Weight regain after bariatric surgery: Promoters and potential predictors
Hala Mourad Demerdash
Hala Mourad Demerdash, Department of Clinical Pathology, Alexandria University Hospitals,Alexandria 21311, Egypt
Abstract Obesity is globally viewed as chronic relapsing disease. Bariatric surgery offers the most efficient and durable weight loss approach. However, weight regain after surgery is a distressing issue as obesity can revert. Surgical procedures were originally designed to reduce food intake and catalyze weight loss, provided that its role is marginalized in long-term weight maintenance. Consequently, it is essential to establish a scientifically standardized applicable definitions for weight regain, which necessitates enhanced comprehension of the clinical situation, as well as have realistic expectations concerning weight loss. Moreover, several factors are proposed to influence weight regain as psychological, behavioral factors, hormonal, metabolic, anatomical lapses, as well as genetic predisposition.Recently, there is a growing evidence of utilization of scoring system to anticipate excess body weight loss, along with characterizing certain biomarkers that identify subjects at risk of suboptimal weight loss after surgery. Furthermore,personalized counseling is warranted to help select bariatric procedure, reinforce self-monitoring skills, motivate patient, encourage mindful eating practices, to avoid recidivism.
Key Words: Weight regain; Bariatric surgery; Hormones; Diet; Exercise; Genetic factors
INTRODUCTION
Morbid obesity is the consequence of cumulative imbalances between energy intake and energy expenditure[1]. It is a serious chronic disease causing various comorbidities reducing affected persons’ well-being and lifespan. Bariatric surgery is an option in morbidly obese subjects when lifestyle and non-surgical strategies evidenced incompetent. It produces superior reduction in body weight along with relief of associated comorbidities compared to nonsurgical interventions[2]. There are several reputable techniques adopted in management of morbid obesity worldwide.However, Laparoscopic Roux-en-Y gastric bypass (LRYGB) and laparoscopic sleeve gastrectomy (LSG) are two most common weight loss procedures due to their significant weight reduction and durability[3,4].
Following bariatric surgery, body contouring occurs when operated subject finally achieves the required body mass index (BMI) in a comprehensive and stable basis,exhibiting proper nutritional, psychological and clinical aspects[5]. Since during weight loss, those subjects may encounter nutritional depletion along with metabolic adaptation, which compromises healing demands and the whole response to surgical stress[6,7]. Consequently, expected weight loss after successful surgical procedure progresses through several anticipated phases[3] (Table 1). However, stability phase outcome is frequently humbled in considerable number of patients, with regain of 5-10 kg, after weight stabilization which is expected and considered normal[4]. Though, in long-term surveillance, there is growing perception concerning the possibility of weight regain after bariatric surgery[6]. Kraschnewskiet al[8] stated that less than 20%of operated subjects who achieved expected weight loss through various surgical procedures within the first year, experienced variable extent of weight regain within five years.
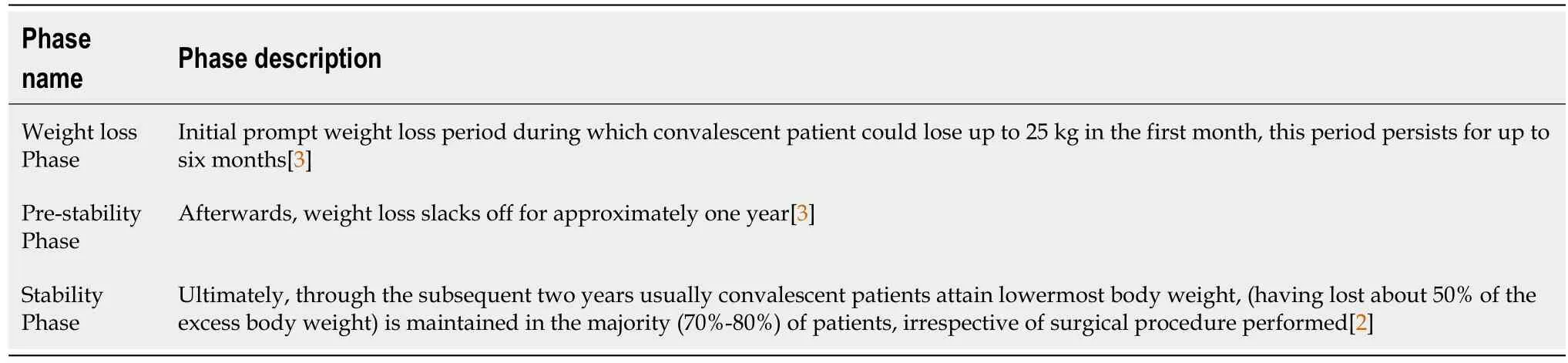
Table 1 Phases of weight changes after bariatric surgery
IDENTIFICATION OF POSTOPERATIVE WEIGHT REGAIN
In order to determine weight regain, it is essential to comprehend the definition of weight stability. Considering that it is expected to observe minor fluctuations in body weight. Rubin defined weight stability as less than 2.5 kg variation in body weight per month over the preceding three months[9]. Given that this issue is subjective; Various literatures proposed a postoperative period of 12-18 mo till body weight becomes stable, with no more fluctuations through the succeeding 4-6 mo[10-12]. Accordingly,definition for weight regain requires careful description by determining patient characteristics, such as baseline BMI, age, gender, surgical procedure, general health perceptions, preoperative comorbidities[13].
