Effectiveness of oral motor respiratory exercise and vocal intonation therapy on respiratory function and vocal quality in patients with spinal cord injury: a randomized controlled trial
,
Abstract Singing, as a method of combining respiratory function exercise and vocal intonation therapy, provides a new direction for respiratory function exercise in patients with spinal cord injury. This randomized controlled trial investigated the effects of oral motor respiratory exercise and vocal intonation therapy on respiratory function and vocal quality in patients with spinal cord injury. Among 31 included patients with spinal cord injury, 18 completed the treatment. These 18 patients were randomly assigned to undergo music therapy(intervention group, 30 min/d, 5 times a week, for a total of 12 weeks; n = 9, 7 males and 2 females; 30.33 ± 11.74 years old) or normal respiratory training (control group, n = 9; 8 males and 1 female; 34.78 ± 11.13 years old). Both patient groups received routine treatment concurrently. Before and at 6 and 12 weeks after intervention, a standard respiratory function test, a voice test, the St. George’s Respiratory Questionnaire, and a quality of life questionnaire were administered. The results showed that the inspiratory capacity, forced expiratory volume in 1 second, forced vital capacity, maximal mid-expiratory flow rate, sing-loud pressure level, and sustained note length were significantly increased in the intervention group compared with the control group. The St. George’s Respiratory Questionnaire and quality of life results of patients in the intervention group were significantly superior to those in the control group. These findings suggest that oral motor respiratory exercise and vocal intonation therapy, as respiratory training methods in music therapy, are effective and valuable for improving respiratory dysfunction and vocal quality in patients with spinal cord injury. This study was approved by the Ethics Committee of China Rehabilitation Research Center (approval No. 2019-78-1) on May 27, 2019 and was registered with the Chinese Clinical Trial Registry(registration number: ChiCTR1900026922) on October 26, 2019.
Key Words: central nervous system; clinical trial; injury; oral motor; randomized; repair; respiratory exercise; spinal cord
Introduction
Traumatic spinal cord injury (SCI) is a serious condition that poses challenging health problems (Shin et al., 2019).Respiratory dysfunction is a major cause of morbidity and mortality in SCI (Hoh et al., 2013) and is of particular concern as a severe consequence of cervical SCI. Respiratory dysfunction causes a reduction in lung volume and disruption of the respiratory system. Among an estimated 12,000 new cases of SCI annually, the reported respiratory failure rate among those hospitalized for cervical SCI is approximately 60%(Nguyen et al., 2020). Respiratory dysfunction is characterized by low lung volumes and a weak cough secondary to respiratory muscle weakness (Berlowitz et al., 2016). Weak respiratory muscles result in reduced lung volume, an increased number of respiratory tract infections, and reduced chest wall compliance (Alajam et al., 2019; DiMarco et al.,2019b). In addition, respiratory dysfunction can negatively affect vocal sound by reducing vocal loudness and decreasing phonation length (Cho, 2018).
Current studies have shown that injuries above the phrenic motor neuron level (C3-5) cause virtually complete paralysis of muscles involved in both inhalation and exhalation;therefore, treatment is mainly dependent on mechanical ventilation or phrenic nerve stimulation (Hoh et al., 2013).Research has shown that participation in respiratory training can effectively improve lung function in SCI patients (Shin et al., 2019). This therapy mainly focuses on training of muscular endurance and strength, which has a training effect on patients’ respiratory muscles. Although training is effective,patients find it tedious, boring, and difficult to maintain (Chiou et al., 2019).
Singing, as a vocal activity, has a great impact on the respiratory system, requiring strong and rapid inhalation,extension, adjustment of exhalation, and coordination of accessory respiratory muscles (DiMarco et al., 2019a). It is an important music therapy method. In recent years, increasing numbers of studies have examined the effectiveness of singing in lung function exercise, but most studies have focused on chronic obstructive pulmonary diseases (Lord et al., 2010, 2012, 2014; Pacheco et al., 2014; Skingley et al.,2014; McNaughton et al., 2016; Lewis et al., 2018; Alajam et al., 2019; Hardy et al., 2019). Singing may have positive effects on respiratory function in SCI patients (Tamplin et al.,2019) because accessory respiratory muscles are commonly recruited during singing (Tamplin et al., 2011). A previous report showed that singing could improve exercise endurance,ease breathing difficulties, and promote quality of life in SCI patients (Tamplin et al., 2013). Therapeutic singing refers to the use of singing activities for a variety of therapeutic purposes (Thaut and Hoemberg, 2014). This technique can synthesize a range of speci fic phonation, respiratory control,and vital capacity (VC) goals into an integrated therapeutic experience, thus providing follow-up exercise to other specific techniques such as oral motor respiratory exercise(OMREX) and vocal intonation therapy (VIT). In support of the respiratory function exercise, singing activities promote strengthening and control of the muscles used for breathing,thus increasing lung capacity (Santoni et al., 2020).
