Multimodal therapy in oligometastatic prostate cancer:A glimpse into the future?
Dear editor,
Since the introduction of radiotracer-labeled prostatespecific membrane antigen(PSMA)targeting positron emission tomography(PET),imaging of prostate cancer(PCa)improved drastically[1,2].Subsequently,metastases may be detected in earlier stages with possible implications on treatment planning[3].Here,we described the multimodal treatment approach on a young patient with newly diagnosed metastatic PCa conducted according to the results of repeated PSMA-PET imaging.
In September 2017,a 54-year-old man was referred to our hospital due to newly diagnosed PCa.A biopsy had revealed a Gleason score 4+4 in seven out of 13 cores with an initial prostate-specific antigen(PSA)of 29 ng/mL.Due to equivocal findings on abdominal magnetic resonance imaging(MRI),furtherGa-PSMA-11 PET/computed tomography(CT)staging was performed revealing multiple metastases to pelvic,as well as retroperitoneal lymph nodes(M1a)(Fig.1A and B).The patient presented with excellent performance status(ECOG 0)and no relevant comorbidities.According to STAMPEDE data,an inductive chemo-hormonal therapy with six cycles of Docetaxel combined with Leuprolinacetat was initiated[4].After termination of the chemotherapy,PSA had decreased to 0.02 ng/mL under continuous androgen deprivation therapy(ADT)and no residual disease was detected by a repeated PET/CT imaging usingF-rhPSMA-7,a probably more sensitive PSMA tracer without urinary excretion(Fig.1C).In July 2018,the patient underwent open radical prostatectomy with extended pelvic lymph node dissection.Final pathology yielded a ypT3b pN1(1/15)R0 L1 V0 Gleason 4+4 PCa with postoperatively undetectable PSA.On further follow-up,PSA slowly rose to 0.5 ng/mL in March 2019 under continued ADT.Therefore,F-rhPSMA-7 PET/CT was performed,detecting a single interaortocaval lymph node metastasis(Fig.1D).After detailed discussion with the patient,salvage lymph node dissection was planned.To assure detection of the suspect lesion,PSMA-radioguided surgery after injection ofTc-PSMA investigation and surgery(Tc-PSMA-I&S)and preoperative single photon emission computed tomography(SPECT)/CT imaging(Fig.1E)was performed in April 2019,as previously described[5].Preoperative PSA was 0.54 ng/mL.Final pathology revealed two lymph node metastases out of seven removed lymph nodes.At 6 weeks after surgery,PSA declined to 0.03 ng/mL.
In patients with newly diagnosed hormone-sensitive metastatic PCa,several studies have recently described survival benefits,when adding docetaxel,abiraterone,apalutamide and enzalutamide to hormonal therapy[4,6-8].Moreover,radiotherapy directed to the primary in addition to standard of care systemic therapy was shown to improve survival in newly diagnosed metastatic PCa patients with low metastatic burden(<4 bone metastases,no visceral lesions)as compared to standard of care systemic therapy alone[9].
Our patient received primary chemo-hormonal therapy in 2017,and hereafter underwent local therapy with radical prostatectomy due to significant PSA response and complete response on advanced molecular imaging as an individual and multimodal treatment approach[10,11].However,the sequence in which these modalities should be administered still remains matter of debate.Initiation of systemic therapy prior to local therapy might help to distinguish between patients with potentially less aggressive disease responding well to systemic treatment and who may benefit of additional local treatment compared to patients with systemic disease in whom local therapy might only be considered for palliative local symptom relief.
Unfortunately,in our patient,the PSMA-PET scan triggered by a rising PSA 1 year after termination of the initial chemotherapy revealed a new pelvic lymph node metastasis.Recent data showed promising results of salvage lymph node dissection with radioguided-surgery in initially non-metastatic,then recurrent PCa patients[12].Specifically,complete biochemical response(PSA<0.2 ng/mL at 4-8 weeks’post-surgery)was demonstrated in 66%of these highly selected patients with a median biochemical recurrence-free survival of 19.8 months.Moreover,patients with low preoperative PSA-values and one single lesion in PSMA-PET imaging were more likely to experience complete biochemical response.Certainly,the mentioned study investigated initially non-metastatic patients with lymph node recurrent disease.Conversely,our patient had metastatic PCa at diagnosis,rather than a metastatic recurrence after initial definitive local therapy.However,previous data suggested a potential survival benefit of metastasis-directed therapy[13-15].