Voorwindeet al[14] introduced six definitions for weight regain after bariatric surgery based on reports of various researches: (1) An increase of more than 10 kg from body weight denoting weight regain after achieving desired weight stability; (2)An increase of more than 25% excess weight loss (% EWL) after achieving weight stability phase; (3) An increase in BMI of 5 kg/m2after attaining steady BMI; (4)Weight regain to a BMI more than 35 kg/m2from baseline after long standing follow upe.g.,five years; (5) Any weight regain; and (6) An increase more than 15% of total body weight from baseline after long period follow upe.g.,five years[14]. This is determined by using following equation (total body weight at end of follow up period– total body weight at baseline/ total body weight at baseline × 100 > 15[13,15].
Percentage of EWL refers to reduction in body weight after bariatric surgery. In brief, a subject whose ideal body weight ought to be 70 kg but weighs 130 kg before bariatric procedure, implies 60 kg excess body weight. Appropriately, an optimum weight loss response is generally termed as 50% EWL[10,16]. Then long term postoperative expected weight loss is approximately two-thirds (2/3) of initial body weight (60 kg excess weight) or 40 kg[17]. The ideal weight is customarily determined on the basis of body mass index of 25 kg/m2[13]. This is obtained from a formula where the square of subject’s height in meters is multiplied by 25. For instance, ifsubject’s height is 1.8 m: (1.8 × 1.8) × 25 then ideal body weight is 81 kg[13].
In pursuit for clinically applicable outcome indicators, some authors referred to percentage of total weight loss (%TWL) as the most accurate metric for calculating weight loss post-operative[10,12]. They claimed that %TWL is minimally affected by perplexing preoperative variables as initial BMI, age, comorbidities particularly diabetes. Therefore, %TWL is simple, easy to estimate and understand[12,18]. It is often utilized in appraising behavioral and pharmacotherapeutic literature[18].
%TWL is determine by formula: (Pre-operative body weight – Current body weight)/ (Pre-operative body weight) × 100[12].
Some authors recommend that %TWL applied routinely to quantify weight loss and suggest that ≥ 20%TWL within 12 mo become the established benchmark to identify good responders to weight loss surgery along with reporting of remission or improvement of obesity comorbidities. As well as to track long-term weight regain after bariatric surgery[18,19]. However, Corcelleset al[20] concluded that use of single variable such as %TWL to delineate weight-loss outcomes can generate deceptive evaluation of patients results. Consequently, they recommended use of more than one definition for weight loss including change in BMI or BMI loss percent EWL, percent%TWL, percent excess BMI loss, and percent total BMI loss[20].
Weight changes in two most common bariatric procedures: LRYGB vs LSG
In terms of short-term outcome; RYGB yields 60%- 80% of excess body weight loss(EBWL) within the first year. It is generally recommended for morbid obesity with BMI over 40[18,19]. On the other hand, LSG yields weight loss at a slower, steadier rate, about 60% of excess body weight is lost within first 18 mo[21,22]. However,several studies revealed that both procedures are equally effective measures for shortterm obesity management (< 36 mo) in super obese subjects[23,24].
Pertaining to long-term outcomes; five years postoperative follow up significant weight regain is sporadic for patients undergoing RYGB 2.5%, whereas patients undergoing LSG 14.6%[11]. This conclusion was supported by other studies[25,26]. It is worth mentioning that bariatric surgery was originally intended to downsize the stomach in an attempt to reduce food intake and prompt weight loss, but research studies approved that it has a minimal role in long-term weight loss maintenance[15,16,27].