OMREX is a technique used to improve articulatory and respiratory control during singing (Thaut and Hoemberg,2014). Musical notes and exercises, mainly through sound vocalization, are applied to enhance respiratory control and function of the speech apparatus. This technique is often used for chronic obstructive pulmonary disease patients but is rarely used for SCI patients. VIT uses vocal exercises to train,maintain, develop, and rehabilitate issues of voice control caused by structural, neurological, physiological, or functional abnormalities of the voice apparatus (Thaut and Hoemberg,2014). It includes vocal control such as inflection, pitch,breath control, and timbre. Compared with singing alone,OMREX and VIT combined with singing could be used to train breathing and voice in a more systematic manner (Santoni et al., 2020). Both OMREX and VIT start with the melody interval of unit tone singing and gradually transition to a short melody line. When combined with singing, these techniques help SCI patients to gradually practice their respiratory function and improve voice quality. We hypothesized that OMREX and VIT could enhance respiratory function and improve voice quality and could be explored as a practical and effective non-invasive therapeutic method for patients with respiratory dysfunction after SCI.
Subjects and Methods
This study was approved by the Ethics Committee of the China Rehabilitation Research Center (approval No. 2019-78-1) on May 27, 2019 (Additional file 1), and informed consent (Additional file 2) was obtained from the participants before commencing the study. The study was registered with the Chinese Clinical Trial Registry (registration number:ChiCTR1900026922) on October 26, 2019.
Subjects
Thirty-one participants were recruited from the China Rehabilitation Research Center, Beijing, China. The inclusion criteria were as follows: 1) hospitalized patients diagnosed with a B or C level of injury according to the American Spinal Injury Association (ASIA) classification (National Spinal Cord Injury Statistical Center, 2017) with an SCI duration of at least 3 months (inclusive); 2) aged 18 to 70 years; 3) Chinese Mandarin speaking; 4) able to sit for more than 30 minutes without postural hypotension; 5) receiving regular routine therapy; 6) no prior professional musical experience; and 7)patients and their families provided written informed consent participate in this study. The exclusion criteria were as follows:1) a history of speech disorder, psychiatric disorder, neurologic impairment, or respiratory disease prior to injury; 2) severe cognitive dysfunction or a Mini-mental State Examination (Clini et al., 2018) score < 17 (illiteracy) or < 20 (primary school);and 3) epilepsy, malignant arrhythmia, or other serious physical diseases. The criteria for withdrawal and termination of the study were as follows: patients could terminate the study if their condition changed, if they were discharged from the hospital, or if they voluntarily withdrew from the study. A total of 18 participants completed the experiment. Thirteen participants were excluded from the study because they did not meet the inclusion criteria (n= 12) or for other reasons (n= 1). The sample size was calculated according to the formulan=Z2·σ2/d2, whereNis the minimum sample size;Zis the con fidence interval, which is generally 90%;σis the standard deviation; andDis the sampling error range, which is normally 0.5. The minimum sample size was calculated asn= 17.99;thus, the sample size was approximately 18. The participants’characteristics are shown inTable 1.
Research design
The study was a randomized controlled trial with a pretestmidtest-posttest design including two groups: the intervention group (n= 9) and the control group (n= 9). Participants were randomly assigned to one of the two groups, including a music therapy group that performed OMREX and VIT and a control group that performed respiratory training. This study was initiated in June 2019 in the Scienti fic Research Foundation of the China Rehabilitation Research Center.
