Accuracy of carbon dioxide insufflation for endoscopic retrograde cholangiopancreatography using double-balloon endoscopy
Yoshiki Niwa, Masanao Nakamura, Hiroki Kawashima, Takeshi Yamamura, Keiko Maeda, Tsunaki Sawada,Yasuyuki Mizutani, Eri Ishikawa, Takuya Ishikawa, Naomi Kakushima, Kazuhiro Furukawa, Eizaburo Ohno,Takashi Honda, Masatoshi Ishigami, Mitsuhiro Fujishiro
Abstract
Key Words: Retrograde cholangiopancreatography; Double-balloon endoscopy; Carbon dioxide insufflation; Anastomosis; Accuracy; Prospective study
INTRODUCTION
Previously, biliary stones in patients with altered gastrointestinal (GI) anatomy were treatedviaa percutaneous trans-hepatic approach, however, this approach is sometimes challenging and may require a long therapeutic period in order to reach the stones[1]. In 2008, retrograde cholangiopancreatography (ERCP) using a short type of double-balloon endoscopy (DBE) called double-balloon endoscopic retrograde cholangiography (DBERC) was reported by Matsushitaet al[2]and biliary stones were able to be treated during a single endoscopic procedure. Since then, improvement in the endoscopic equipment was made and access to the blind end and subsequent treatment became easier[3-5]. A multicenter prospective study demonstrated that the mean time required to reach the blind end was 22.4 min and the therapeutic success rate was 97.9%[6].
However, in patients with a longer blind loop, severe adhesions, or a past history of hepatectomy, reaching the blind end for biliary drainage is still challenging[7]. The proper route at the bifurcation of the jejunojejunal anastomosis, as in Roux-en-Y reconstructions, or the gastrojejunal anastomosis, as in Billroth II reconstructions, is sometime difficult to be identified. When the incorrect route is initially selected, the examination and treatment time becomes much longer, as the endoscopist must return to the anastomosis in order to choose the correct path. It has been reported that the type of reconstruction may also affect the time required to reach the blind end as well as the ERCP success rate[7]. The correct selection of the route at the anastomosis can lead to a decreased insertion time. Yanoet al[8]reported that the direction in which sprayed indigo carmine solution flowed due to peristalsis indicates the afferent loop of a Roux-en-Y anastomosis, and that the alternate route should be selected. The correct route was selected in 80% of the patients in their study Fukubaet al[9]used carbon dioxide insufflation enterography (CDE) to confirm the correct route. In this method, the endoscopist inserts the tip of the endoscope into one of the two tracts at the branch and insufflate carbon dioxide (CO2) with an obstruction created by the inflation of an endoscopic balloon. Fluoroscopy is used to determine the direction of CO2flow. However, their study had retrospective fashion and included small number of cases. The aim of this prospective study was to evaluate the usefulness of CDE during DBERC in patients with altered GI anatomy by prospectively investigating the accuracy of route selection using CDE at the branch of the anastomosis.
MATERIALS AND METHODS
