Fluoxetine, a selective serotonin reuptake inhibitor used clinically, improves bladder function in a mouse model of moderate spinal cord injury
Long Ma , Jing-Yuan Tang , Jin-Yong Zhou, Chen Zhu Xin Zhang Ping ZhouQiu Yu Yan Wang Xiao-Jian Gu
Abstract After spinal cord injury, the upward conduction of the spinal cord is lost, resulting in the loss of micturition control, which manifests as detrusor sphincter dyssynergia and insufficient micturition. Studies have shown that serotonergic axons play important roles in the control of the descending urination tract. In this study, mouse models of moderate spinal cord contusions were established. The serotonin agonists quipazine (0.2 mg/kg), 8-hydroxy-2-(di-n-propylamino) tetralin (8-OH-DAPT, 0.1 mg/kg), buspirone (1 mg/kg), sumatriptan (1 mg/kg), and rizatriptan (50 mg/kg), the serotonin reuptake inhibitors fluoxetine (20 mg/kg) and duloxetine (1 mg/kg), and the dopamine receptor agonist SKF-82197 (0.1 mg/kg) were intraperitoneally administered to the model mice 35 days post-injury in an acute manner. The voided stain on paper method and urodynamics revealed that fluoxetine reduced the amount of residual urine in the bladder and decreased bladder and external urethral sphincter pressure in a mouse model of moderate spinal cord injury. However, fluoxetine did not improve the micturition function in a mouse model of severe spinal cord injury. In contrast, the other serotonergic drugs had no effects on the micturition functions of spinal cord injury model mice. This study was ethically approved by the Institutional Animal Care and Use Committee of Jiangsu Province Hospital of Chinese Medicine (approval No. 2020DW-20-02) on September 11, 2020.
Key Words: bladder; external urethral sphincter; fluoxetine; micturition; selective serotonin reuptake inhibitor; spinal cord injury;urodynamics; voided stain on paper measurement Chinese Library Classification No. R453; R744.2; R971+.2
Introduction
The neural circuits involved in micturition are controlled by the peripheral sensory system, the spinal cord, and the brain.Spinal cord injuries (SCIs) and injuries at the brain-stem level often disrupt the supraspinal tract, which controls micturition.When supraspinal control is lost, the coordinated contraction of the bladder and the external urethral sphincter (EUS)during voiding is greatly affected, often resulting in detrusor sphincter dyssynergia and low void efficiency (Taweel and Seyam, 2015). As a result, SCI patients gradually develop pathologically high intra-bladder pressure, causing bladder hypertrophy, abnormal pain, and urinary tract damage.Therefore, the recovery of the bladder function is often described as highly desirable among SCI patients (Estores,2003; Anderson, 2004; Han and Xu, 2020).
To improve functional bladder recovery, much attention has focused on pharmacological interventions (Kroll, 2017; White and Holmes, 2019; Tang et al., 2020). For example, several studies demonstrated that β3-adrenergic receptor agonists could alleviate hyperactive detrusor function post-SCI (Frazier et al., 2006; Andersson, 2017). Other studies demonstrated that the administration of serotonergic agonists could enhance micturition function in rats with chronic SCI (Dolber et al., 2007; Norouzi-Javidan et al., 2016). Supporting the impact of serotonergic inputs, treatment with serotonergic receptor antagonists was also shown to block the functional recovery mediated by the robust regeneration/sprouting of descending serotonergic axons (Lee et al., 2013; Lang et al.,2015). However, the development of effective drugs that are able to improve voluntary bladder control post-SCI remains preliminary. In this study, we established spinal contusion injuries of varying severity, and we screened a group of clinically used serotonergic drugs for urinary functional recovery by monitoring voiding patterns and urodynamics.
Materials and Methods
Experimental animals
Owing to the technical difficulty of bladder expression following spinal cord injury when using male mice, this study only included female mice. Adult female C57 mice(n= 99), aged 8 weeks, weighing 22-26 g, were obtained from the Laboratory Animal Center of Nantong University in China [license No. SCXK (Su) 2014-0001]. This study was ethically approved by the Institutional Animal Care and Use Committee of Jiangsu Province Hospital of Chinese Medicine(approval No. 2020DW-20-02) on September 11, 2020. All experiments were designed and reported according to the Animal Research: Reporting ofIn VivoExperiments (ARRIVE)guidelines. Age- and weight-matched animals were housed at room temperature (22°C) under a standard 12-hour light/dark cycle and were randomly assigned to sham or experimental groups. A flowchart of the experiments, including detailed information regarding the grouping of animals, the numbers of animals in each group, and the varying injury severities that were established, is presented inFigure 1.