Procedure
After obtaining approval from the Scientific Research Foundation of the China Rehabilitation Research Center,participants were first screened by SCI specialists. Patients diagnosed with ASIA classi fication B and C conditions who had respiratory dysfunction were referred to the Music Therapy Department. Participants were reviewed by the researchers to identify potential interventional objectives based on the inclusion and exclusion criteria of the study. Once potential participants were identified, an invitation to the study was sent to the potential participants or to the family members of participants who were not able to make decisions themselves with an explanation of the study, including the purpose,procedures, risks, bene fits, con fidentiality, and subjects’ rights.Once consent forms were acquired, the participants were divided into two groups based on their ASIA classification.Music therapy researchers screened patients based on previous tracheotomy outcomes to determine whether the patients had abnormal articulation or impaired laryngeal function. After screening, computer-generated sequences(Excel 2013, Microsoft Office software, Seattle, WA, USA)were used to randomly assign patients to the two groups using a completely randomized design. The participants in the intervention group were trained by music therapists for 12 weeks to perform OMREX + VIT, while participants in the control group were trained in respiratory exercises for 12 weeks. The enrollment and allocation of participants are shown inFigure 1.
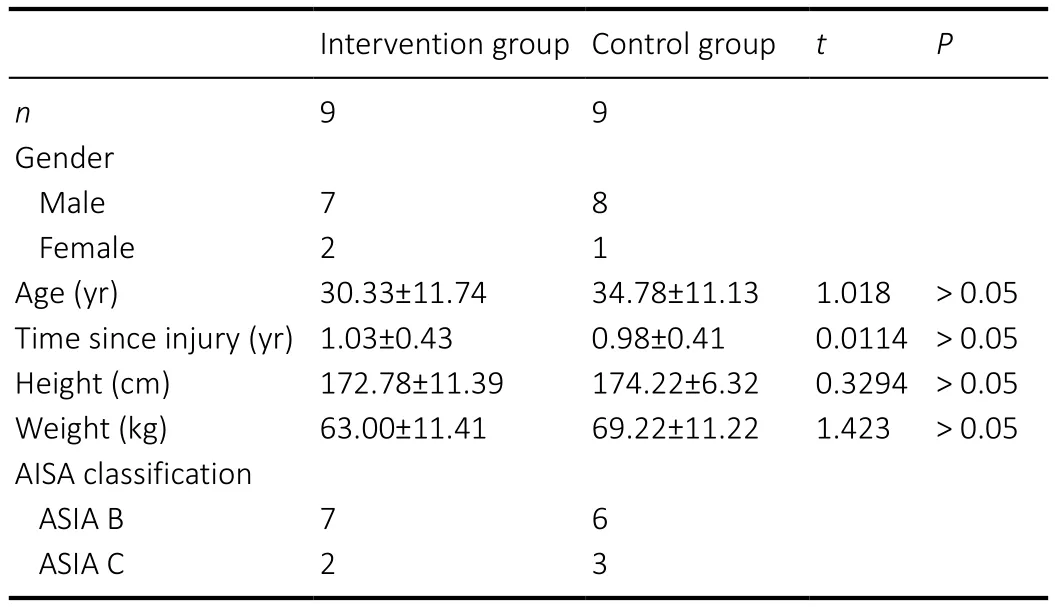
Table 1 |Characteristics of study participants
Interventions
Once the participants for each group were identified,an intervention delivery schedule was developed. The intervention group was trained in OMREX to improve respiratory volume and was trained in VIT to improve vocal quality by music therapists. Each patient was trained by a music therapist for 30 minutes per session, five sessions a week, for 12 weeks. In the first 10 minutes, the music therapist helped participants to practice inhalation and exhalation on one long single note (Additional Figure 1bars 1-8) and staccato singing in short melodic intervals as preparation for the session (Additional Figure 1bars 9-12). In the next 15 minutes, the patient performed vowel singing by melody intervals with alternating tonality practice (Additional Figure 1bars 13-16), and then a short melody line consonant with alternating tonality practice was performed (Additional Figure 1bars 17-21). In the last 5 minutes, the patient sang specific Chinese song tracks, such as “Orchid”, “Hawthorn Tree”, or “Country Road”. The control group received routine respiratory function training by a respiratory therapist,including breathing control and pursed-lip breathing (Clini et al., 2018). The therapy sessions of the two groups were both 30 minutes per day, five times a week, for a total of 12 consecutive weeks. All patients underwent routine treatment during the study period. The routine treatment included taking regular medications and other routine care and support.
Measurements
All participants were assessed before recruitment into therapy to obtain baseline values. A mid-term evaluation was conducted after 6 weeks, and the final evaluation was performed after 12 weeks. The test sessions consisted of(1) respiratory function tests, (2) vocal assessment, and (3)questionnaires. No participant wore abdominal binders or other aids likely to affect lung function during assessment or training.