Inclusion criteria was the consecutive patients who were scheduled to undergo DBERC from June 2015 to November 2017 at our institution. Exclusion criteria were the Patients with a poor general condition and emergent cases. Informed consent was obtained from each patient prior to his or her involvement in this study. A short-type double-balloon endoscope consisting of an EI-530B endoscope (effective length: 1.550 mm, working channel: 2.8 mm, FUJIFILM, Tokyo, Japan) and a TS13101 overtube (FUJIFILM, Tokyo, Japan) were used for each examination. CO2insufflation was performed in all procedures[7]. DBE insertion was performed by experienced endoscopists (Nakamura M and Yamamura T) and their assistants who held the overtube. Patients were placed under conscious sedation with diazepam (0.02 mg/kg) and pentazocine (7.5 mg) withleft lateral decubitus position. Analgesics were additionally and repeatedly used for 7.5 mg as necessary, based on the consciousness and pain of the patient during the procedure. Dexmedetomidine (loaded at 6 μg/kg/h for 10 min and maintained at 0.4 μg/kg/h) was administered concomitantly in patients in whom sufficient sedation was not achieved using diazepam and pentazocine[10]. General anesthesia was used in child and adolescent patients. The pancreatobiliary team (Kawashima H, Ohno E, and Ishikawa T) performed the ERCPs. After reaching the target site, the body position was changed to dorsal or abdominal to perform ERCP. We performed both visual observation and CDE route selection in each patient from the jejunojejunal or gastrojejunal anastomosis to the target of the jejunobiliary anastomosis or the original Vater papilla and compared the accuracies of both route selection methods. When the endoscope reached the anastomosis during DBERC, the main endoscopist selected one of two lumens as the visual observation (Figure 1, Evaluation 1). The lumen on the left was initially selected, and the lumen that made a sharp angle if side selection was not available (Figure 1). The endoscopist then advanced the endoscope by one stroke and inflated the balloon on the tip of the endoscope to avoid a backflow of carbon dioxide, as previously reported[9]. Carbon dioxide was added up to ten seconds under fluoroscopy until the endoscopist could estimate whether the selected route lead to the target (Figure 1, Evaluation 2). When carbon dioxide could be seen in the patient’s upper, right abdomen (Video 1), the selected route was considered to be correct. Then the endoscope was advanced and ERCP was performed. When CDE enhanced the pelvis (Video 2), the selected route was considered incorrect, and the endoscopist pulled back to the anastomosis and continued the procedure using the other route. In patients with the Billroth II reconstruction and a Braun anastomosis leading to the original Vater papilla, we initially selected the left route at Braun anastomosis. If the left route did not lead to the target, the center route was chosen. The definitions of correct and incorrect routes are shown in Figure 1. The primary endpoint was the correct rate of CDE for selection of the route to the target. Secondary endpoints were the comparison of correct rate between visual observation and CDE around the anastomosis and examination times. Regarding the relation between patient’s burden, the factors associated with the dose of sedation and analgesic were analyzed using logistic regression analysis. The study was registered in the University Hospital Medical Information Network and in a clinical trial registry (UMIN000018357), and was approved by ethic committee at Nagoya University Hospital (registration No. 2015-0228).
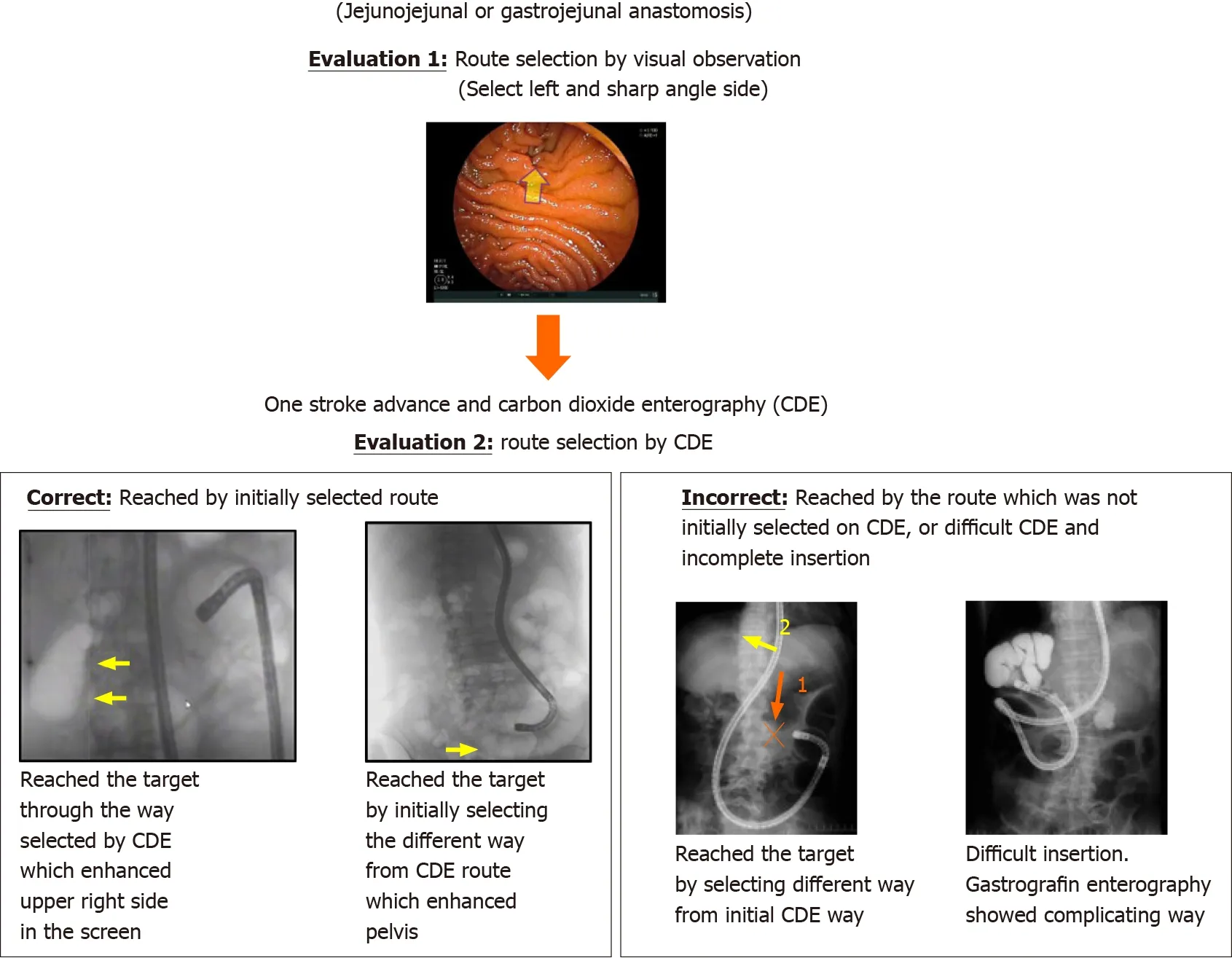
Figure 1 Jejunojejunal or gastrojejunal anastomosis. Evaluation 1 for route selection by visual observation and Evaluation 2 for route selection by carbon dioxide insufflation enterography. CDE: Carbon dioxide insufflation enterography.