DETERMINANTS OF WEIGHT REGAIN
The etiology of weight regain tends to be multifactorial including behavioral and dietary habits, mental health, anatomical changes, hormonal variations and genetic aspects[27,28]. Certainly, it results from a combination of components, which vary among individuals’ overtime[29]. Moreover, anticipation of weight regain should be mandatory in consultation with all parties; patient, surgeon and nutritionist prior to surgery, as it may influence patient’s ability to avoid weight regain[28]. Madanet al[30] have observed that only 10% of patients could recall being enlightened about the possibility of weight regain after surgery.
Dietary habits and behavioral practices
Negative eating habits and lack of dietary modifications are risks to long-term postoperative failure. Therefore, to obtain maximum benefit from surgery, patients should be encouraged to adhere to appropriate dietary habits[31]. Since, weight regain commonly occur as result of poor assortment of healthy diets rather than excessive intake[29]. Sawamotoet al[32] reported that persistence of poor preoperative eating behavior after surgery was associated with 68.6% failure rate. Also, Felsenreichet al[33] found that unhealthy eating habit correlated with rate of 59% weight regain within 10 years after surgery. Nikiforovaet al[34] obtained similar results, they proposed the explanation for weight regain include; sleeve or pouch dilation according to procedure performed, enhanced ghrelin levels, lifestyle behaviors and lack of follow-up support. Additionally, Mitchellet al[35] found a higher incidence of weight regain among subjects who consumed limited number of meals, less than 5 small frequent meals, and often skipped breakfast. Owing to a false belief that decrease in number of meals aids supplementary weight loss, whereas actually ingestion of numerous small meals per day augments diet-induced thermogenesis and stimulates smaller insulin secretion[32].
Healthy dietary deeds acknowledged among weight loss maintainers[36]:(1) Commitment to daily intake of breakfast as it assists stabilization of blood glucose level[31];(2) Consumption of ample amounts of water, as optimal hydration prevent oxidative stress, while losing more than 2% of body water causes altered body temperature control, increased both physical and mental fatigue[36]; (3) Greater protein intake about 1.0-1.5 g/kg of ideal body weight per day, restriction of sugar less than 5 gm per serving and less than 30% of daily calories fat[30,37]; and (4) Ingestion of nutrients with low glycemic index and high dietary fibers contents such as fruits and vegetables prolong intestinal absorption[31]. Accordingly, Nutritional follow-up monitoring is consistently regarded as a vital element of medical management after bariatric surgery[38].
Mental health and psychiatric disorders
In this respect adverse eating behaviors could be a crucial factor; including emotional binge eating described as episodes of overeating even when not hungry, on exposure to emotional stimuli or stress to extent of causing gastrointestinal discomfort[31].Similarly, Grazing is repetitive unplanned eating of minor quantities of food with loss of control over this feeding, associated with some psychological disturbance[39]. Also,distracted passive eating implies hyperphagia in presence of an element disturbing one’s attention from the quantity of food ingested as chatting with a friend or watching television[27,40]. Moreover, some individuals may display cravings for fats and sweets, described as addictive personality or could be regarded as cortisolmediated response to stress[41]. Sugar craving phenomenon may possibly be induced by central metabolic actions, as serotonin or dopamine imbalance, altered leptin levels[41]. Cognitive behavioral consideration proves more effective in curing maladaptive eating disorders than sole nutritional counselling without managing psychological part[42,43]. Authentically, psychological conditions as grazing could lead to weight regain postoperatively, regardless of surgery type in about 16%-39% of patients postoperatively[44-46]. This considerably high incidence necessitates accurate assessment,close monitoring and attention to guidelines for nutritional management postoperatively recommending eating slowly, chewing food thoroughly, and increasing the frequency of meals[42].
Physical activity and lifestyle
Physical inactivity is considered a valuable component criticized of having a role in weight regain along with as sleep deprivation (sleeping less than the recommended amount) and television watching more than two hours daily, all may be associated with reduced sensitivity to the internal satiety signals[36]. Similarly, Petitet aldeduced that sleep deprivation augments mood changes, upsets glucose metabolism and appetite regulation[47]. They suggested that sleep replenishes glucose stores in neurons while the awake cycle depicts recurrent glycogen breakdown[47].
