Review of the effects of SARS-CoV2 infection and COVID-19 on common pediatric psychiatric illnesses
Kripa Balaram, Masroor Ahmed, Raman Marwaha
Kripa Balaram, Masroor Ahmed, Raman Marwaha, Department of Psychiatry, Case Western Reserve University (MetroHealth), Cleveland, OH 44109, United States
Abstract Severe acute respiratory syndrome coronavirus-2 is a novel coronavirus strain that causes pneumonia and acute respiratory distress syndrome along with other morbidities, collectively known as coronavirus disease 2019 (COVID-19) disease.There has been widespread discussion about the psychological impact of COVID-19 particularly on children and adolescents. There have been overarching negative effects with regards to decreased physical activity, more screen time, increasingly unhealthy diets, and irregularities in sleep/wake schedules. This, coupled with disruptions in ongoing mental health treatment and associated support structures,has caused unprecedented declines in the emotional and psychosocial wellbeing of children and adolescents. This review aims to systematically review the literature to provide a general overview of the ways in which COVID-19 has affected common psychiatric illnesses in children and adolescents. The included articles in all subsections concluded that symptoms of these common childhood psychiatric disorders have generally been exacerbated by the COVID-19 pandemic. This review indicates that quarantine and the consequent isolation have had multiple significant and consistent negative implications on the mental health of children and adolescents. Our study indicates that there should be increased vigilance among providers and families to mitigate the negative psychological effects that the COVID-19 pandemic has on children with common childhood psychiatric disorders.
Key Words: COVID-19; Depression; Anxiety; Attention deficit hyperactivity disorder;Obsessive-compulsive disorder; Tourette's; Children; Adolescents
INTRODUCTION
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV2), is a novel coronavirus strain that causes pneumonia and acute respiratory distress syndrome along with other morbidities, collectively known as coronavirus disease 2019 (COVID-19) disease[1]. The World Health Organization declared SARS-CoV2 infection to be a global pandemic in March 2020. As of February 2021, there are upwards of 110 million cases of SARS-CoV2 infection worldwide with over 28 million cases and 500000 total deaths documented in the United States. In addition to significant medical impact, there has also been a profound psychologic impact because of the pandemic, particularly among vulnerable populations. There has been widespread discussion about the psychological impact of COVID-19 particularly on children and adolescents[2].
Since the start of the pandemic, the transition to online-based education, increasing school closures, and the alteration of normal adolescent social activities have caused an unmitigated disruption in the lives of children[2]. In general, the greatest impacts appear to be losses in areas of daily routine, institutional support structures, and social connection[2]. Though these effects are generally attributed to the cessation of inperson learning in schools, it is generally assumed that there have been overarching detrimental effects with regards to decreased physical activity, more TV and screen time, increasingly unhealthy diets, and irregularities in sleep/wake schedules[2].
This, coupled with disruptions in ongoing mental health treatment and associated support structures, has caused unprecedented declines in the emotional and psychosocial wellbeing of children and adolescents[2].
This review aims to systematically review the literature to provide a general overview of the ways in which COVID-19 has affected common psychiatric illnesses in children and adolescents.
For this review, we performed multiple literature searches of PubMed, Cochrane and PsycInfo to find articles (Figures 1-5). The first search used the keywords "COVID 19," "children," and "OCD," the second search used the keywords "COVID 19,""children," and "ADHD," the third search used the keywords "COVID 19," "children,"and "Tourette’s syndrome,” the fourth search used the keywords "COVID 19,""children," and "depression," and the fifth search used the keywords "COVID 19,""children," and "anxiety.” The search was not initially restricted by study design or language but was limited to articles published between January 1 to December 31,2020. Review articles published in or translated to English were included. Full-text references cited in these articles were also researched for additional relevant studies.The inclusion criteria were on-topic articles discussing the effect of COVID-19 on common pediatric psychiatric disorders. The exclusion criteria were any study designs that were case reports, surveys, or study protocols, or articles that were considered to be off topic.