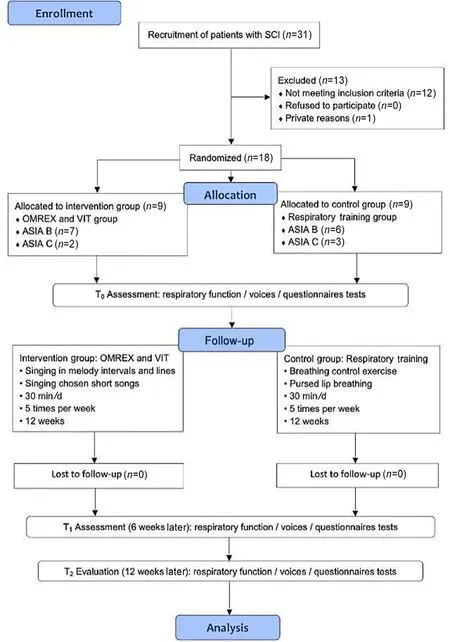
Figure 1 | Flow diagram, consort flowchart for participant recruitment and allocation.
Respiratory function tests
Respiratory function tests were conducted according to the guidelines of the American Thoracic Society (National Spinal Cord Injury Statistical Center, 2017; Clini et al., 2018)and were modi fied to incorporate the limitations associated with SCI (Ashba et al., 1993; Kelley et al., 2003; Lemos et al.,2019). Respiratory function tests were performed using an Anhui Anke FGC-A+lung function measurement instrument(Anhui Anke Biotechnology Group Co., Ltd., Anqing, Anhui Province, China). Lung function was measured in liters or as a percentage of the predicted value [e.g., VC, total lung capacity, inspiratory capacity (IC), residual capacity,forced expiratory volume in 1 second (FEV1), forced VC(FVC), maximal mid-expiratory flow rate (MMF), and FEV1/FVC] (Black and Hyatt, 1971). Ventilatory and upper airway functions were assessed by maximal inspiratory and expiratory flow volume loops using a spirometer (Anhui Anke Biotechnology Group Co., Ltd.). Data were collected using a portable Micro RPM respiratory pressure meter(Compumedics Sleep Pty. Ltd., Abbotsford, Australia) in accordance with the American Thoracic Society/European Respiratory Society guidelines (National Spinal Cord Injury Statistical Center, 2017; Clini et al., 2018).
Vocal quality assessment
Sound pressure analysis was performed by participants wearing headphones (Sony MDR-1A, 3-100,000 Hz, Sony,New York, NY, USA). Sound was recorded for a combination of vocal exercises, familiar song singing, and standardized paragraph reading. After recording the above content in a quiet soundproofed room, the sound pressure level (SPL) was analyzed with an MCS Real-Time Spectrum Analyzer 2.1.6(Gewerbegebiet Aaronia, Germany). The audio recordings from the vocal assessment were used to measure the SPL, including the sing-loud SPL, speak-loud SPL, and sustained note length.Voice quality was assessed both subjectively by the perceptual voice pro file (Cohen et al., 2009) and objectively by computer analysis (Multidimensional Voice Pro file, La Trobe University,Melbourne, Australia) (Oates and Russell, 1997).
Questionnaires
Questionnaires (Swigris et al., 2018; Chua et al., 2019) and a musical background questionnaire — Seashore Measures of Musical Talent (Colman, 2008) (Additional file 3) — were used in this study. The Seashore Measures of Musical Talent questionnaire was not included in the evaluation indications.Participants were interviewed before and after music interventions, which provided a measure of long-term effects on pleasure and arousal in patients.
Among the assessments, respiratory function tests and vocal assessments were performed by the same experienced operator. The St. George’s Respiratory Questionnaire (SGRQ)and quality of life (QoL) questionnaire were evaluated by professionals. All evaluators were registered research assistants who worked as health care professionals and had 5 years of clinical experience. Participants were interviewed by professional evaluators before and after the interventions to ensure consistency and standardization of the training.