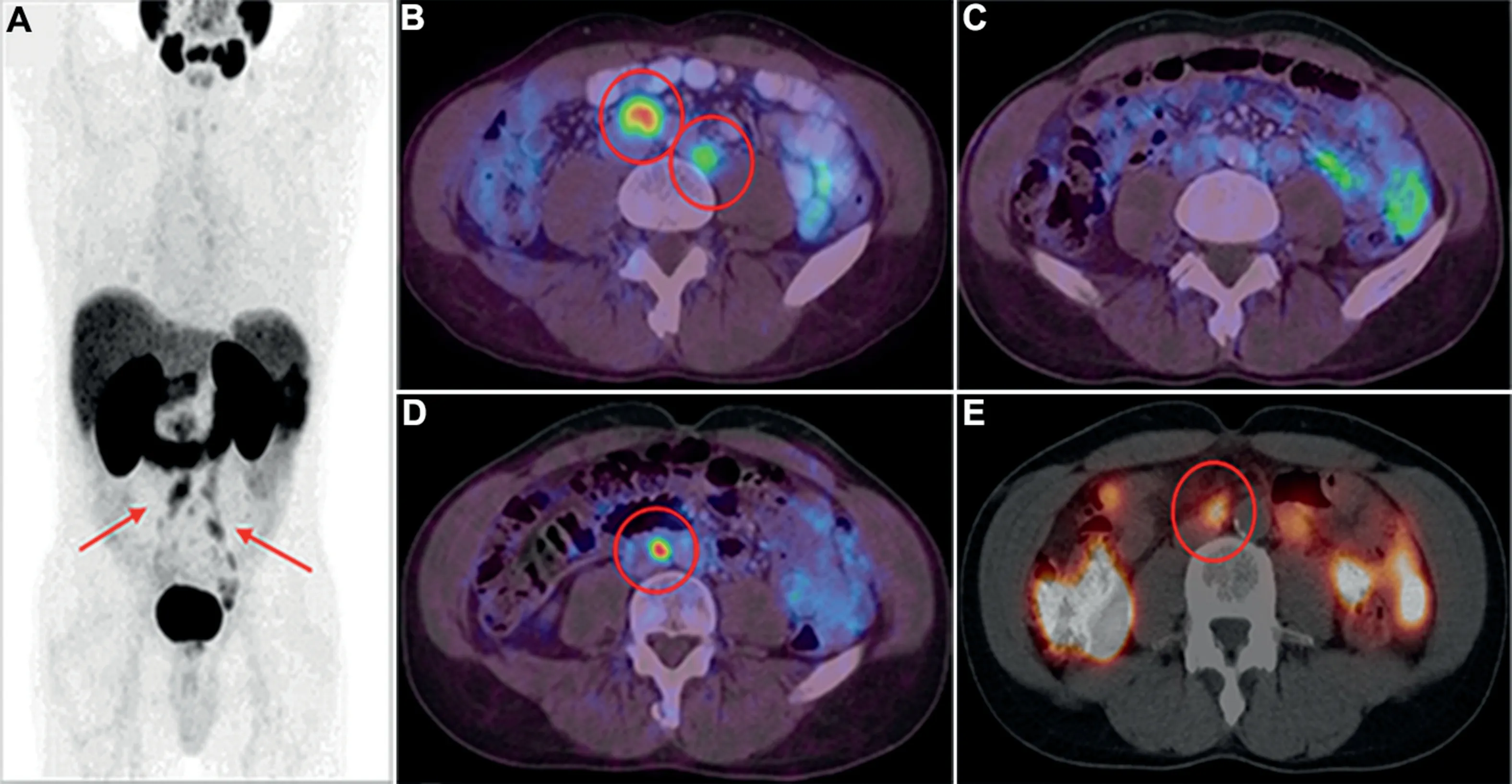
Figure 1 PSMA PET and SPECT imaging.(A)Initial 68Ga-PSMA-11 PET(maximum-intensity-projection)showing bilateral pelvic,as well as retroperitoneal lymphatic dissemination(arrows);(B)Example of initial retroperitoneal lymph node metastasis(circles;axial 68Ga-PSMA-11 PET/CT fusion image);(C)Complete remission of lymph node metastasis after chemo-hormonal therapy(axial 18F-rhPSMA-7 PET/CT fusion image);(D and E)Solitary recurrent retroperitoneal lymph node metastasis after radical prostatectomy(D.Axial 18F-rhPSMA-7 PET/CT fusion image;E.Axial 99mTc-PSMA-I&S SPECT/CT fusion image obtained prior to PSMA-radioguided salvage surgery).PSMA,prostatespecific membrane antigen;PET,positron emission tomography;SPECT,single photon emission computed tomography;CT,computed tomography;99mTc-PSMA-I&S,99mTc-PSMA investigation and surgery.
