Differences in parents of pediatric liver transplantation and chronic liver disease patients
Sami Akbulut, Gulsen Gunes, Hasan Saritas, Bahar Aslan, Yunus Karipkiz, Khaled Demyati, Sukru Gungor,Sezai Yilmaz
Sami Akbulut, Khaled Demyati, Sezai Yilmaz,Department of Surgery and Liver Transplant Institute, Inonu University Faculty of Medicine, Malatya 44280, Turkey
Sami Akbulut, Gulsen Gunes, Department of Public Health, Inonu University Faculty of Medicine, Malatya 44280, Turkey
Hasan Saritas, Bahar Aslan, Department of Surgical Nursing, Inonu University Faculty of Nursing's, Malatya 44280, Turkey
Yunus Karipkiz,Department of Nursing Care Inonu University Faculty of Medicine, Malatya 44280, Turkey
Khaled Demyati, Department of Surgery, An-Najah National University Hospital, An-Najah National University, Nablus 11941, Palestin
Sukru Gungor, Department of Pediatric Gastroenterology, Inonu University Faculty of Medicine, Malatya 44280, Turkey
Abstract
Key words: Liver transplantation; Pediatric liver transplantation; Chronic liver disease;Parent satisfaction; Health-related quality of life health care parent satisfaction scale;Impact on family scale
INTRODUCTION
Since the first successful liver transplantation (LT) was performed by Starzl and colleagues in 1967, LT has become the gold standard treatment for both pediatric and adult patients with chronic liver disease (CLD). With advances in surgical techniques,effective antimicrobial prophylaxis, and improvements in potent immunosuppressive treatment options, 1-year and 10-year survival rates after pediatric LT have reached 95% and 80%, respectively[1]. With the prolongation of overall survival, quality of life and satisfaction after LT have become important issues for patients and their parents.In addition to studies comparing the quality of life before and after LT, many studies have compared the quality of life of LT patients and healthy individuals[1-3]. The primary aim of this study was to compare the satisfaction of parents of pediatric LT patients and that of parents of pediatric patients with CLD using the pediatric healthrelated quality of life (PedsQL) health care parent satisfaction scale and the impact on family scale (IFS). In addition, the study evaluated the relationships between education level, monthly income, and place of residence according to the PedsQL and IFS results.
MATERIALS AND METHODS
Study design
During this survey-bas ed study, parents of children who underwent pediatric LT between January 2010 and April 2017 at Inonu University Liver Transplant Institute were consecutively selected and included in the LT group. During the same period,the parents of children with CLD who underwent regular followed-up at the pediatric hepatology outpatient clinic of the same site were consecutively selected and included in the CLD group because their child’s LT indication was not yet established or they were on the LT waiting list.
Parents of 130 pediatric patients who underwent LT and survived were contacted by phone and details of the survey were shared with them. Although 105 of the parents accepted the invitation to participate, 14 were not included in the study because they were foreign nationals. As a result, 91 parents were eligible for inclusion in the LT group. Parents of 130 pediatric patients with CLD undergoing routine follow-up were informed about the survey, but 26 stated that they did not want to participate. Ten additional parents were excluded because they were foreign nationals. As a result, 94 parents were eligible for inclusion in the CLD group.
The survey was conducted by two researchers with previous experience performing survey studies. Ten parents were randomly selected from both groups to determine their comprehension of the questions. Both groups were compared in terms of number of children (one, two, three, or four or more), career (employed,unemployed, retired), education level (elementary school, middle school, high school,university), monthly income (< 1000 TL, 1000-3000 TL, > 3000 TL), place of residence(village, town, city), house where parents live (rent or own), and social assurance (yes or no). Both groups were also compared in terms of parameters of the PedsQL health care parent satisfaction scale and IFS scale.
The secondary aim of this study was to establish whether education level, monthly income, and place of residence were related to the IFS and PedsQL results. Therefore,information about education level (elementary school, middle school, high school,university), monthly income [low (< 1000 TL), middle (1000-3000 TL), high (> 3000 TL)], and the place of residence (village, town, or city) were compared according to the IFS scores and PedsQL scores. After approval was received from the Inonu University institutional review board for non-interventional studies (Approval No:2017/11-5), parents were contacted and the survey was conducted. Verbal consent was obtained to participate in the study.