OBSESSIVE COMPULSIVE DISORDER
A total of 12 articles were identified through a literature search. There were no clinical trials, randomized controlled trials or meta-analysis that were identified. After excluding articles that were off-topic, seven articles remained for inclusion (Figure 1).

Figure 1 PRISMA table for Search 1.
Though the mean age of onset for those with obsessive-compulsive disorder (OCD)is 19.5 years, childhood onset does occur and generally persists throughout adulthood[3]. According to the diagnostic and statistical manual of mental disorders, 5thedition,25% of males have onset of symptoms before age 10. Characterized by obsessions and compulsions, OCD can present with a varying combination of symptoms including intrusive and persistent unwanted thoughts, repetitive checking, fears of contamination, feelings of worry and disgust, and repetitive behaviors or patterns of behaviors that an individual is compelled to perform[4,5]. In general, symptoms of OCD are exacerbated by acute stressors, such as trauma.
Due to the COVID-19 pandemic, children and adolescents who are susceptible to OCD are most likely to be affected[6]. There were several studies that concluded that children and adolescents diagnosed with OCD experienced a considerable worsening of their symptoms[6-10]. One particular study concluded that this significant worsening was most prevalent in those with an earlier age of symptom onset and in those with a family history of attention deficit hyperactivity disorder (ADHD)[7].Another study also identified a substantial increase in contamination fears and cleaning or washing obsessions due to general fears of exposure to infection brought on by the pandemic[8,9]. Contrastingly, there has also been widespread advocacy of infection control measures, such as frequent handwashing, and dissemination of information on avoiding exposure/contamination. These measures may actually lead to those suffering from severe OCD symptoms to feel less stigmatization over their cleansing obsessions[9,10]. They may instead feel more acceptance over their symptoms, as their fears become well-founded and “real” and their ritualized behaviors became generally widespread and even encouraged[9,10]. Therapeutic interventions, such as cognitive behavioral therapy, are designed to achieve symptomatic relief by targeting behaviors like excessive hand washing and intrusive thoughts of contamination. This can lead to a cognitive dissonance in those with OCD as the COVID-19 pandemic has led to a widespread and public campaign to encourage these behaviors.
ADHD
A total of 29 articles were identified through a literature search. There were no clinical trials, randomized controlled trials or meta-analysis that were identified. After excluding articles that were off-topic, four articles remained for inclusion (Figure 2).
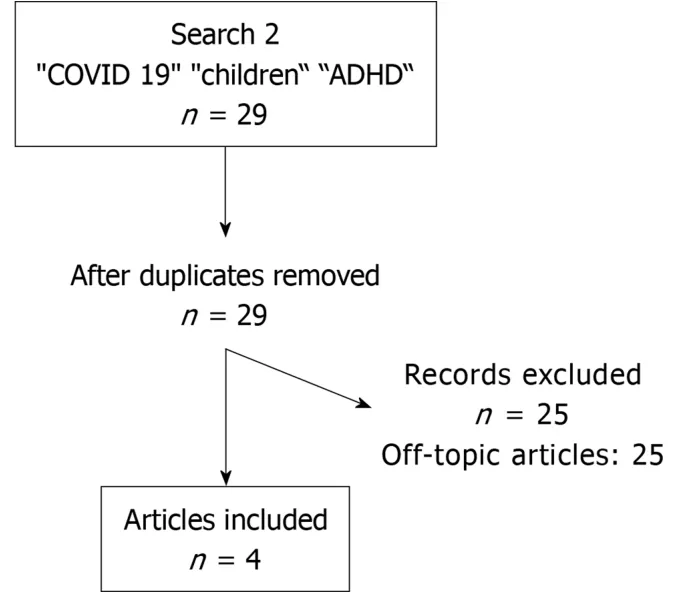
Figure 2 PRISMA table for Search 2.