Corresponding to American College of Sports Medicine proposals for weight loss and prevention of weight regain for adults; entailed performance of 150 min per week of moderate or vigorous physical activity [moderate < 3-6 metabolic equivalents(METs), vigorous > 6 METs][48]. In view that experts assessed exercise performance in MET. Where one MET is expressed as the amount of energy spent to rest quietly, for average adult one calorie per every 2.2 pounds of body weight per hour[49]. This signifies that moderate activity is enough to burn 3 to 6 times as much energy per minute than lying quietly[50]. American Society for Metabolic and Bariatric Surgery encourages the increase in physical activity to a minimum of 30 min per day[48].Notably, within the first year postoperative, physical activity contributes to enhanced oxygen consumption with prompt adaptability in heart rate and improved lipid profile[51]. While, Freireet al[52] depicted that it has a negligible effect on short-term weight loss, but assists long term weight loss maintenance. Some studies reported that subjects engaged in moderate to vigorous physical activity achieved a greater % EBWL compared to others less physically active 2-5 years postoperative[53-55].
Anatomical modifications
RYGB bears a long-term failure rate of 20%-35%, particularly in super-obese population (BMI > 50 kg/m2) due to gastro-gastric fistula or disrupted staple line[56].Gastro-gastric fistula is a communication between pouch and stomach remnant, which permits food to cross duodenum reducing restrictive and malabsorptive potentials of RYGB, but is alleviated by surgical revision as biliopancreatic diversion or duodenal switch[57]. Even though wide gastrojejunostomy or pouch dilatation could be anticipated, if pouch is > 6 cm in length or > 5 cm in width[58,59]. Although, subjects who develop large pouches (> 50 mL) may comprise comparable weight loss to those with normal sized pouches[59]. However, this never omit contribution of large pouch to weight regain[57,58].
Consequently, Dayyehet al[59] found that dilated gastrojejunal stoma after RYGB produces early gastric pouch emptying, they concluded that its’ diameter was correlated with weight regain. While in LSG weight regain may result from physiologic dilation of stomach remnant in the long run, or failure of complete removal of the gastric fundus[60]. This entails reduction in post-prandial satiety,allowing increased volume of food consumed, to the extent that 59% of patients regained more than 20% of their lost body weight[60,61].
Hormonal/metabolic imbalance
Summary of gut hormone changes after surgery: A chief focus after performing bariatric surgery is time interval of satiety hormones signifying early sense of fullness with smaller meals based on their release site[62]. Additionally, there is an overall agreement that great improvement in glycemic control accomplished are likely to be associated with alterations in the secretion of gastrointestinal hormones including hunger (ghrelin), satiety [glucagon-like peptide-1 (GLP-1) and peptide tyrosine tyrosine (PYY)], and energy balance[63].
LSG reduces the size of the stomach; stimulus for gut hormones secretion specifically GLP-1 is obtained by proximal alimentary signals,e.g.,increased cholecystokinin derived by entrance of hydrochloric acid, amino acids, or fatty acids into duodenum[64,65]. These changes influence release of ghrelin, PYY, GLP-1 and glucose-dependent insulinotropic polypeptide (GIP) as well as other gut hormones[65,66]. On the other hand, RYGB approach, eliminates the stomach and proximal small intestine, creating a small pouch and direct connection with distal gut, consequential variations in gut hormones secretion results from abrupt exposure of intestinal epithelium to nutrients, with subsequent stimulation of L- cells[66]. This is coupled with significantly suppressed ghrelin, elevated GLP1, PYY levels, along with high pH of undigested chyme possibly contributing to diminished food intake and altered energy expenditure, leading to weight loss[66,67]. Also, exclusion of the upper segment of the intestine, where the GIP producing K-cells are present, would entail diminished levels of GIP, and is likely to constrain fat accumulation and intuitively supports long-term weight loss maintenance[68].
Hormonal disparity associated with weight regain
GLP-1:Acts to lower blood glucose by stimulating insulin release and inhibiting glucagon secretion[65]. GLP-1 is decomposed by ubiquitous dipeptidyl peptidase-IV(DPP-IV) enzyme[69]. Conversely, DPP-IV expression seems to be mediated by epigenetic influences as hyper- methylation of the DPP-IV promoter due to unhealthy lifestyle or genetic predisposition[69]. Also, deregulation of metalloproteinases coincident with fibrosis in different adipose tissue depots were found to induce insulin resistance in adipocytes and skeletal muscle cells[70]. Specifically, morbidly obese subjects coupled with insulin resistance undergoing bariatric surgery, may confront suboptimal response of GLP-1 associated with possibility of weight regain[71]. Those subjects achieve better response in terms of glycemic control and weight loss upon management with postoperative DPP-IV inhibitors[72].