Impact on family scale
According to the Turkish version of this scale, the reported internal consistency coefficient was 0.81 (Cronbach's alpha), the total correlation coefficient of the subparameters was 0.87-0.98, and the test-retest invariance coefficient was 0.79[4]. The IFS scale was used to assess the influence of the child’s health status on parents and consisted of four main subheadings: Financial impact (4 items); familial/social impact(9 items); personal strain (6 items); and mastery (5 items). Financial burden refers to economic consequences for the family. Familial/social impact refers to the disruption of social interaction. Personal strain refers to the psychological burden experienced by the primary caretaker. Mastery refers to the coping strategies used by the family[5].The total impact score was calculated using the total scores obtained from the first three main subheadings (excluding the mastery score). After a few items were removed from the Turkish version, parents were asked to answer the remaining 24 Likert-type questions (strongly agree = 1, agree = 2, disagree = 3, strongly disagree =4). Parents’ responses to items were reverse-coded to calculate scores (1 = 4 points, 2 =3 points, 3 = 2 points, 1 = 4 points). The total score was obtained by summing the points of the 24 items and varied between 24 and 96 points; a lower score indicated lower impact and a higher score indicated higher impact[4].
PedsQL health care parents satisfaction scale
According to the Turkish version of this scale, the reported internal consistency coefficient was 0.93 (Cronbach’s alpha), total correlation coefficient of the subparameters was 0.39-0.72, and the test-retest invariance coefficient was 0.98[6]. The PedsQL was used to assess the satisfaction of parents regarding the health care provided to their child by health care workers. This scale consisted of six main subheadings: Information (5 items); family inclusion (4 items); communication (5 items); technical skills (4 items); emotional needs (4 items); and overall satisfaction (3 items). Parents were asked to answer the 25 Likert-type questions (never satisfied = 0;sometimes satisfied = 1; often satisfied = 2; almost always satisfied = 3; always satisfied = 4; not applicable = NA). The options marked by parents were converted to scores as described in the literature (0 = 0 points, 1 = 25 points, 2 = 50 points, 3 = 75 points, 4 = 100 points)[6].
Statistical analysis
Statistical analyses were performed using SPSS Statistics v25.0 (IBM Corp., Armonk,NY, United States). The continuous variables were expressed as median, interquartile range, and minimum-maximum. The categorical variables were reported as number and percentage. The Kolmogorov-Smirnov test was used to determine whether the quantitative variables showed normal distribution. The Mann WhitneyUtest was used to compare the two groups in terms of quantitative variables. Pearson’sχ2and Fisher’s exact test were used to compare the categorical variables. Kruskal-Wallis oneway analysis of variance pairwise comparison andχ2tests were used to compare more than two independent groups. APvalue < 0.05 was considered statistically significant.
RESULTS
Demographic and social features
A total of 185 parents 19 to 65 years of age were included in this survey-based study.Of the 91 parents in the LT group, 57 were males and 34 were females. Of the 94 parents in the CLD group, 51 were male and 43 were female. Statistical significance t differences were found between groups in terms of career (P< 0.001), monthly income(P= 0.016), and education level (P= 0.041); however, statistically significant differences were not found in terms of sex, number of children, place of residence,house where parents live, or social assurance (Table 1). In total, 75.8% of the parents in the LT group were unemployed and 44.7% of the parents in the CLD group were unemployed. Although the monthly income of 70.3% of the parents in the LT group ranged from 1000-3000 TL, the monthly income of 56.4% of the parents in the CLD group ranged from 1000-3000 TL. In total, 63.7% of the parents in the LT group and 47.9% of the parents in the CLD group finished elementary school.
PedsQL and IFS comparison
Both parent groups were compared according to the IFS and PedsQL scores (Table 2).Statistically significant differences were found between the groups in terms of financial impact (P< 0.001), familial-social impact (P< 0.001), personal strain (P<0.001), and total impact (P< 0.001); the LT group parents had higher scores for each of these categories. Statistically significant differences were found between the parent groups in terms of PedsQL scores regarding information (P< 0.001), family inclusion(P< 0.001), communication (P< 0.001), technical skills (P< 0.001), emotional needs (P< 0.001), and overall satisfaction (P< 0.001); the LT group parents had higher scores for each PedsQL domain.
