderate lymphedema;group 3,severe lymphedema.
Comparing the results of the three groups, there were no statistically significant differences in age,time from operation to lymphedema onset, chemotherapy,radiotherapy, breast-conserving surgery, and affecting of the dominant arm. However, there was a significant difference in the chronicity of lymphedema among the three groups (P <0.001). The lymphedema chronicity of group 3 patients was more than 10 years, with significantly higher initial difference of circumference between the affected and unaffected extremity (P <0.001). This is consistent with other studies, which showed that the amount of initial swelling is associated with the duration of lymphedema[17,18].
Previous studies have reported a better response to CDT in patients with mild lymphedema, but this was inconsistent with our results[19].The result in group 1 showed that patients with mild lymphedema had good response to the treatment right after CDT, and tended to increase at 3-months follow-up.One year after CDT,the value of circumference difference increased again,and there was no significant difference from the initial one (P = 0.175). Nine cases (69.2%) cured (the difference of circumference between affected and unaffected extremity was less than 0.2 cm) in group 1 right after CDT, and did not strictly followed their home plans. This maybe contributed to the increased circumference difference. However, mild lymphedema did not deteriorate to moderate or severe lymphedema within 12 months. Untreated lymphedema progression was common, with one-third of patients with mild and moderate arm lymphedema patients progressing to higher grade within the first 5 years. Compared with our results, the absence of CDT progression over 12 months may be a meaningful effect.
CDT is found has a good therapeutic effect in BCRL after ALND for breast cancer, but there is a different progress according to the different initial grade of lymphedema. Traditionally, lymphedema has been considered a chronic progressive disease in which soft tissue becomes more fibrotic, making fluid more difficult to replace, and therefore less responsive to CDT [20]. In group 3, the circumference difference decreased from 8.76 cm to 4.52 cm (P <0.001) right after CDT, or from severe lymphedema to mild and moderate (17/26, 65.4%). The biggest drop in circumference difference was at 3-months follow-up,with an upward trend at 12-months follow-up.However, all of the circumference differences during the maintenance phase were lower than the value before CDT, significantly (P < 0.001). It may be considered that BCRL with a high initial circumference difference can be continuously improved through CDT.
Several limitations of this study are worth discussing. First, as a retrospective study, the adherence of patients could not be assessed. Second,there were natural differences in limb size, especially in dominant and non-dominant arms. In this study we compared the circumference of affected limb with that of non-affected one, but the volume change according to the natural difference was not analyzed. Third,patients with chronic lymphedema may have extensive tissue fibrosis,and CDT may play a smaller role.Thus,assessing fibrosis tended to more accurately assess CDT response. Further studies are needed to validate the relationship between fibrosis and response of CDT.
Due to these limitations,more researches are needed to confirm these findings. Nevertheless, the effectiveness of CDT in all three groups was significant. Therefore, it was important to encourage patients to receive CDT, whether mild or severe lymphedema.
- TMR Non-Drug Therapy的其它文章
- Neurophysiological basis of auricular acupuncture for the the treatment of p-chlorophenylalanine-induced insomnia
- Effects of electroacupuncture at auricular concha area on the circadian rhythm of melatonin secretion in p-chlorophenylalanine-induced insomnia rats
- The effects of Chinese herbal fumigation on the prevention of peripheral neurotoxicity caused by chemotherapy:a meta-analysis
- Research progress on the effect of the combination of Jing acupoints bloodletting therapy and Sangzhi (Mori Ramulus) on shoulder-hand syndrome after stroke
- Core acupoints of acupuncture for hyperplasia of mammary gland:a network analysis