Statistical analysis
SPSS version 26 for Windows (SPSS Inc., Chicago, IL, United States) was used to analyze the data in this study. The McNemar test was used to compare the rates of correct route selection between the two methods. The patients’ clinical results were compared using the Kruskal-Wallis test and the Mann-WhitneyUtest. Multiple logistic regression using the stepwise selection method was used to determine the effects of the dosages of sedation and analgesics in each patient. Statistical significance was set atP< 0.05.
RESULTS
We were able to reach the target in 50/52 patients (Table 1). The remaining two patients had severe adhesions that prevented the endoscopist from reaching the target. Thirty-three patients were included in the jejunojejunal anastomosis group (due to Roux-en-Y reconstruction and liver transplantation) and the gastrojejunal anastomosis group (due to Billroth II reconstruction and pancreatoduodenectomy) included 19 patients, six of whom had Braun anastomoses. The most frequent indication for ERCP was the treatment of biliary stones. Time from the branch to the target was likely to be longer than that from the incisor tooth to the branch.
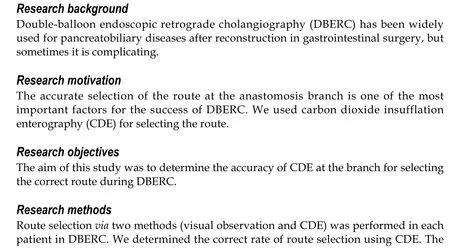
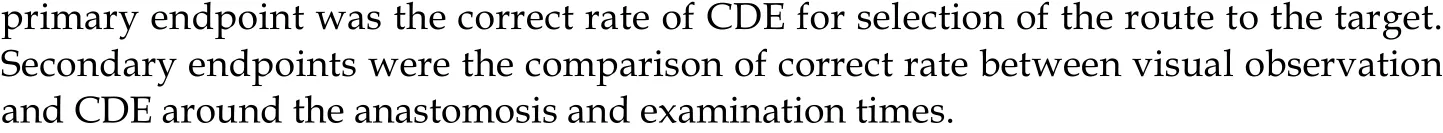
CDE was more accurate than visual observation in both groups (Table 2). The rate of correct route selection using CDE was higher in the gastrojejunal anastomosis group than in the jejunojejunal anastomosis group. Incorrect CDE in the patients with Braun anastomoses was occurred in 2/6 (33.3%) and higher than those without Braun anastomosis. Table 3 shows the patients’ clinical results for each group. Time from the branch to the target and total examination time were longer in patients with incorrect selection by CDE (n= 4). Of these four patients, the target was reached in two patients, one of who had too sharp angle at the branch to occlude the lumen and the other in whom the balloon attached on tip of endoscope was prolapsed to the anastomosis during CDE. Pancreatobiliary interventions were performed in 38 patients. To evaluate the relation between patient’s burden and DBERC, the factors associated with the doseof sedation and analgesic were analyzed using logistic regression analysis. We found no significant relationships between patient factors and the required dose of midazolam, though a higher analgesic dose was significantly associated with an age < 65 years (Tables 4 and 5). There were not any adverse events related to DBE insertion in this study.