Education, monthly income, and place of residence
Statistically significant differences were found between the education level subgroups interms of the IFS domains of financial impact (P= 0.003), familial-social impact (P=0.008), personal strain (P< 0.001), and total impact (P< 0.001). However, these differences were not found in terms of the IFS domain of mastery (P= 0.404) or the PedsQL domains of family inclusion, communication, technical skills, emotional needs, and overall satisfaction (Table 3).
Statistically significant differences were found between the monthly income level subgroups in terms of the IFS domains of financial impact (P< 0.001), familial-social impact (P< 0.001), personal strain (P= 0.001), and total impact (P< 0.001). However,these differences were not found in terms of IFS mastery (P= 0.828) or the PedsQL domains of family inclusion, communication, technical skills, emotional needs, andoverall satisfaction (Table 4).
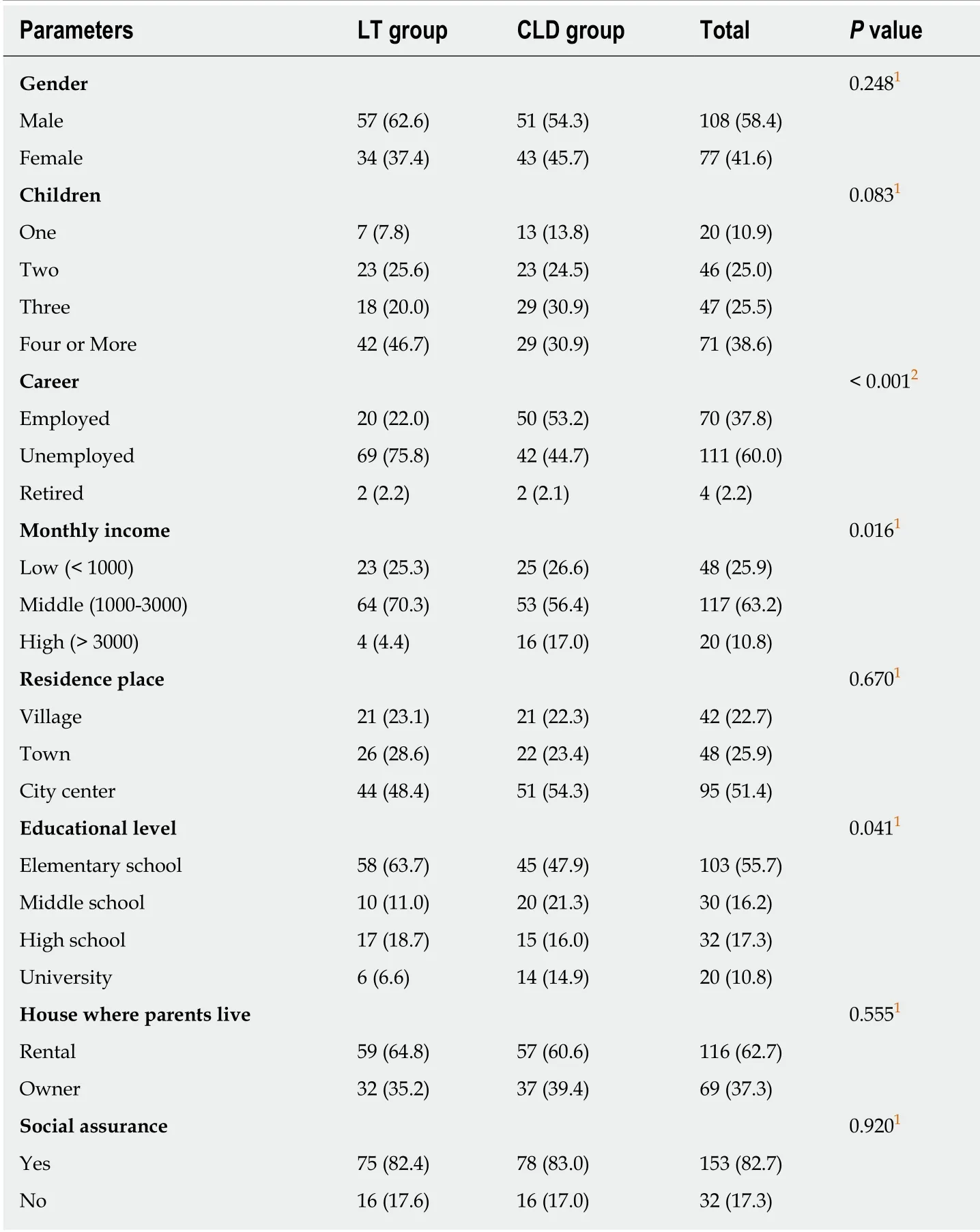
Table 1 Comparison of liver transplantation and chronic liver disease groups in terms of demografic and social parameters, n (%)
Statistically significant differences were found between the place of residence subgroups in terms of IFS domains of personal strain (P= 0.023) and total impact (P=0.027). However, these differences were not found for other IFS parameters or any of the PedsQL domains (Table 5). The results showed that there were inverse relationships between the education level, monthly income, and place of residence and difficulties that parents experience because of their children's health status.However, no relationship was found between education level, monthly income, and place of residence and satisfaction with the health care services provided in the hospital.