ADHD, characterized by persistent patterns of inattention and/or hyperactivity/impulsivity that interferes with functioning, is one of the most prevalent psychiatric disorders of childhood[3,11]. In general, children diagnosed with ADHD have been noted to experience an exacerbation of symptoms throughout the COVID-19 pandemic[11-14]. In addition, children with the hyperactive phenotype of ADHD may find the constraints of quarantine and lockdown to be particularly difficult to accommodate[15]. Several studies noted an increase in symptoms such as hyperactivity, irritability, emotional outbursts, and defiant or disruptive behavior[12-14]. There was also a noted increase in problematic behaviors from caregivers, such as irritability or aggressive behavior directed towards the child. These changes were generally attributed to both the nonspecific emotional stress caused by the pandemic and the lack of daily structure and increasingly flexible school/Learning schedules[13].
TOURETTE’S DISORDER
A total of five articles were identified through a literature search. There were no clinical trials, randomized controlled trials or meta-analysis that were identified. After excluding articles that were off-topic, three articles remained for inclusion (Figure 3).
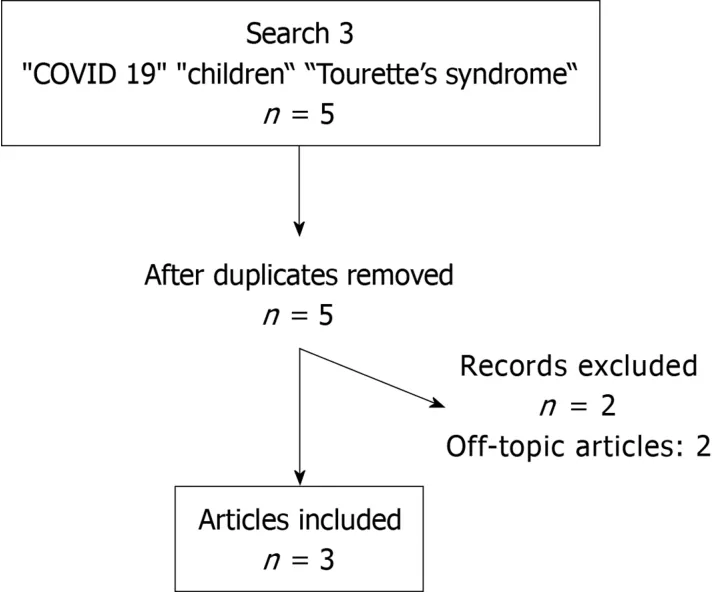
Figure 3 PRISMA table for Search 3.
Public health measures aimed at controlling the spread of the COVID-19 pandemic have led to some changes in the symptomatic presentation of Tourette’s disorder[15-17]. The advent of online learning and social distancing measures have decreased the social burden of tics, and resulting psychological distress, felt by children in school and other learning environments[16]. In contrast, several other non-obscene socially inappropriate tics - such as spitting, coughing, sneezing, or inability to maintain interpersonal distance with touching – have become more socially unacceptable[15].This can lead to increased anxiety and distress in children with these symptoms who may feel undue pressure to modify or control these behaviors[15]. This increased anxiety can lead to a secondary increase in tic symptoms[15]. In general, children with Tourette’s disorder were observed to have overall clinical decline with either a worsening of existing symptoms or a resurgence of previously-controlled symptoms[15-17].
DEPRESSION AND ANXIETY
A total of 378 articles were identified through a literature search by using the keywords “COVID,” “depression,” and “children.” There were two clinical trials, two meta-analysis, and eleven systematic reviews. There were no randomized controlled trials that were identified. The clinical trials were excluded as they were off topic. The systematic reviews were excluded due to the overlap from within the meta-analyses.After excluding articles that were off-topic, two meta-analyses remained for inclusion(Figure 4).
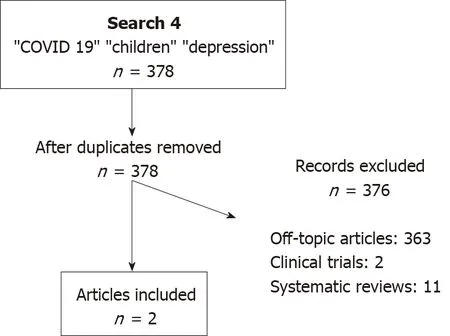
Figure 4 PRISMA table for Search 4.