Ghrelin/leptin ratio:A range of subjects may display a robust neuroendocrinemetabolic starvation feedback to initial weight loss that promotes metabolic energy preservation and favors weight regain after bariatric surgery[73]. Furthermore, Serum leptin is expected to decline by 50% after the first postoperative week, with an additional decrease during the first postoperative year[67]. Consequently, good responders revealed greater ghrelin to leptin ratio during fasting and post-prandial preoperative assessment contrasted with those who encountered weight regain[73].On the other hand, operated patients who gradually regain weight, encountered resistance to the satiety-inducing effects of leptin[74]. The condition is characterized by elevated circulating leptin levels and decreased leptin sensitivity[75].
Growth hormone:Growth hormone (GH) is another sporadic factor principally regulated by two hypothalamic peptide hormones: GH-releasing hormone (GHRH)and somatostatin[76]. Though, further brain signaling pathways are participating in the control of GH secretion. Obese subjects may exhibit multiple endocrine defects that correspond to body composition variations, as increased visceral fat and decreased fatfree mass[77]. Theoretically, combination of various somatotropic axis alterations might be accountable for diverse scores of GH and insulin growth factor-1 (IGF-1)deficiency in obese subjects. Among the underlying neuroendocrine alterations of low plasma GH levels in obesity, associated with GHRH, somatostatin dysregulation[77].Few studied recommended preoperative evaluations of GH/IGF-1[78]. They proposed that prevalence of persisting GH and/or IGF-1 levels below the normal range for six months after surgery was correlated with a significantly insufficient weight loss[77,78]. The GH/IGF-1 axis is assessed by evaluating serum IGF-1 Levels and the GH peak after stimulation by (GHRH + arginine hydrochloride)[78].
Reactive hypoglycemia:Establishes another hypothesis for weight regain as a consequence of dumping syndrome, mediated by hypersecretion of GIP and GLP-1, which may induce B cell expansion and insulin hypersecretion as long term consequences[79,80]. Besides this, Hypoglycemia ensues in 64%-82% of subjects within 5 years postoperative. The assumption for its occurrence involve refined pancreatic B cells function and mass, improved insulin sensitivity, diminished ghrelin level[80,81]. Since glucose is perceived as a chief appetite mediator, several attacks of hypoglycemia due to substantial insulin hypersecretion after meals, may trigger appetite[82]. Relatedly,direct effect of insulin on lipid accumulation since one of major function of insulin is inhibition of lipolysis[81,83]. Hence existing information reveals that attenuated postprandial gut hormone feedback /or reactive hypoglycaemia may show a correlation between eating disorders and hormonal imbalance[75,84].
Female menopause:Female menopause would apparently reduce effectiveness of bariatric-surgery outcome; given that estrogens mediate the effects of reproductive axis function on weight regulation[85]. Asarianet al[86] concluded that surgery seems more effective for pre-menopausal women (or post-menopausal women receiving hormone replacement therapy) than climacteric women with lower levels of estrogen.Because estrogens powerfully regulate the satiating effect of gut hormones as GLP-1[76,85].
Genetic predisposition
Authentically, it is largely proposed that genetic and environmental aspects could modify the outcome of bariatric surgery, especially in the long run[87,88]. Exceedingly high baseline BMI > 50 kg/m2is be associated with concomitant fast postoperative weight loss, besides greater risk of postoperative weight regain[89,90].
Numerous genes were identified as obesity related genes, and mutations of any produces rare monogenic forms predispose to obesity; including leptin gene, leptin receptor, pro-opiomelanocortin (POMC), melanocortin 4 receptor, melanocortin 3 receptor, fat mass and obesity-associated (FTO), insulin induced gene 2, G proteincoupled receptor 24, corticotropin releasing hormone receptor and corticotropin releasing hormone receptor[91]. Remarkably, mutations in the zone of leptin/melanocortin pathway in the central nervous system being essential in regulation of energy homeostasis appears to result in enhanced appetite and reduced satiety, consequently early postoperative failure[89].