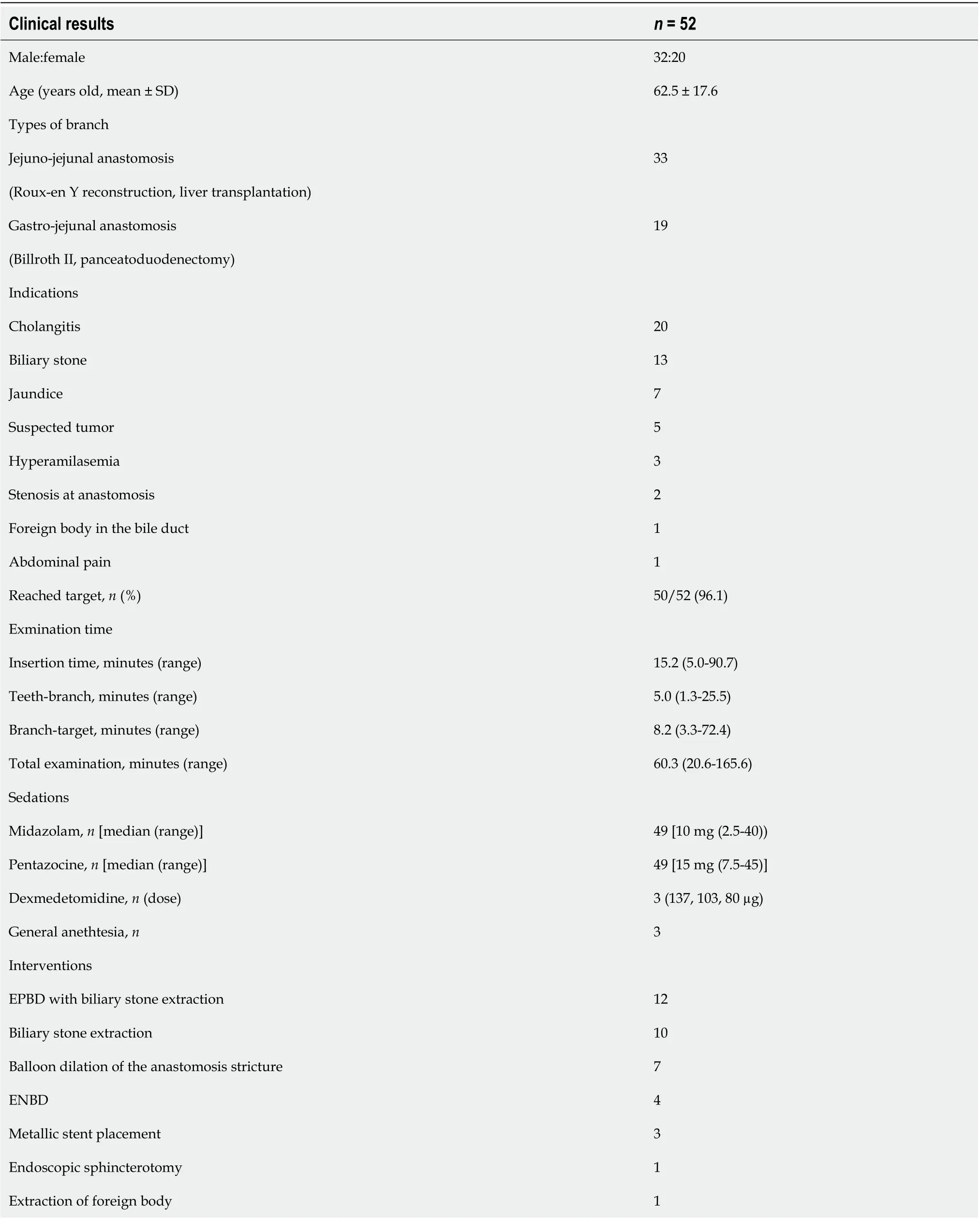
Table 1 Clinical results of ouble-balloon endoscopic retrograde cholangiography
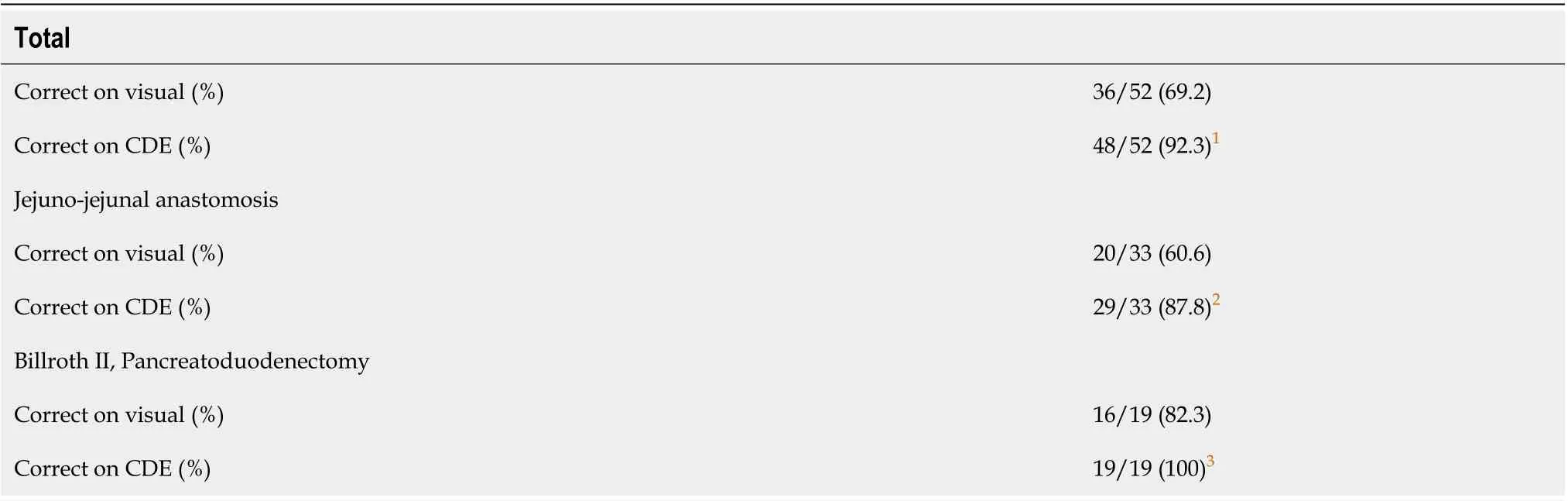
Table 2 Correct rate for route selection
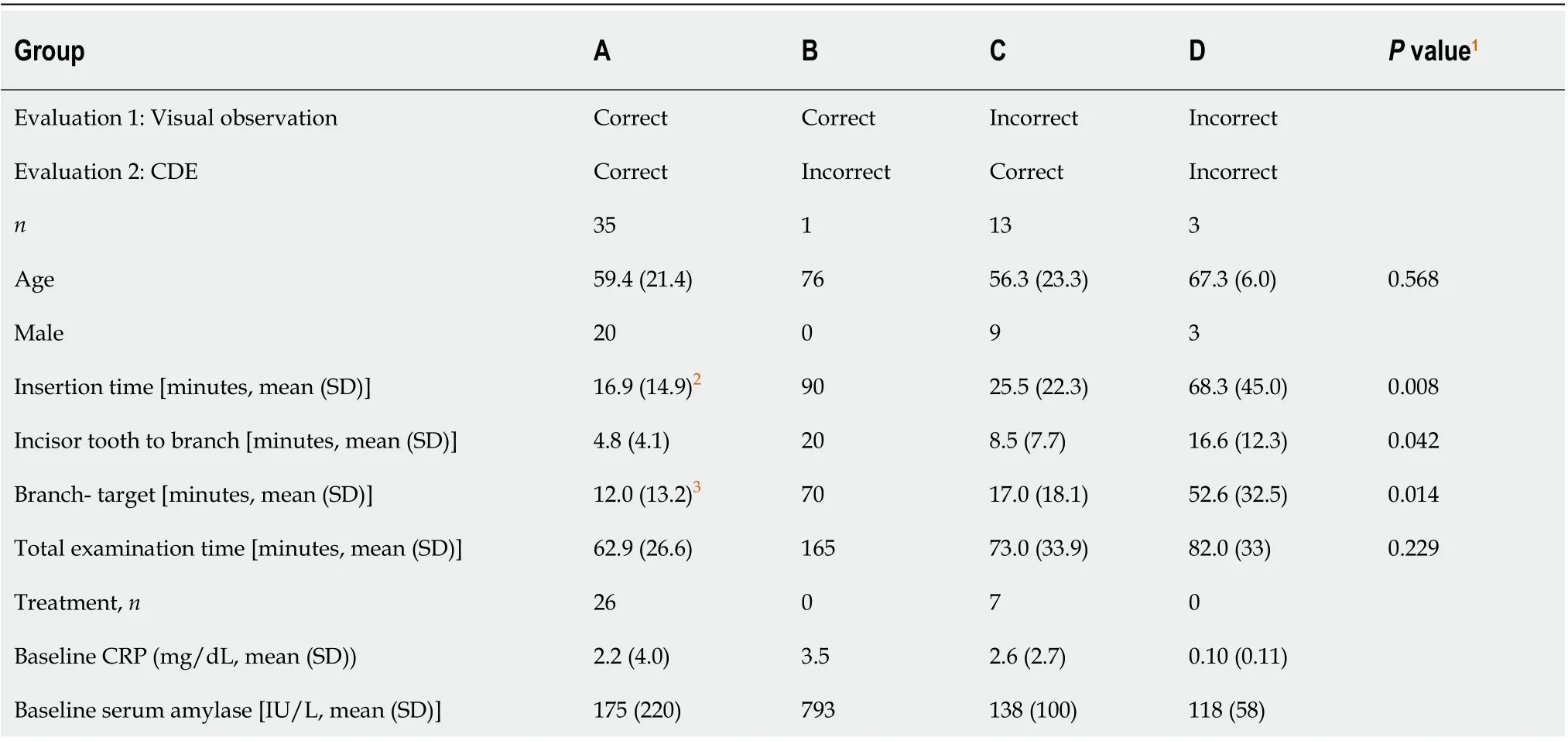
Table 3 Comparison of clinical results according to evaluation groups
DISCUSSION
This was the first prospective study to evaluate the results of CDE for selecting the route to the target during DBERC. These results indicated that CDE accurately selected the correct route at the anastomosis in patients with GI reconstruction who underwent DBERC. The mean total insertion time in this study was 15 min, which was shorter than that in the previous report[6]. When CDE accurately selected the route, the total insertion time was shorter. When visual observation is used to select a route, its accuracy cannot be determined until the target is reached. The use of CDE allows endoscopists to estimate the direction and distance of the target prior to reaching it, which results in a decrease in the total insertion time. The CDE method takes approximately 30 s to complete, including 10 s of CO2insufflation. However, when CDE leads the endoscopist to choose the incorrect route, a longer total insertion time results. This emphasizes the importance of the accuracy of CDE.