Statistical analysis
Data were collected from the two groups at three time points as follows: before the intervention (t0, baseline), 6 weeks later(t1), and 12 weeks later (t2). Using the mean of each group and the standard deviation of the normal distribution, two-way analysis of variance analysis was used to analyze inter-group differences, time effects, and inter-group time interaction differences. The data from the 18 patients with respiratory disorders who completed this study were analyzed with SPSS 22.0 (IBM, Armonk, NY, USA). All data from the intervention and control groups were collected before (t0), during (t1), and after the intervention (t2). Prior to analysis, basic frequencies were analyzed in the data to screen for missing values and outliers and to establish data entry accuracy. Data were analyzed using a repeated-measures analysis of variance to determine the speci fic effects of the interventions.
Results
Effect of OMREX and VIT on respiratory function in SCI patients
Respiratory function was measured in both groups before the first session, during the middle of the sessions, and after the last session. Two-way analysis of variance was used to analyze the results of the intervention group and the control group att0,t1, andt2. Compared with the control group, the IC (t2= 1.93± 0.57 L,F= 5.565,P= 0.0224), FEV1 (t2= 0.92 ± 0.06 L,F=9.988,P= 0.0027), FVC (t2= 2.32 ± 0.81 L,F= 8.813,P= 0.0047),and MMF (t2= 2.59 ± 0.27 L/s,F= 4.951,P= 0.0111) were increased, and the FEV1/FVC (t2= 39.66 ± 8.51%,F= 15.96,P= 0.0002) was decreased in the intervention group att2. A significant increase was observed in the intervention group for FEV1 fromt0tot1(t1= 0.83 ± 0.08 L,F= 18.61,P= 0.0001).Figure 2shows a comparison of the results of the two groups.
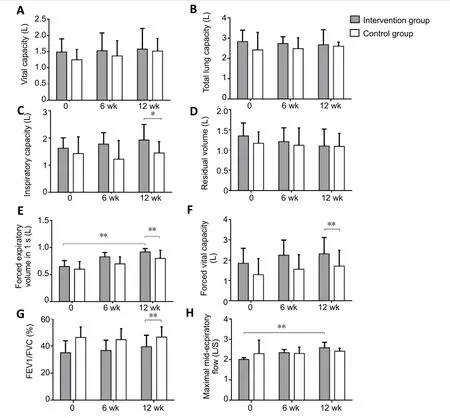
Figure 2|Comparison of respiratory function in spinal cord injury patients undergoing oral motor respiratory exercise and vocal intonation therapy or respiratory training.
Effect of OMREX and VIT on vocal quality assessment in SCI patients
Compared with the control group, the sing-loud SPL (t2= 17.6± 2.1 dBA,F= 7.828,P= 0.0011) and sustained note length (t2= 19.5 ± 4.9 seconds,F= 11.88,P= 0.0012) were increased in the intervention group att2. A significant difference was observed in the intervention group for the sing-loud SPL fromt0tot1(t1= 14.2 ± 1.7 dBA,F= 6.837,P= 0.0024). No difference was observed for the SPL and speak-loud SPL between the two groups.Figure 3shows a comparison of the results of the two groups.
Effect of OMREX and VIT on questionnaire assessment results in SCI patients
A main effect of time was found for the SGRQ and QoL. The SGRQ (t2= 50.91 ± 11.26,F= 6.345,P= 0.0170) and QoL (t2=71.43 ± 13.53,F= 4.734,P= 0.0371) values in the intervention group were significantly lower than those in control group att2.Figure 4shows a comparison of the results of the two groups.
Discussion
In this study, VIT and OMREX were used to train patients with respiratory dysfunction caused by SCI. Compared with the previously reported method that only used singing, the speci fic training method in this study was more targeted and trainable. Initially, 31 patients were enrolled in this study, and 13 patients were excluded because they did not meet the inclusion criteria or for other reasons. Therefore, 18 patients completed the study.
Respiratory function
Respiratory training is a common training method to treat respiratory dysfunction in patients with SCI. However, because of the limitations of the methods and the use of a single training model, the training is difficult for patients to maintain(Tamplin et al., 2011, 2013). Vocal respiratory training involves the use of breath training and vocal training, which combines the action of the diaphragm, chest cavity, pharynx, and other organs to improve respiratory function and vocal quality. Vocal respiratory training can be divided into two specific training techniques — OMREX and VIT. Single-note singing is the first step of OMREX. When patients sang a single note, they were accompanied by harmonic piano playing. A music therapist also played a piano to aid patients during breath training(Thaut and Hoemberg, 2014). Patients in the intervention group were guided to inhale and exhale during note singing(Additional Figure 1bars 1-8). During the second step, music therapists instructed patients to sing “staccato” notes through short rhythmic patterns — an action that requires quick and intense contractions of the diaphragm. Using this training,a rhythmic pattern, which is produced by the alternation of inhalation and exhalation, can be embedded within the short melody (Additional Figure 1bars 9-12). After completing the respiratory and “staccato” singing training, vocal intonation was practiced using a long melody. Patients were guided by piano playing to sing vowels in the same long melodies with different tonality. Quick deep inhalation and exhalation combined with vocal singing, OMREX, and VIT can be used to integrate breathing physiology into the training of sound lines,which improves vocal quality as well as breathing function.