Spinal contusion injury model
To generate the spinal contusion injury models, we first anesthetized mice using the nasal application of 2% isoflurane(2 L/min). We then performed a laminectomy at the thoracic level (T10) to remove the vertebra and expose the spinal cord underneath. Lateral clamps were used to stabilize the spinal cord. The contusion spinal injury was induced using an Infinite Horizon spinal cord impactor (Precision Systems and Instrumentation, Fairfax Station, VA, USA), applying either 70(moderate) or 90 (severe) kilodyne (kdyn; 1 dyn = 10-5N) of force (Matyas et al., 2017). In the sham group, the animals received a laminectomy but were not subjected to any contusion injury.
Drug treatment
We tested the acute effects of various drugs on voiding. The following drugs were administered intraperitoneally 35 days post-injury: normal saline; quipazine (0.2 mg/kg; Cat# Q1004;Sigma, St. Louis, MO, USA;n= 5) (Liu et al., 2017); 8-hydroxy-2-(di-n-propylamino) tetralin (8-OH-DPAT; 0.1 mg/kg; Cat#H8520, Sigma;n= 5) (Liu et al., 2017), SKF-82197 (0.1 mg/kg;Cat# S179, Sigma;n= 3) (Liu et al., 2017), fluoxetine (20 mg/kg;Cat# F132, Sigma;n= 9) (Lee et al., 2003), duloxetine (1 mg/kg; Cat# D044, Sigma;n= 7) (Wróbel et al., 2018),buspirone (1 mg/kg; Cat# B7148, Sigma;n= 6) (Myers et al.,2004), sumatriptan (1 mg/kg; Cat# 1642154, Sigma;n= 6)(Lychkova and Pavone, 2013); and rizatriptan (50 mg/kg; Cat#SML0247, Sigma;n= 6) (Langford et al., 2010) in total (see detailed information inFigure 1). All drug treatments were administered 30-120 minutes before the voided stain on paper (VSOP) assay was performed.
Behavioral assessment
We assessed all mice in each group (sham, 70, and 90 kdyn contusion injury) with the Basso Mouse Scale (BMS) (Bassoet al., 2006) at days 1, 3, 5, 8, 12, and 20 post-injury. The scores on the BMS range from 0 to 9 (0 indicates complete paralysis/loss of locomotion, and 9 indicates the full recovery of coordinated locomotion). This well-established scale was used to describe spontaneous locomotor recovery post-SCI.
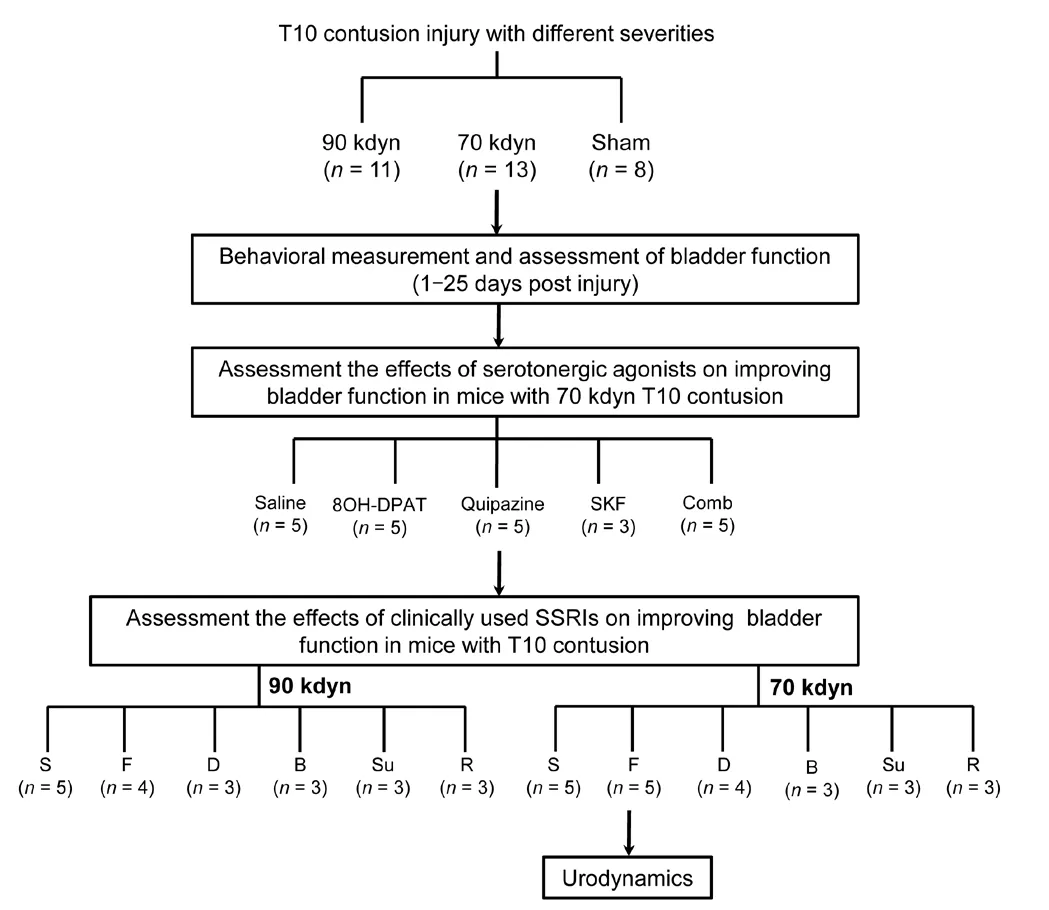
Figure 1|Experimental design flowchart.
Immunohistochemistry of tissue sections