DISCUSSION
The burden of liver disease continues to grow worldwide[7,8]. Pediatric CLD affects not only the quality of life and health care satisfaction of the patient but also those of the patient’s family; in addition, illness in a family member may result in a heavy financial burden for the family[9]. Of course, parents feel it is their responsibility to give their children a happy life, and they often feel guilty when first facing thediagnosis of a chronic illness in their child[10]. Parents need a collaborative relationship with health care providers as a key component of family-centered care because the role of the family is critical to promoting successful outcomes and adaptation to chronic illness[11].

Table 2 Comparison of liver transplant and chronic liver disease groups in terms of pediatric health-related quality of life and impact on family scale results
Pediatric LT has become a gold standard therapeutic modality for children with end-stage liver disease. It offers hope for children and families when the child is diagnosed with CLD. After successful LT, the life of the recipient is saved and the quality of life is substantially improved. However, pediatric LT patients are medically fragile and present with complex care issues requiring high-level management in the home. Pediatric LT leads to chronic medical conditions and has been identified as a disease with a high number of readmissions[12]. However, the outcomes of LT for the pediatric population have improved significantly over the past two decades.Unfortunately, as long-term survival improves, potential complications related to immunosuppression, delayed growth and development, and metabolic issues are seen more commonly in long-term survivors. Because children who undergo LT need lifelong medication with immunosuppressants to prevent potential graft rejection,they are more vulnerable to infection and adverse drug reactions. Furthermore, it has been shown that children with LT have mean intellectual and mathematical skills scores that are significantly lower than the normative mean and are at higher risk for developing learning difficulties in terms of mathematics than the general population.This further adds to the functional, psychological, and financial difficulties of the parent who caring for and supporting a child with CLD[13].
As long-term survival of children following LT improves, it is important to examine the quality of life for these children and their families, as well as their personal experiences and satisfaction related to their health care. Although LT is lifesaving and presumably enhances the quality of life, the child remains affected by a chronic condition that includes morbidities, such as long-term management of biliary complications, renal dysfunction, risk of de novo malignancies, and a life-long need for immunosuppression. These challenges pose a potential burden with varying impacts on patients and their families. Pediatric LT patients have significantly lower health-related quality of life relative to healthy children, especially due to absencefrom school, whereas LT patient scores for social and school functioning were comparable to those of cancer patients[14].