At 6 weeks after OMREX and VIT singing training, the IC, FEV1,FVC, FEV1/FVC, and MMF of the intervention group showed obvious improvements, but the difference was not signi ficant.However, after 12 weeks, a significant improvement was observed in the music training group compared with the control group. This finding suggests that specific targeted music training, for instance, OMREX and VIT combined with therapeutic singing in this study, is effective in treating respiratory dysfunction in SCI patients during long-term training. Time accumulation and training methods are both key factors. Among the measurements of respiratory function, the IC and FVC of the intervention group were enhanced after 12 weeks, which indicated that inspiratory practice before singing a long melody by performing a rapid deep inhalation exercise is bene ficial to improve respiratory volume. When comparing FEV1 and MMF, the intervention group showed an obvious difference from the control group after 12 weeks. This finding suggested that through singing long notes, staccato notes,and melodies in different tonalities, patients who performed music singing training could adjust their respiratory flow more normally during inhalation and exhalation. Therefore, the FEV1, FEV1/FVC, and MMF values of the intervention group showed more effective improvement than those in the control group. Furthermore, the FEV1 also showed an improvement in the intervention group from the beginning to the endpoint of the study. This result indicates that singing practice is an effective method to preserve the FEV1 and that singing long melodies helps to retain greater inspiratory volume. In the final evaluation, no obvious change was observed in VC, total lung capacity, or residual volume, indicating that no difference was found between the music training group and the normal respiratory training group. Patients who underwent regular respiratory training also showed enhanced VC, total lung capacity, and residual capacity measurement scores, which was beneficial for respiratory function. The melodies of“Orchid”, “Hawthorn Tree”, and “Country Road” are all within one octave, making them relatively easy to sing. Practicing any of these three songs after VIT and OMREX can consolidate the effect of respiratory training and improve the respiration and voice quality of participants. The speeds of “Orchid” and“Hawthorn Tree” are moderate, while the speed of “Country Road“ is faster than the other two songs. Patients in the intervention group could breathe more quickly and deeply.

Figure 3| Comparison of vocal quality in spinal cord injury patients undergoing oral motor respiratory exercise and vocal intonation therapy or respiratory training.
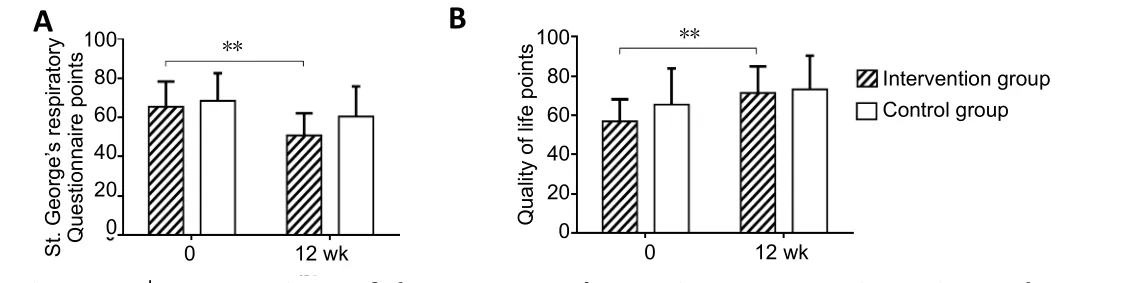
Figure 4 | Comparison of the St. George’s Respiratory Questionnaire and quality of life results in spinal cord injury patients undergoing oral motor respiratory exercise and vocal intonation therapy or respiratory training.