To collect specimens for histological analyses, we first performed transcardial perfusion using 4% paraformaldehyde at 20 days post-injury. The whole spinal cord tissues were then post-fixed in 4% paraformaldehyde overnight, cryoprotected with 30% sucrose, and transversely sectioned into 40-μm-thick sections using a cryostat (Leica CM1950, Nussloch. Germany).Sections were blocked with 10% normal donkey serum,incubated with rabbit anti-glial fibrillary acidic protein (1:600;Cat# Z0334; DAKO, Glostrup, Denmark) at 4°C overnight. The sections were then incubated with the secondary antibody Alexa Fluor 488-conjugated donkey anti-rabbit IgG (1:200;Invitrogen, Waltham, MA, USA) at room temperature for 2 hours, and mounted onto slides using Fluoromount-G(Cat# 0100-01, Southern Biotech, Birmingham, AL, USA)mounting solution. Fluorescent images of transverse spinal sections were taken using a 20× lens on a Zeiss 710 Confocal microscope (Carl Zeiss Microcopy, White Plains, NY, USA).
Residual urine and VSOP measurement
We collected residual urine by manually expressing the bladder every 12 hours for 1-25 days post the contusion injury, starting 1 day post-injury. Mice were anesthetized with nasally applied 2% isoflurane (2 L/min) gas during bladder expression (David and Steward, 2010). Expressed urine was collected in a 1.5 mL tube, and the volume was measured. We also performed the VSOP assay (Sugino et al., 2008) to assess the effects of different drug treatments on bladder function.Briefly, we first generated a standard curve by placing different volumes of normal saline (50-800 μL) on filter paper (Whatman Cat# 05-714-5; Sigma-Aldrich, Cambridge,MA, USA). The stain areas were then marked, scanned,and analyzed using ImageJ software (version 1.8.0_172;National Institutes of Health, Bethesda, MD, USA) to obtain relative areas. A standard curve was generated by correlating the saline volume with the stained area. To normalize the hydration status among multiple animals, we supplied mice with distilled water (50 mL/g, subcutaneous injection)before the VSOP measurement. During VSOP, the animals were placed in a wire-netted cage on top of the filter paper(approximately 20 cm above). After 2 hours, the residual urine was manually expressed. The filter paper was placed under an ultraviolet (UV) light to clearly illuminate the urine stain(Hou et al., 2016). Urine stains were then marked, scanned,and measured with ImageJ to determine the relative area. The areas of all urine stains were added together and converted to a micturition volume based on the formula generated using the standard curve. The voiding efficiency was calculated as the ratio of the micturition volume to the sum of the micturition and residual volumes.