Accordingly, generation of genome-wide association studies (GWAS) provides a reasonably rich source of information to illustrate the molecular mechanisms connecting gene regulation, lifestyle and environmental factors in defining the risk of obesity[92,93]. Thus GWAS has improved comprehension of common genetic variants and collectively elucidated approximately 6% of the variation in adult BMI[93,94].Correspondingly, the current hypothesis asserts that patients carrying none or few number of risk alleles of obesity show more efficient weight loss after bariatric surgery than carriers of multiple risk variants[95]. Genetic risk scores is computed by summarizing risk related variants across the genome, through gathering information from various predictive single nucleotide polymorphism (SNP)[91].
Unfortunately, in spite of intensive genetic research, the molecular mechanisms are barely clarified[91,95]. The epigenetic alterations preceding or post-translational regulatory genes without changes in the nucleotide sequence, particularly methylation of DNA cytosine (C) represents an extremely stable modification[96]. Particularly epigenetic markers, in subjects who regained the weight loss induced by nutritional or surgical intervention displayed differential DNA methylation patterns in leukocytes or subcutaneous adipose tissue or compared to subjects successfully maintained their weight loss over a short or long periods[97].
Eventually, the methylation of genes involved in metabolic pathways exhibited changes after bariatric surgery. For example, weight regain is associated with hyper methylation of POMC and in turn, revealed higher melanocyte stimulating hormonepositive neurons[97]. On the other side, low methylation of neuropeptide Y gene is linked to hunger and satiety controlling peptides as ghrelin[98]. Furthermore,distinctive variants of FTO gene interrelate with dietary subscription, as high-protein regime benefits weight loss and improvement of body configuration in carriers of the FTO risk allele rs1558902, while carriers of FTO rs9939609 allele attained better weight loss response to low-fat hypocaloric diet[99].
Another epigenetic element is small non-coding RNAs (21-22 nucleotides), they are crucial for post-transcriptional regulation of gene expression. Single-stranded micro-RNA (miRNA) binds to a complementary target messenger RNA (mRNA) to disrupt translational processes[100]. Some studies reported short- and long-term miRNA profile changes after bariatric surgery in diverse tissues of both animal and humans that were associated with weight regain/or failure to achieve the desired body weight[101,102]. Accordingly, Obesity provoked changes in miRNA concentration within adipose tissues which promotes chemotaxis of macrophages and other immune cells towards the adipocytes. These miRNAs further impose chronic low grade inflammation, which sequentially may alter miRNA profile[103]. For example, miR-365 and miR-574, are proposed in adipose tissue hypertrophy through regulation of Early B cell factor 2 specific brown fat selective role involved in adipocyte differentiationviaregulation of Peroxisome proliferator-activated receptor Gamma PPARγ, a ligandactivated transcription factor, involved in numerous cellular functions as lipid metabolism, glucose homeostasis and impediment of oxidative stress[104]. Therefore,they may represent prospective targets for non-surgical therapy of obesity and postulate novel biomarkers for predicting bariatric surgery outcomes[103].
PREDICTORS OF WEIGHT REGAIN
An essential measure during evaluation of patients with obesity prior to surgery; is identification of attributes or biomarkers that could deduce improvement of the metabolic profile of candidates that benefits from surgery on long term. Also, to categorize subjects more susceptibility to regain weight after surgery[32].
A greater weight reduction during early weight loss phase postoperative
Initial prosperous weight loss within the first few months postoperative anticipated long term weight loss at 4 and 8 years, examining long-term impression of intensive lifestyle intrusion on obesity associated comorbidities and mortality[35,105]. Also,Vogelset al[106] assumed that comparatively high baseline BMI and fat mass were correlated with concomitant long-term weight loss maintenance during two years follow up period (< 10% regain). Alvaradoet al[107] deduced better response upon requesting morbidly obese subjects to lose around 4.5-9 kg of weight, in few weeks instantaneously prior to bariatric surgery, they attained improved postoperative weight loss. Similarly, some studies assessed preoperative weight loss of less than 5%or 5%-10% of total body weight was accompanied with superior outcome[108,109],However, other studies concluded that extremely high baseline BMI above 50 kg/m2was correlated with inferior postoperative weight loss (below 50% EWL)[110,111].