When a balloon is used to occlude the lumen, insufflated CO2can only go forward.However, CO2can sometimes flow back to the main route to the cecumviathe small space between the lumen and balloon, in which situation, it is difficult to assess the routes as CO2is observed in all areas of the abdomen. CDE should be performed as soon as the balloon is inflated, when there is no space between the lumen and the balloon. In contrast, visual observation of the jejunojejunal branch was accurate in 60% of patients, which is comparable to the 50% that would be predicted based on having two, equal choices. The left side lumen often had a sharp angle at the branch and the endoscopist chose that way; however, it was not always correct. We believe that it was easy to rotate the anastomosis and the position was changeable by several factors, namely air insufflation volume, insertion technique, and bowel movement. The accuracy of the visual observation method was slightly higher in patients with gastrojejunal anastomoses, which are unlikely to be influenced by these factors.
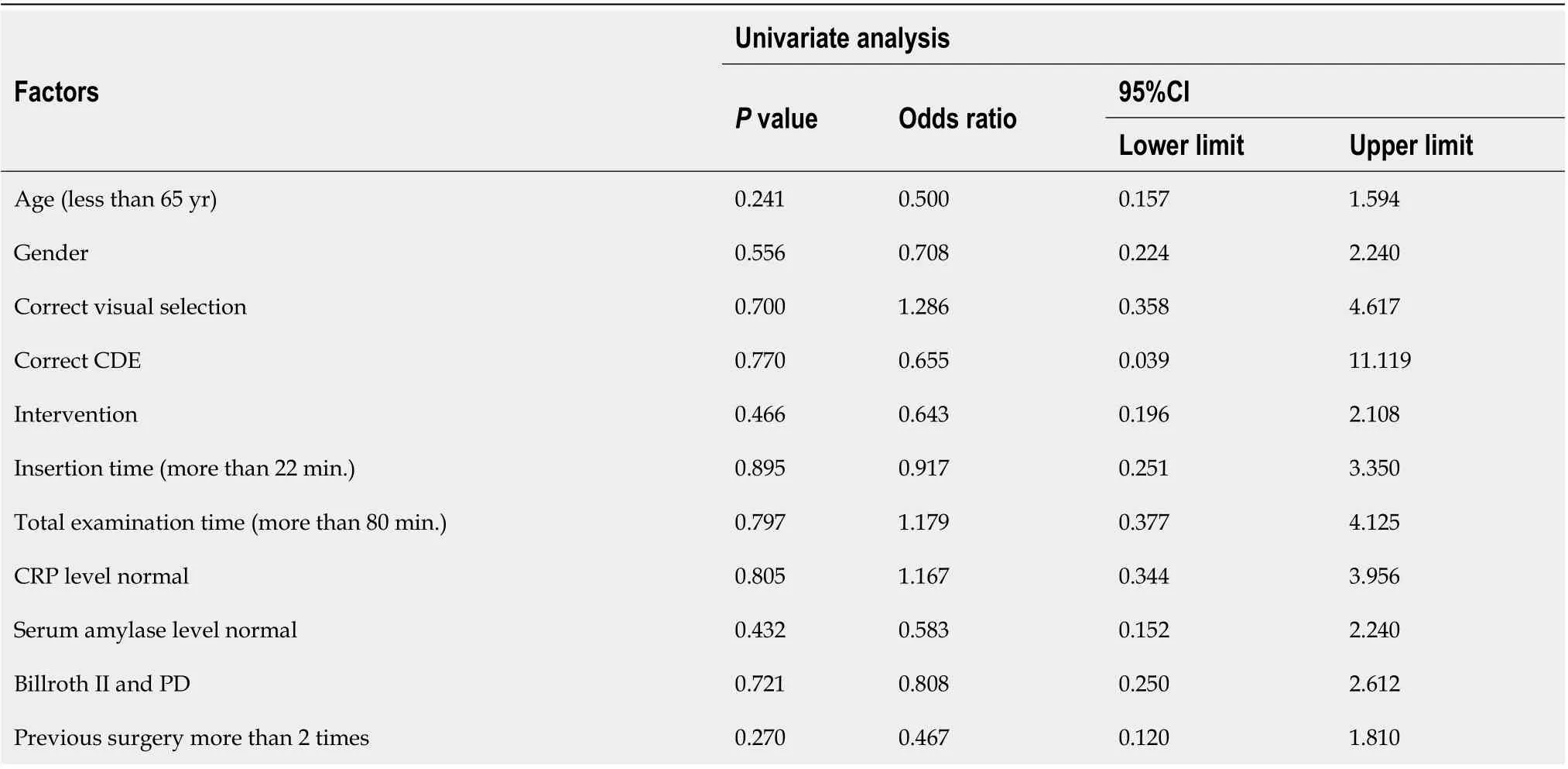
Table 4 Univariate analysis influencing factors for dose of sedation
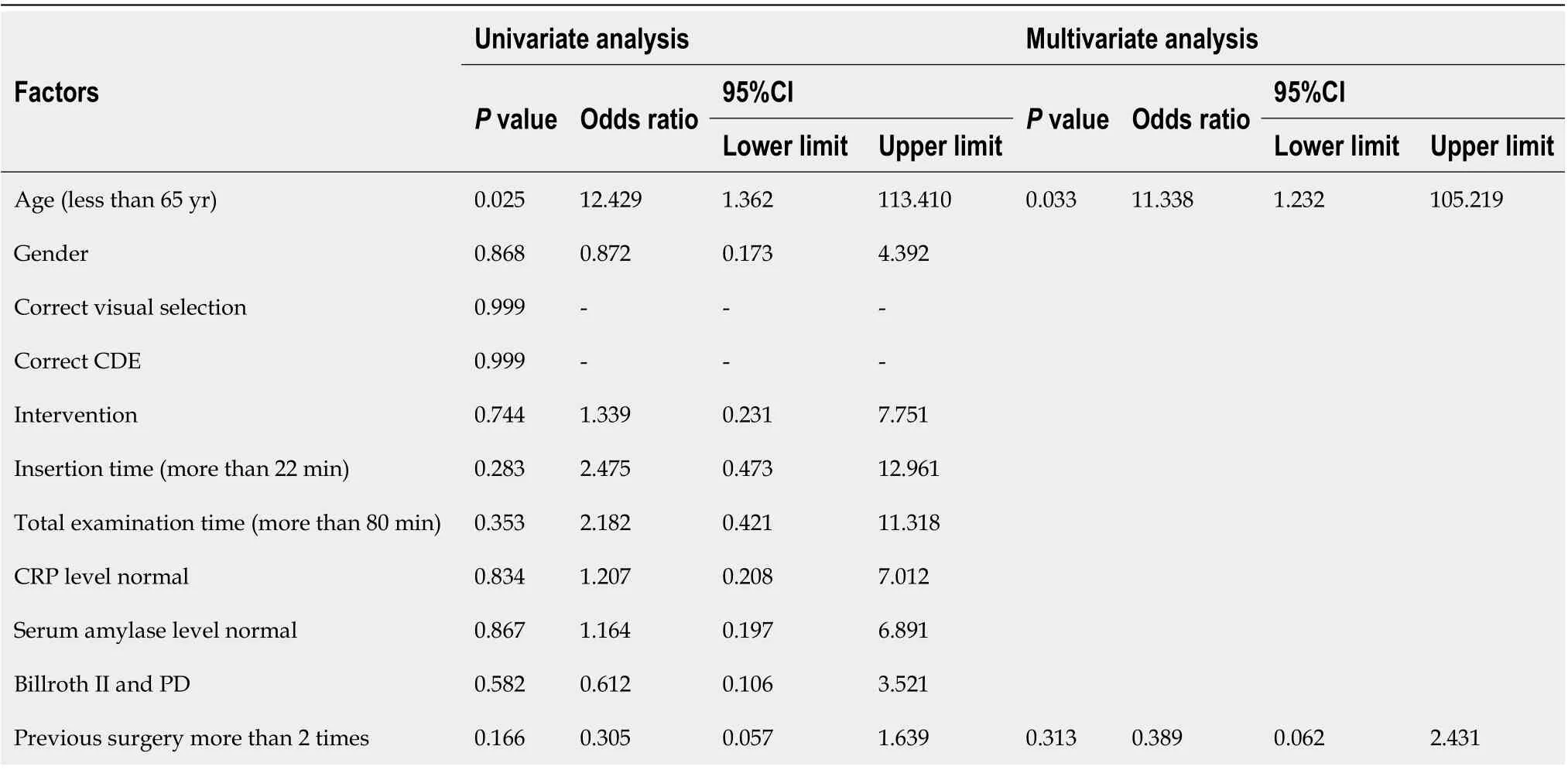
Table 5 Univariate and multivariate analyses influencing factors for dose of pentazocine
Yaneet al[11]reported that a pancreatic indication, the first ERCP attempt, and no transparent hood were statistically significant factors affecting procedural failure for short-type single-balloon enteroscope-assisted ERCP. Other insertion-related items besides transparent hood were not investigated. However, the procedural failure is also related to the procedure time, which can affect adverse events such as aspiration pneumonia and acute pancreatitis[12,13]. DBERC is a sequential procedure involving an insertion technique and biliary intervention. Adhesions and other factors can result in a challenging insertion of the