Urodynamic recordings and analysis
Terminal urodynamic recordings were performed as described in the literature, with modifications (Lee et al., 2013; Lang et al., 2015). Briefly, the mice were first anesthetized using urethane (0.8 g/kg, intraperitoneal injection), and then we carefully inserted a polyethylene catheter into the bladder through the urethra. To elicit repetitive voids, saline was constantly infused into the bladder at 40 μL/min. To monitor bladder pressure, we used the inserted catheter to infuse saline using a pressure transducer (Grass Technologies,Astronova Inc., West Warwick, RI, USA). To perform electromyography (EMG) recordings, two fine-hook electrodes were positioned surround the EUS. EMG signals were captured with a pre-amplifier (model 1700, A-M Systems) and digitized by Digidata Acquisition System (1440A; Molecular Devices,Silicon Valley, CA, USA). A band-pass filter of 10-1000 Hz and a sampling rate of 2000 Hz were applied to the recording.
Statistical analysis
For all figures, data are presented as the means, and error bars indicate the standard error of the mean (SEM). The number (n) of samples employed is indicated in the figure legends. For two-group comparisons, we chose the Student’st-test (two-way grouped). For comparisons between multiple groups, we performed a one-way analysis of variance or a repeated-measures of analysis of variance, with Bonferroni correction. Normality and homogeneity of variance were assessed by STATA (version 12; StataCorp LLC., College Station,TX, USA). Statistical analysis was performed using Prism 8.0(GraphPad Software, San Diego, CA, USA). Significance was set toP< 0.05.
Results
Generation of spinal contusion injuries of different severities at T10
First, we assessed the behavioral outcomes of inducing contusion injuries with different forces. Although in both groups, the BMS scores steadily increased post-injury, the hind limb locomotor recovery was significantly better in the group subjected to moderate force (70 kdyn) compared with the group subjected to a stronger (90 kdyn) force (Figure 2A). At 3 weeks post-injury, the mice in the moderate contusion injury group showed coordinated plantar stepping, achieving a mean BMS score of 6. In contrast, those in the stronger force contusion group only showed occasional plantar stepping, with a mean BMS score of 3 (Figure 2A). Histologically, immunoreactivity against glial fibrillary acidic protein, which serves as a marker for lesion-induced inflammation, showed that the area of the lesion epicenter was smaller in mice from the moderate contusion group (70 kdyn) compared with the group with more severe (90 kdyn) contusion injury (Figure 2B). These results suggested that the moderate contusion injury spared more descending tracts than the severe contusion injury.
Bladder function following spinal contusion injuries of different severities
We next assessed the bladder functions of animals following the generation of varying severities of spinal contusion injuries. Consistent with previous studies (David and Steward,2010), both moderate and severe contusion injuries resulted in compromised bladder function, as indicated by high residual urine volumes. In the moderate contusion group, the volume of expressible urine peaked 4 days post-injury and then declined until reaching a plateau at approximately 12 days post-injury, which remained significantly higher than that for the sham group (Figure 3). In contrast, the residual urine volume of mice in the severe contusion injury group remained high from days 4-20 post-injury (Figure 3), suggesting no spontaneous recovery of bladder function.
Serotonergic agonists improve micturition function in mice with moderate spinal contusion injuries
Previous studies suggested that the activation of serotonergic receptors could improve micturition function post-SCI (Dolber et al., 2007; Norouzi-Javidan et al., 2016). To further test this hypothesis, we treated mice with moderate spinal contusion injury with various serotonergic agonists, including quipazine and 8-OH-DPAT, which are both 5-hydroxytryptamine receptor 2A agonist. SKF-8219, a dopamine receptor (D1/D5) agonist,was used as a control. To assess the micturition function, we measured VSOP (Figure 4A). Both quipazine and 8-OH-DPAT significantly improved the voiding efficiency of mice with moderate spinal contusion injury (Figure 4B-E). In contrast,neither normal saline nor SKF-8219 showed any effects(Figure 4B-E), indicating the specific improvement of bladder functional recovery post-SCI in response to serotonergic agents.
Fluoxetine, but not other clinically approved serotonergic drugs, improves micturition function in mice with moderate spinal contusion injuries
To promote the translatability of this study, we tested the effects of a group of serotonergic drugs that are currently clinically approved. Among these drugs, the widely used selective serotonin reuptake inhibitor (SSRI) fluoxetine increased the voiding volume during the VSOP test, indicating improved voiding efficiency (Figure 5A-E). In contrast, the tested clinically approved serotonergic agonists did not improve micturition function (Figure 5B), likely because of a lack of specificity for the activation of serotonergic supraspinal axons, which is mediated by 5-hydroxytryptamine receptors.Fluoxetine treatment did not have any effects on micturition function in mice with severe spinal contusion injury (Figure 5A), which may indicate that all descending serotonergic axons might be severed.