Table 3 Comparison of pediatric health-related quality of life and impact on family scale results in terms of educational level subgroups
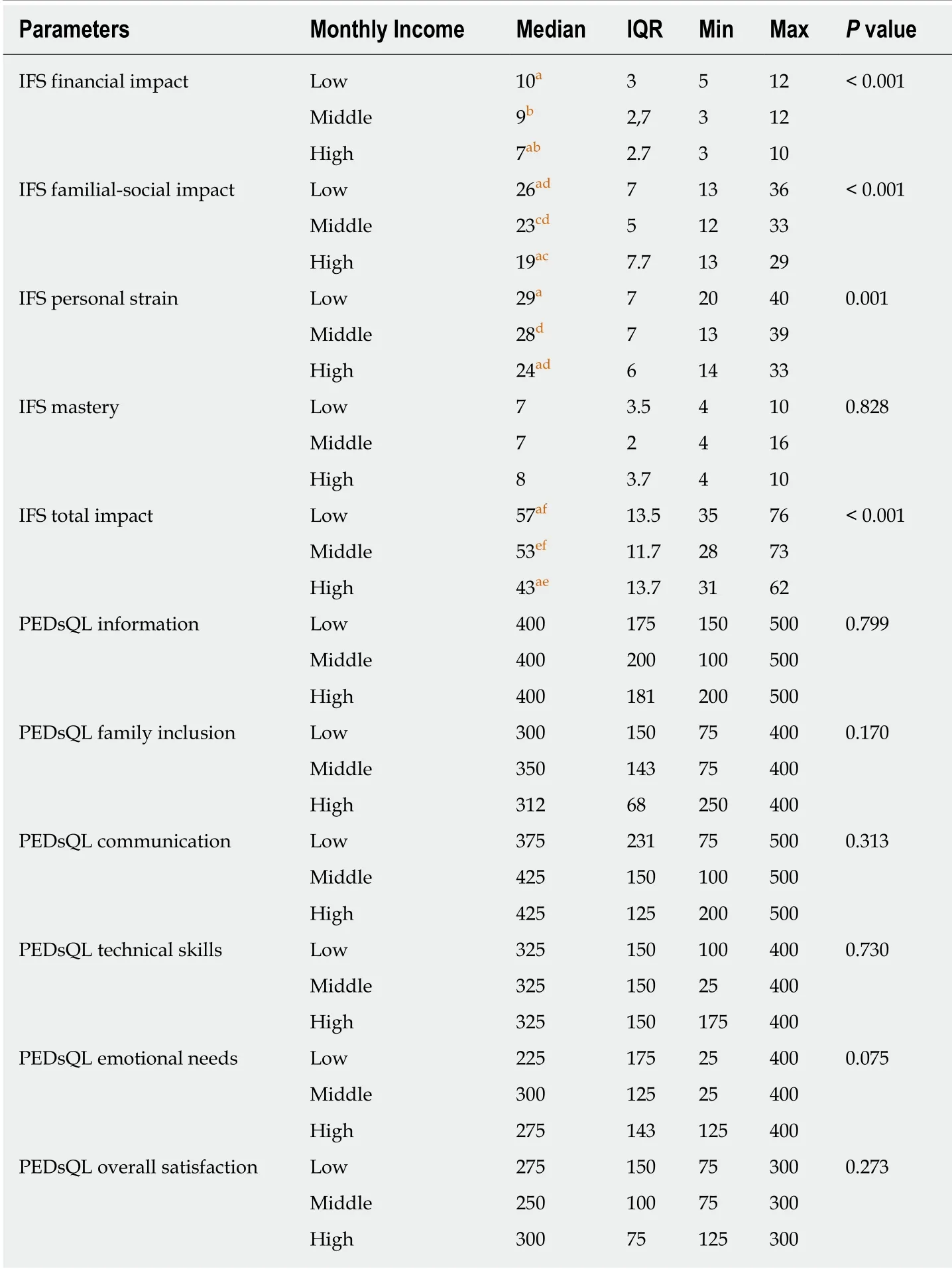
Table 4 Comparison of pediatric health-related quality of life and impact on family scale results in terms of monthly income subgroups
In addition to the emotional, physical, and financial impacts of LT on parents,research of family psychosocial needs following LT has indicated that parents of children who have undergone transplantation experience symptoms of emotional trauma[15]. A multi-center analysis of health-related quality of life and family function indicated that parents reported significant levels of family stress, and that parents of older transplant recipients reported higher levels of stress[2].
This study showed that parents of LT patients have more difficulties due to their children’s health status, which affects many areas of their lives, than parents of CLD patients. Furthermore, the IFS scores of the LT group correlated significantly with education and income levels; scores were higher for those with lower incomes and lower education levels. This may be due to the increased pressure experienced bylow-income families when children with CLD undergo LT. For example, additional travel to the transplant center for frequent follow-up appointments, expensive medications, and frequent hospitalizations are all part of the LT process. LT imposes tremendous long-term financial and emotional constraints on parents.