In OMREX training, inhalation is based on abdominal breathing with the assistance of chest breathing, causing the diaphragm to move up and down quickly to increase its strength. When patients with SCI sing the staccato note “wu”, they need to use the abdominal breathing method to inhale quickly and sing. The staccato vocal exercise causes the intercostal muscles, external intercostal muscles, and diaphragm muscles to move quickly, thus supporting breathing while singing short notes. This technique is very similar to pursed-lip breathing in respiratory therapy but requires breathing with more emphasis on sound quality. The syllable “wu” is a lip-down closed accent that saves VC to generate longer sustained vocalization. Singing the tone of “l(fā)a” requires more breathing support because the open mouth accent requires more breath in a short period of time than the lip-down closed accent “wu”; thus, more breath control is needed to maintain the long note. Therefore, the intervention group performed significantly better than the control group in the practice of long tones. These changes facilitated training using the short melody singing exercise. VIT can significantly enhance the experience by providing preparatory time cues, enhancing vocal and pitch support, creating relaxation and tension cues,supporting dynamic changes, and motivating SCI patients to engage in vocal exercises. During VIT, good breath control is necessary for every aspect of vocal output. Therefore, in this study, the music therapist chose “wu” or “me” as the lipdown syllable to practice a closed accent and “l(fā)a” as the open accent to practice vocal quality. The singing of a short melody from three melodic intervals and five scale degrees helped SCI patients in the intervention group to better practice vocal quality, especially in the middle voice area.
Vocal quality and its relevance to respiratory function
In the voice quality assessment, the patients in the intervention group exhibited more improvement than those in the control group at 6 and 12 weeks. The sustained note length was longer than that of the respiratory training group.In the speak-loud SPL test, patients who sang melodic lines had significantly better training effects after 12 weeks than patients with normal breathing training. Thus, it is suggested that vocal singing training had a greater effect than normal respiratory training, and a clear advantage was observed in improving sustained note singing quality. In the intervention group, some patients could stably sing the long vowel note “wu” or other closed accent notes after 20 training sessions, which resulted in a great improvement in sustained note length measures. Regarding relevant respiratory measurements, significant differences in FEV1, MMF, and FEV1/FVC were observed. Therefore, it can be inferred that training by singing long notes with vowels has a speci fic effect on the control of respiratory velocity (FEV1 and MMF). There was no obvious difference in patient gender. In addition, the mean SPL of the intervention group was higher than that of the control group. Patients with quadriplegia may benefit from OMREX and VIT. If their disabilities do not interfere with OMREX and VIT, many of these patients could learn to practice interval singing under guidance, which may be more bene ficial than traditional respiratory training.
Quality of life
The SGRQ score can indirectly reflect patients’ respiratory function status. In this study, the total SGRQ scores of the intervention and control groups were negatively correlated;therefore, a lower score indicated better respiratory function.The symptom and disease effects measured by the SGRQ scores were lower in the intervention group than in the control group, suggesting that singing has a positive effect on improving respiratory symptoms and reducing disease effects in patients with SCI. The activity ability score on the SGRQ was higher in the intervention group than in the control group, suggesting that singing improved the motivation of SCI patients to participate in activities, and this score was positively correlated with the increase in QoL score.
After the intervention, the SGRQ scores and overall QoL scores in both groups were improved, indicating that both music therapy and respiratory training had a positive impact on the QoL of patients with SCI. Among them, the psychological, social, and spiritual dimensions of the QoL assessment of the intervention group were significantly improved after performing singing activities compared with the control group, while the scores of the physiological and functional dimensions of the control group were all improved compared with the intervention group. This result suggests that participating in music activities can produce a more positive emotional experience and a more integrating social experience. The training method based on music and singing involves greater participation for patients with SCI.Additionally, singing is easier and more interesting for patients than regular respiratory training.
The scores of the two groups in different dimensions showed that both respiratory training and music therapy can improve the patient’s respiratory score and QoL score. Respiratory training has a positive effect on improving the physiological symptoms and functional scores, while music therapy has a more obvious advantage for the psychological, emotional experience, and social experience scores.
Limitations
One limitation of this study was the small sample, as previously detailed. Thirteen participants were excluded from the study, which may have caused variance in group allocation. Addition of a blank control group to observe selfhealing could have improved the accuracy of the comparison.Furthermore, this study only recruited 18 patients. If larger studies are conducted in the future, the therapeutic outcomes could be more precisely observed.