Baseline insulin sensitivity
Insulin regulates numerous metabolic processes within serval organ in body.Consequently, reduced sensitivity to insulin action is termed insulin resistance,i.e.,suboptimal response of various metabolic functions to normal insulin levels in blood[112]. It has a prime influence in predicting vulnerability to weight regain, and may be concluded through insulin resistance as defined by HOMA-IR[113]. Hence high baseline plasma insulin may be indicative of postoperative insulin resistance[112].Similarly, Antuna-Puenteet al[114] proposed that subjects with high plasma triglyceride concentrations were found to be insulin resistant. Konget al[115] recommended applying a combination of biomarkers including elevated baseline fasting plasma insulin and inflammatory biomarkers as IL-6 levels, and the number of HAM56+cells(macrophages) in subcutaneous white adipose tissue (WAT) to anticipate opposition to weight loss as well as susceptibility to weight regain with a prediction accuracy of 75%. Estimation of pancreatic β cell function (insulin secretion) and insulin sensitivity were calculated by using following formulas[116,117]:
(1) HOMA-IR = [Fasting insulin (uU/mL) × Fasting blood glucose (nmol/L)]/22.5.
(2) HOMA-β = [20 × fasting insulin (uU/mL)]/[Fasting blood glucose (mmol/L)-3.5].
(3) Quantitative insulin-sensitivity check index (QUICKI)= 1/[log fasting plasma insulin (uU/mL) + log fasting blood glucose(mg/dL)].
(4) Oral glucose tolerance test (OGTT): Fasting blood samples are drawn, then subject ingest 75 gm glucose load for OGTT. Glucose and insulin are measured in all blood samples obtained, usually at 0, 60, and 120 min or only 0 and 120 min during the OGTT.
(5) Matsuda index = 10000√ (FPI × FPG) × (x GPC × x IPC). Where FPI is fasting plasma insulin expressed as μU/mL, FPG is fasting plasma glucose expressed as mg/dL, x GPC is mean plasma glucose concentration after the load and x IPC is the mean insulin concentration after the load[117].
Expected normal ranges for above parameters: HOMA-IR normal range is less than 1.4, HOMA-β reference value is less than 81.7, while QUICKI index is less than 0.4 and MATSUDA index non diabetic range is less than 4.5[116,117].
Plasma concentrations of total cysteine
Plasma cysteine level is strongly connected with enlarged fat mass, probabilities of developing obesity and could be used as predictor of weight regain[118,119]. Cysteine is an essential sulfur-containing amino acid, that can form disulfide linkages, which simultaneously regulate protein structure and stability[120]. Circulating total cysteine(tCys) exists either as free cysteine homogeneous (cystine) or mixed (e.g.,homocysteine-cysteine) disulfides, and albumin-bound cysteine[121]. While cellular cysteine is the rate limiting precursor of intracellular antioxidant glutathione and prevail principally in reduced form[122]. Since plasma tCys is predominantly oxidized, high levels tCys, presume unfavorable outcomes, and is often related to obesity[120].
In addition, Cysteine enhances the activity of stearoyl-CoA desaturase-1 (SCD-1),which is a key enzyme for synthesis of monounsaturated fatty acids. SCD-1 introduces a single double bond at the Δ9, 10 of long-chain acyl-CoA substrates[123]. Its chief products are palmitoleic acid and oleic acid; the largely copious fatty acids in cholesterol esters, membrane phospholipids and triglycerides[123]. The activity of SCD-1 is also associated with the levels of sulfur containing amino acid, particularly cysteine. So SCD-1 suppression results in diminished fat deposits (regardless of food intake), enhanced insulin sensitivity and greater basal energy expenditure[123,124].Accordingly, high plasma tCys observed to be positively linked to elevated total cholesterol, low density lipoprotein-cholesterol and triglycerides[125]. As it effectively inhibits hormone-sensitive lipase, and promotes adipocyte triglyceride and glucose uptake[125]. Hanvoldet al[126] concluded that profound tCys elevation two years after RYGB was associated with weight regain.
Plasma adipokines
Some adipokines have displayed the ability to influence weight regain owing to their roles in energy expenditure and or food intake as adiponectin, retinol-binding protein 4 (RBP4), angiotensin converting enzyme (ACE) activity[127].
RBP4:RBP4 is transport protein for retinol (Vitamin A) secreted mainly by the liver and to a lesser extent by the adipose tissue. Munkhtulgaet al[128] stated that the minor allele of regulatory RBP4 SNP was found to augment adipocyte RBP4 expression and was correlated with elevated BMI in Asian population. Wanget al[129] reported higher baseline RBP4 associated with compromised weight loss, they elucidated increased release of RBP4 in obese WAT owing to the presence of hypertrophic adipocytes during weight regain. In view that RBP4 carrying retinol is a precursor of ligands of retinoid X receptor, which activates peroxisome proliferator activated receptors modulating transcription of genes involved in fat metabolism and adipogenesis[130].In this respect, elevated RBP4 level reflects stimulated adipocyte proliferation,adipogenesis and accordingly weight regain[131].