Fluoxetine improves the quality of bladder function following moderate spinal contusion injury
To further investigate the quality of bladder function, we performed urodynamics assessments to measure bladder contractions and EUS activity during voiding in the sham and moderate spinal contusion injury groups. As shown inFigure 6, in the sham group, the EUS showed a basal level of tonic activity. Starting from the onset of voiding, when the bladder pressure rapidly increases, the EUS bursts phasically to coordinate with bladder contractions (Figure 6AandB). In contrast, following moderate spinal contusion injury, animals developed hyperactive, atypical EUS EMG bursting activity during both the non-voiding and voiding periods (Figure 6CandD). The administration of fluoxetine significantly diminished the amplitudes of bladder contractions and EUS EMG bursting activity during voiding (Figure 7A-D). However,we did not observe any overt improvements in coordinated EUS-bladder contractions during micturition. These results suggested that fluoxetine treatment might reduce bladder hyperreflexia and EUS hyperactivation post-SCI.
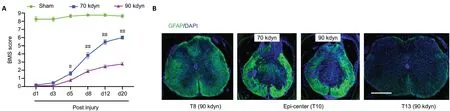
Figure 2|Characterization of T10 spinal contusion injury severity.
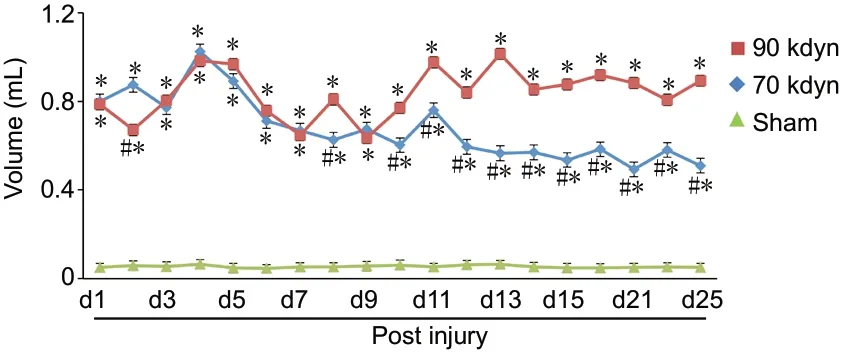
Figure 3|Time course of spontaneous voiding recovery following spinal contusion injuries of different severities.

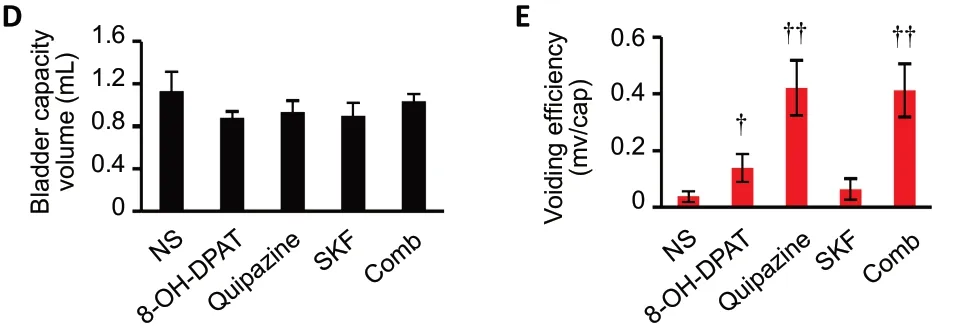
Figure 4|Serotonergic receptor agonists increase the voiding efficiency in mice with moderate spinal contusion injuries.

Figure 5|Fluoxetine specifically increased the voiding efficiency in animals with moderate T10 spinal contusion injury.
Discussion
In this study, after establishing T10 spinal contusion injuries of varying severities, we observed different levels of functional micturition deficits. The pharmacological study showed that the activation of serotonergic, but not dopaminergic,receptors was able to significantly improve void volumes and voiding efficiency. We then screened multiple clinically approved serotonergic drugs and identified the SSRI fluoxetine as a positive effector that was able to improve bladder function following moderate spinal contusion injury. These results indicate that fluoxetine may serve as a translatable treatment for improving micturition function post-SCI.