endoscope into the GI tract. When insertion requires more than 60 min, a delicate technique should be used for subsequent biliary interventions. Based on our study, incorrect CDE may lead to an insertion requiring more than 60 min (Table 3). In patients < 65 years old, longer insertion times may lead to abdominal pain (Table 5). Therefore, accurate CDE is important to reduce the patient’s burden and improve safety.
In patients with reconstructed GI tracts, success of DBERC is highly dependent on the exact anatomy. The DBERC endoscope insertion and procedural success rates in patients with stenosis of the anastomosis site after liver transplantation have been reported as 68%-85% and 78%-88.2%, respectively, and are lower than the success rates in patients who underwent other GI reconstruction procedures[14-17]. This may be due to the fact that endoscope insertion and therapeutic procedures are more difficult due to changes in hepatic volume and afferent loop length after such surgery[7]. In patients who have undergone a hepatectomy, the selection of the correct route at the hepaticojejunostomy anastomosis is important to access the target site in a timely manner.
DBERC has a learning curve. The time required to complete the DBERC procedure in this study, especially the time required to reach the blind end, is less than that in previous reports[18,19]. This indicates that endoscopists who have experience maneuvering the DBERC may have shorter examination times. However, the procedure duration time still had a wide range. Some difficult cases inevitably require a long duration to complete the procedures. It is challenging to perform procedures within the expected duration, and this problem may be overcome by the improvement of endoscopes and devices[20].
This study had several limitations. First, it includes a small sample size in which both methods were used in the same patient. The result and performance of the second evaluation method depended on the first evaluation. A randomized, comparative study between CDE and visual observation for the proper route selection is necessary.