Additionally, RBP4 Links to insulin resistance through RBP4 associated effects comprising increased hepatic gluconeogenesis by accentuating the exhibition of phosphoenolpyruvate carboxykinase enzyme in the liver which simultaneously suppresses insulin signaling in skeletal muscle by blocking insulin-stimulated phosphorylation of insulin receptor substrate-1[132]. Moreover, glucose transporter GLUT4 protein level in human adipocytes correlates positively with the rate of glucose clearance and inversely with circulating RBP4 level[133].
ACE:ACE gene polymorphisms are associated with BMI and obesity[134]. Provided that immense amounts angiotensin II (Ang II), product of ACE activates adipocyte differentiation and consequently influence adipose tissue mass[135]. Moreover, Wanget al[136] observed that greater reduction in ACE level was coupled with stable body weight during follow-up and abstained tendency to weight regain. Velkoskaet al[137]demonstrated the effect of ACE inhibitors on body weight management by reducing body water orviareduction in energy intake.
ACE is a carboxypeptidase that is expressed in many tissues including adipose tissue but predominantly in the vascular endothelium, brain and lung. The enzyme is anchored to cell membranes and is shed into the plasma by enzymatic cleavage[138].Furthermore, a positive association between the weight loss induced change in serum ACE concentration and weight regain duringad libitumfeeding (free feeding)[138,139]. A causal association appears between ACE and weight regain. However, the underlying mechanism remains unclear, in spite of the fact that ACE plays a role in many processes other than the regulation of blood pressure, such as inflammation,fibrosis and the regulation of food intake by the hypothalamus by reinforcing thermogenesis (though corticotrophin releasing hormone-autonomous mechanism)[136].
Fibroblast growth factor 21:Fibroblast growth factor 21 (FGF21) is a “myokine.” that stimulates the oxidation of fatty acids, production of ketone bodies, and inhibition of lipogenesis[141]. Kharitonenkovet al[141] proposed that it could be a prospective metabolic regulator and a potential anti-diabetic drug. FGF21 mRNA is expressed in gastrointestinal tract, brain, skeletal muscle, brown adipose tissue, and heart[142].FGF21 is a molecule with a very short half-life of 1-2 h in absence of specific stimuli,due to enzymatic cleavage by fibroblast activation protein α (FAP), a serine protease that inactivates FGF21[143]. Interestingly, FAP is secreted from muscle during physical exercise[144]. Also, FGF21 is removed from circulation by renal clearance[140].
FGF21 acts as a fasting-induced hormone intended for the adaptive response to starvation and consumption of energy derived from tissues breakdown[145]. Several studies hypothesized relationship between energy expenditure, body weight regulation and FGF21[145-147]. Through provoking energy expenditure with acute low-protein diet 3% causes almost an average energy expenditure (adaptive thermogenesis) can identify individuals who are able to disperse the excess calories consumed as heat (“spendthrift”) opposed to those who are incapable (“thrifty”)[145]. The extent of the elevation in serum FGF21 level in condition of acute low-protein overfeeding is positively correlated with the acute change in 24-h energy expenditure. While poor responders (Thrifty) show an attenuated FGF21 response to acute low-protein feeding,therefore are vulnerable to weight gain over 6 mo[145,146]. Provided that individuals don’t suffer liver, cardiac, kidney or muscle disease which may interfere with test results[147].
CONCLUSION
Bariatric surgery is a tool to achieve significant weight loss, to obtain maximum benefit must adapt pre and postoperative follow up. Also, the role of a nutritionist in bariatric surgery team has expanded ahead diet counseling, to address individual barriers and counsel morbidly obese subjects by ensuring they understand selected bariatric procedures, offering education, identify individual factors that may predict weight regain, reinforce self-monitoring skills, encourage mindful eating practices, supply appropriate nutritional supplements, and motivate daily physical activity, provide close support and follow-up to avoid relapse.
 World Journal of Meta-Analysis2021年5期
World Journal of Meta-Analysis2021年5期
- World Journal of Meta-Analysis的其它文章
- Review of the effects of SARS-CoV2 infection and COVID-19 on common pediatric psychiatric illnesses
- Maturation of robotic liver resection during the last decade: A systematic review and meta-analysis
- Current and future of anterior cruciate ligament reconstruction techniques
- COVID-19 and psychiatry training: A cross-national trainee perspective