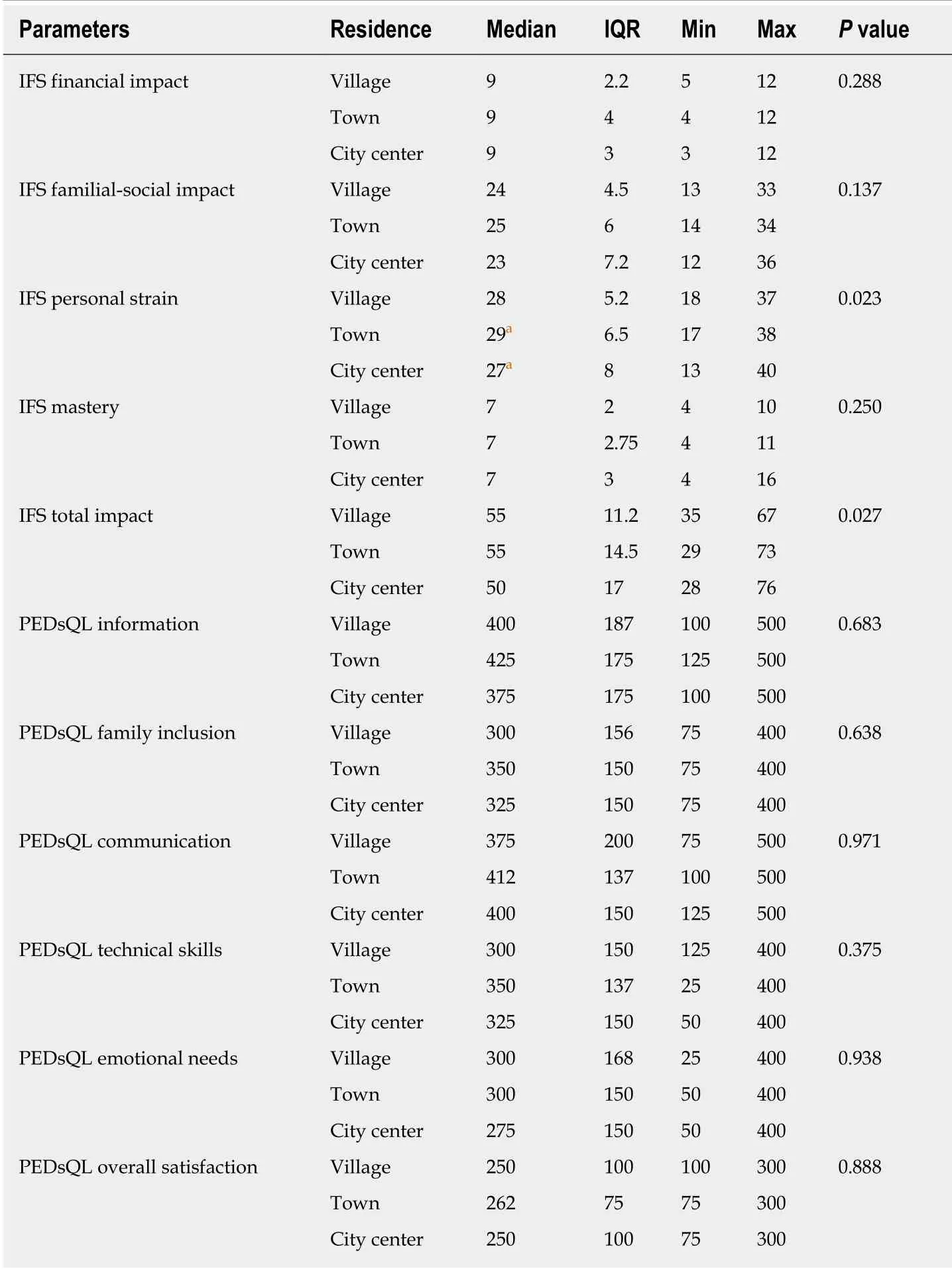
Table 5 Comparison of pediatric health-related quality of life and impact on family scale results in terms of residences place subgroups
Although the IFS scores were higher for the LT group than for the CLD group, the satisfaction scores of parents in the LT group regarding their child’s health care were higher than those of parents in the CLD group. The feeling that they have done everything possible to save their child might contribute to this satisfaction reported by the LT group. Moreover, the level of care at the transplant center in terms of comfort and the advanced comprehensive facility offered at this center compared to the general pediatric hepatology clinics might also contribute to the improved satisfaction scores. The satisfaction scores were not significantly affected by the education and income levels of the parents.