CONCLUSION
In conclusion, CDE is able to accurately select the route at the anastomosis in patients with GI reconstruction who are undergoing DBERC.
ARTICLE HIGHLIGHTS
Research results
We enrolled 52 consecutive patients scheduled for DBERC at our institution from June 2015 to November 2017. We were able to reach the target in 50/52 patients. The rate of correct route selection using visual observation and CDE were 36/52 (69.2%) and 48/52 (92.3%), respectively (P= 0.002). The rate of correct route selection using CDE in patients with a jejunojejunal anastomosis was 29/33 (87.8%), and the rate in patients with a gastrojejunal anastomosis was 19/19 (100%).
Research conclusions
CDE was able to accurately select the route at the anastomosis in patients with gastrointestinal reconstruction who are undergoing DBERC.
Research perspectives
Using CDE, DBERC will be performed safely and easily for patients who underwent any gastrointestinal reconstruction. A randomized, comparative study between CDE and visual observation for the proper route selection is necessary.
 World Journal of Gastroenterology2020年42期
World Journal of Gastroenterology2020年42期
- World Journal of Gastroenterology的其它文章
- could microRNA expression tell us more about colorectal serrated pathway carcinogenesis?
- Vascular anomalies associated with hepatic shunting
- Prognostic role of artificial intelligence among patients with hepatocellular cancer: A systematic review
- Case series of three patients with hereditary diffuse gastric cancer in a single family: Three case reports and review of literature
- Intussusception due to hematogenous metastasis of hepatocellular carcinoma to the small intestine: A case report
- Fedora-type magnetic compression anastomosis device for intestinal anastomosis