Multiple supraspinal nuclei are involved in micturition control,including both the bladder and the urethral sphincter. The most studied structure is the pontine micturition center (or Barrington’s nucleus), a nucleus located in the pontine area(Fowler et al., 2008). Other descending neurons, including serotonergic neurons that originate from the medullary raphe nuclei and noradrenergic neurons that originate from the locus coeruleus or the brain stem A5 area, are known to be involved in micturition control (Malykhina, 2017;Manohar et al., 2017). However, the specific roles played by distinct supraspinal tracts in micturition control remain largely unknown (Fowler et al., 2008; Hou et al., 2016; Keller et al., 2018; Yao et al., 2018). The SSRI fluoxetine improved functional bladder recovery but not duloxetine, which is a serotonin and norepinephrine reuptake inhibitor, suggesting that serotonergic and noradrenergic descending axons might play distinct and possible contradictory roles in micturition control.
Serotonin receptors are broadly expressed in the central nervous system, including in the lumbosacral spinal cord.Consistent with a previous study (Lang et al., 2015), our results showed that two traditional 5-hydroxytryptamine 1A/2A receptor agonists substantially increased both voiding volume and efficiency following moderate spinal contusion injury.However, the use of clinically approved 5-hydroxytryptamine receptor agonists at safe doses was unable to achieve a similar effect. In contrast, one clinically approved SSRI, fluoxetine, was able to significantly improve micturition function. Fluoxetine had no overt effects in animals with severe contusion spinal cord injury, suggesting that very few descending axons survived in the severe injury model. These results suggested that the specific activation of serotonergic supraspinal circuits is crucial for improved bladder function post-SCI.
Fluoxetine did not improve dyssynergia post-SCI, which suggested a low efficiency for the reformation of spontaneous supraspinal inputs originating from the medullary raphe nuclei or other micturition related nuclei. The extent of axonal regeneration or sprouting beyond the lesion site has been shown to be extremely restricted in the adult mammalian central nervous system (He and Jin, 2016; Tran et al., 2018; Courtine and Sofroniew, 2019). Various strategies have been applied to the promotion of axonal regeneration in the central nervous system, such as enhancing intrinsic neuronal growth properties or alleviating the extrinsic inhibitory environment (Lang et al., 2015; He and Jin, 2016;Carmichael et al., 2017; Liu et al., 2017; Rosenzweig et al.,2019). Combinatory strategies that include both clinically approved pharmacological treatments and methods that promote the regeneration of descending tract axons might achieve improved functional recovery for both moderate and severe SCI conditions. This study was limited by the focus on acute SSRI effects, and future studies will investigate whether the chronic administration of fluoxetine can facilitate the recovery of bladder function post-SCI. Our results showed that fluoxetine, a commonly used anti-depression drug,might help improve bladder function post-SCI, thus shedding light on potential therapeutic targets for the development of novel drugs to promote the functional recovery of micturition following SCI or other traumatic central nervous system injuries.
Acknowledgments:We thank the General Clinical Research Center at Jiangsu Province Hospital of Chinese Medicine, China for technical assistance.
Author contributions:Study design: LM, JYT, XJG; experiment implementation: LM, JYT, JYZ, CZ, XZ, PZ, QY, YW; manuscript writing: LM,JYT, XJG. All authors approved the final version of the manuscript.
Conflicts of interest:The authors declare no competing interests.
Financial support:This work was supported by Jiangsu Province Hospital of Chinese Medicine, No. Y19061 (to LM). The funder had no roles in the study design, conduction of experiment, data collection and analysis,decision to publish, or preparation of the manuscript.
Institutional review board statement:The study was approved by the Institutional Animal Care and Use Committee of Jiangsu Province Hospital of Chinese Medicine (approval No. 2020DW-20-02) on September 11,2020.
Copyright license agreement:The Copyright License Agreement has been signed by all authors before publication.
Data sharing statement:Datasets analyzed during the current study are available from the corresponding author on reasonable request.
Plagiarism check:Checked twice by iThenticate.
Peer review:Externally peer reviewed.
Open access statement:This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix,tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
Open peer reviewers:Luc Bauchet, Montpellier University Medical Center,France; H?z?r Ufuk Akdemir, Ondokuz Mayis University, Turkey.
Additional file:Open peer review report 1.
- 中國神經(jīng)再生研究(英文版)的其它文章
- Pharmacological interventions targeting nuclear factor-kappa B signaling in multiple sclerosis
- Corrigendum
- Proteolysis targeting chimera technology: a novel strategy for treating diseases of the central nervous system
- Notice of Retraction
- Luteolin delays photoreceptor degeneration in a mouse model of retinitis pigmentosa
- MicroRNA and mRNA profiling of cerebral cortex in a transgenic mouse model of Alzheimer’s disease by RNA sequencing