Coping styles not only affect the health of the parents but also influence the child[16].For example, a qualitative study performed in China to examine the parental coping strategies of parents whose children underwent LT found that most parents had a proactive approach to coping with the diagnosis, treatment, and care of the illness[10].Therefore, it is important to understand what stressors might affect the parents so that appropriate interventions can be designed to help alleviate them.
In conclusion, chronic illness is a major source of stress for pediatric patients and their families. Although children with end-stage liver diseases are saved by LT, their health-related quality of life is impaired compared to that of healthy controls. Parents of pediatric LT patients have more difficulties due to their child’s health status, but they have better health care-related satisfaction levels. It is recommended that, in addition to medical follow-up after LT, psychological and financial support should be offered to the patients and their parents throughout the follow-up process.
ARTICLE HIGHLIGHTS
Research background
Parents of children with chronic liver disease (CLD) and those who undergo liver transplantation (LT) have severe emotional, physical, and financial difficulties which affect their quality of life. While LT save treat CLD, pediatric LT patients remain medically fragile and present a complex care issues requiring high-level management in the home. In this study we aim to assess the impact of pediatric LT on parent’s quality of life and to study their satisfaction with treatment to better understand their needs.
Research motivation
Parents feel it is their responsibility to give their children a happy life and cure them from diseases, however in the case of pediatric LT; children remain affected by a chronic condition that includes morbidities, repeated hospitalizations and a life-long need for immunosuppression.Parents have more difficulties due to their children’s health status, which affects many areas of their lives. We aim to study the impact of LT on the life of pediatric patients after transplantation to highlight areas where intervention and assistance might be needed to help parents cope with the requirements of complex of the complex management of their children.
Research objectives
The main objective of this study is to assess the satisfaction of parents of pediatric LT patients and that of parents of pediatric CLD patients. Data from this study would help us to evaluate if this pediatric LT is associated with better parents satisfaction and better quality of life, and to highlight areas where intervention and assistance might be needed by these parents.
Research methods
During this survey, data were collected from parents of 91 pediatric patients who underwent LT and parents of 94 pediatric patients with CLD. Group comparisons were made based on the pediatric health-related quality of life (PedsQL) health care parent satisfaction scale, Impact on Family Scale (IFS) and demographic characteristics. Demographic variables such as education level, monthly income, and place of residence were compared between CLD and LT parent groups. Finally, PedsQL and IFS results were also analyzed according to demographic variables.
Research results
A total of 185 parents aged 19 to 65 years were included. According to the PedsQL results, family inclusion, communication, technical skills, emotional needs, and overall satisfaction were significantly different between the groups; the LT group had consistently higher scores.Additionally, scores for the IFS parameters of financial impact, familial-social impact, personal strain, and total impact were consistently higher for the LT group.
Research conclusions
While children with CLD are saved by LT, their health-related quality of life is impaired compared to that of healthy controls. Parents of children who underwent LT were very satisfied with the health care services provided to their children. However, they had more difficulties than parents of children with CLD. These data further stress the importance providing continuous social and financial support to families of pediatric LT patients to help them with the psychological, financial and health care difficulties they have.
Research perspectives
Quality of life and satisfaction after LT have become an important issue for pediatric patients and their parents. Parents feel satisfied with the medical management when their children have LT and offered their chance of cure by advanced medical procedures, however they pass into severe difficulties after LT as their child health remain fragile and require complex long-term management for the associated morbidities including repeated hospitalization. More evidencebased information is needed to describe and assess the impact of pediatric LT on parents and to better understand their needs.
 World Journal of Clinical Cases2020年11期
World Journal of Clinical Cases2020年11期
- World Journal of Clinical Cases的其它文章
- Tumor circulome in the liquid biopsies for digestive tract cancer diagnosis and prognosis
- Isoflavones and inflammatory bowel disease
- Cytapheresis for pyoderma gangrenosum associated with inflammatory bowel disease: A review of current status
- Altered physiology of mesenchymal stem cells in the pathogenesis of adolescent idiopathic scoliosis
- Association between liver targeted antiviral therapy in colorectal cancer and survival benefits: An appraisal
- Peroral endoscopic myotomy for management of gastrointestinal motility disorder