Implications for clinical practice
In regular respiratory training, breathing is not easy to observe because there is no sound or visual perception. In vocal training-based music therapy, the sound quality can not only provide a direct behavioral measure, the therapy is also interesting and easy to maintain. In long-term rehabilitation,music therapy can be used by health care professionals for respiratory training after SCI, which is a practical clinical application of music medicine. Additionally, music therapists need to recognize their practice as playing an active role in this therapy. Through training of medical staff in music therapy, music therapists provide professional guidance to improve the clinical effectiveness of the implementation of music medicine for many patients. Based on the results of the current study, it is possible to promote active singing groups on an individual basis and improve the function, participation,and self-worth of SCI patients during long-term rehabilitation.In addition, music therapists may be encouraged and trained by professionals and family caregivers to use active singing to improve the life satisfaction of patients.
Conclusions
OMREX- and VIT-based music therapy is beneficial for improving respiratory dysfunction and sound quality in SCI patients. These exercises are easy for the patients to participate in and adhere to, cause no trauma, and should be promoted in clinical practice.
Acknowledgments:This research was supported by the China Rehabilitation Research Center (CRRC). We thank our colleagues from Music Therapy Center, Department of Psychology, CRRC; Chinese Institute of Rehabilitation Science; Center of Neural Injury and Repair;Department of Spinal and Neural Functional Reconstruction and Beijing Key Laboratory of Neural Injury and Rehabilitation, CRRC; who provided technical support, modi fication advice, and statistical recommendations.It is greatly assisted to the research. We also thank Hong-Wei Liu (from Capital Medical University, China) for patient recruitment, and thank Liang-Jie Du and Ming-Liang Yang (both from Capital Medical University,China) for project application.
Author contributions:Study design and manuscript writing: XYZ;statistical description: CBL; allocation and statistical analysis: CQ; patient recruitment: HWL; music therapy: YCS; project application: LJD, MLY,SHL; study guidance: JJL. All authors approved the final version of the manuscript.
Con flicts of interest:We declare that there are no con flicts of interest in this work. No financial or associative interest that represents a con flict of interest in connection with the work submitted.
Financial support:This work was supported by Scienti fic Research Foundation of China Rehabilitation Research Center, No. 2019zx-23 (to SHL) and Beijing Municipal Natural Science Foundation of China, No.7192238. The funding sources had no role in study conception and design,data analysis or interpretation, paper writing or deciding to submit this paper for publication.
Institutional review board statement:This study was approved by the Ethics Committee of the China Rehabilitation Research Center (approval No. 2019-78-1) on May 27, 2019 and was registered with the Chinese Clinical Trial Registry (registration number: ChiCTR1900026922) on October 26, 2019.
Declaration of patient consent:The authors certify that they have obtained the consent forms from patients. In the form, patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published.
Reporting statement:The writing and editing of the article were performed in accordance with the CONsolidated Standards Of Reporting Trials (CONSORT) Statement.
Biostatistics statement:The statistical methods of this study were reviewed by the epidemiologist of Capital Medical University, China.
Copyright license agreement:The Copyright License Agreement has been signed by all authors before publication.
Data sharing statement:The individual deidenti fied participant data(including data dictionaries) will be shared; the data in particular will be shared; the additional, related documents will be available (studyprotocol, statistical analysis plan, etc.). The data will become available in the future of 5 years. Research colleagues can access the data through the China Clinical Trials Registry, the Resman clinical trials public administration platform.
Plagiarism check:Checked twice by iThenticate.
Peer review:Externally peer reviewed.
Open access statement:This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-Share Alike 4.0 License, which allows others to remix,tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
Additional files:
Additional file 1:Hospital Ethics Approval (Chinese).
Additional file 2:Informed Consent Form (Chinese).
Additional file 3:Seashore Measures of Musical Talent Tests.
Additional Figure 1:Inhalation and exhalation melodic exercise example.
- 中國神經(jīng)再生研究(英文版)的其它文章
- Gut microbiota: a potential therapeutic target for Parkinson’s disease
- Stem cell heterogeneity and regenerative competence: the enormous potential of rare cells
- Therapeutic potential of neuromodulation for demyelinating diseases
- Glycogen synthase kinase-3β inhibitor SB216763 promotes DNA repair in ischemic retinal neurons
- Brain plasticity after peripheral nerve injury treatment with massage therapy based on resting-state functional magnetic resonance imaging
- Dynamic changes in the systemic immune responses of spinal cord injury model mice