One common limitation of most previously published trials concerning treatment modalities in newly diagnosed metastatic PCa is the use of conventional imaging techniques.With PSMA-based PET imaging,sensitivity and specificity increased tremendously in comparison to conventional imaging[2].Therefore,earlier metastatic stages may be detectable,rendering comparisons to metastatic stages diagnosed by conventional imaging possibly difficult.In consequence,in metastatic patients diagnosed by PSMA-PET imaging,intensified active treatment may be considered more frequently in the future[3].However,there are several unsolved questions.It is unknown if the extension of lymphadenectomy(or radiotherapy)should follow the extension of metastasis of initial PET/CT to potentially avoid undertherapy.Moreover,it is unclear if survival may be prolonged by intensified treatment modalities.Nonetheless,although cure may not be possible in advanced stages,as visible by very low persisting PSA levels in the presented case,use of ADT may be delayed,which in itself has morbidity and mortality.Further studies are needed to find optimal treatment combinations and sequences including systemic,as well as local therapy options for these patients.
To date,the optimal sequence of treatments in newly diagnosed metastatic PCa with low metastatic burden is unclear,especially in patients diagnosed by PSMA-based PET imaging.In our experience,as highlighted in the presented case,a multimodal approach with systemic,as well as local(i.e.
surgical and radiotherapeutic)treatment may be considered in selected patients to achieve potentially longer survival.Ideally,such patients should be included in clinical trials.Author contributions
Study concept and design:
Tobias Maurer.Data acquisition:
Matthias Heck,Matthias Eiber,Tobias Maurer.Drafting of manuscript:
Sophie Knipper.Critical revision of the manuscript:
Sophie Knipper,Gunhild von Amsberg,Franziska Stolzenbach,Thomas Steuber,Matthias Heck,Matthias Eiber,Christoph Berliner,Tobias Maurer.Conflicts of interest
The authors declare no conflict of interest.
Sophie Knipper*
Martini-Klinik Prostate Cancer Center,University Hospital Hamburg-Eppendorf,Hamburg,Germany
Gunhild von Amsberg
Martini-Klinik Prostate Cancer Center,University Hospital Hamburg-Eppendorf,Hamburg,Germany
Department of Oncology,University Hospital Hamburg-Eppendorf,Hamburg,Germany
Franziska Stolzenbach
Martini-Klinik Prostate Cancer Center,University Hospital Hamburg-Eppendorf,Hamburg,Germany
Thomas Steuber
Martini-Klinik Prostate Cancer Center,University Hospital Hamburg-Eppendorf,Hamburg,Germany
Department of Urology,University Hospital Hamburg-Eppendorf,Hamburg,Germany
Matthias Heck
Department of Urology,Technical University of Munich,Munich,Germany
Matthias Eiber
Department of Nuclear Medicine,Technical University of Munich,Munich,Germany
Christoph Berliner
Department of Nuclear Medicine,University Hospital Hamburg-Eppendorf,Hamburg,Germany
Tobias Maurer
Martini-Klinik Prostate Cancer Center,University Hospital Hamburg-Eppendorf,Hamburg,Germany
Department of Urology,University Hospital Hamburg-Eppendorf,Hamburg,Germany
*Corresponding author.
E-mail address:
a.knipper@uke.de(S.Knipper)16 July 2019
 Asian Journal of Urology2021年2期
Asian Journal of Urology2021年2期
- Asian Journal of Urology的其它文章
- Super-mini percutaneous nephrolithotomy
- Are we progressing in prostate cancer management?
- Testicular germ cell tumors
- Bilateral ureteral reconstruction using appendicular interposition combined with Wallace anastomosis following stenosis after radical cystectomy and ileal neobladder construction
- Cystic nephroma:A bosniak III benign tumor in the kidney
- Expanding luminal epitheliums as cells of origin for prostate cancer