A total of 533 articles were identified through a literature search by using the keywords “COVID,” “anxiety,” and “children.” There were three clinical trials, four meta-analysis, two randomized controlled trials, and thirteen systematic reviews. The clinical trials were excluded as they were off topic. The randomized controlled trials were excluded as they were not pertinent to the population subgroup of our review and dealt with the ailments in the adult population. The systematic reviews were excluded due to the overlap from within the meta-analyses. After excluding articles that were off-topic, one meta-analysis remained for inclusion (Figure 5).
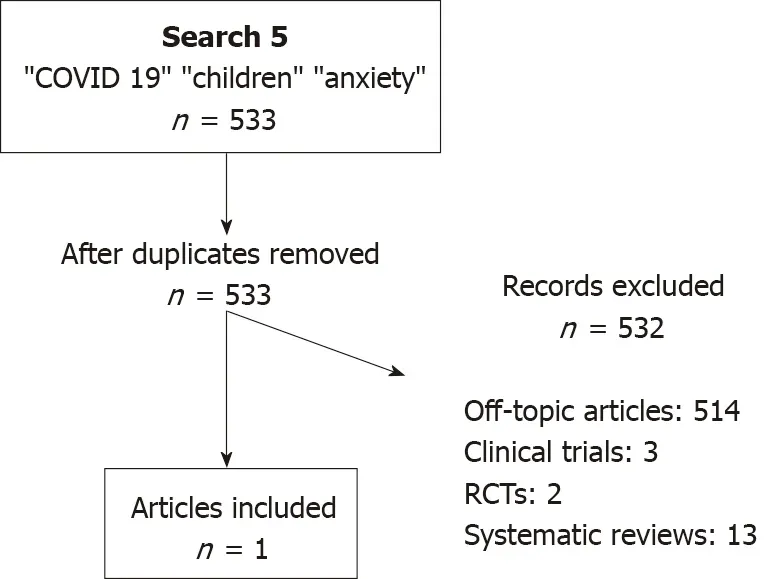
Figure 5 PRISMA table for Search 5.
Both anxiety and depression are major ailments amongst the youth that are often under-reported and under-recognized. Data by SAMHSA, or the Substance Abuse and Mental Health Services Administration, shows that the overall prevalence of depression for adolescents aged 12 to 18 is 13.1% as opposed to 7.1% for adults.Similarly, the rates are 31.9% and 19.1% when it comes to anxiety amongst adolescents,and adults respectively. This means that the relative prevalence of these disorders already remains higher amongst the adolescents as compared to adults.
COVID-19 and its consequent effects have further negatively impacted the mental health of children and adolescents. Multiple studies have shown that social isolation and the resultant loneliness were associated with increased risk of both depression and anxiety[18-25]. Anxiety was seen to be more prevalent amongst children maintaining quarantine, and this was thought to be likely mostly due to loss of primary caregiver’s job, financial instability leading to a dearth in provision of basic amenities[22]. It was also noted that the time period of isolation was more important for symptomatology of mental health ailments than the severity of isolation[23].
The studies noted certain interesting factors. There was seen to be a mild difference between the sexes as well, with loneliness being more strongly associated with social anxiety in boys and depression in girls[23]. Certain primary school students who viewed COVID-19 as a serious disease had increased anxiety and somatic symptoms[2]. One study mentioned that children who practiced social distancing for fear of getting infected were predisposed to anxiety disorders. The same study also mentioned that children who engaged in social distancing secondary to peer pressure had a higher likelihood of depression[24]. This illustrates a thought-provoking difference in symptoms based upon the motivator for social distancing in the first place. Interestingly an age-related difference was also discernible in certain study populations. High school children reported higher number and severity of symptoms of anxiety and depression as compared to their primary and middle school counterparts[24,25]. Certain salient causes of increased depression levels in the study population were also noticed such as internet/smartphone addiction and affected friends/family members in the past.
On the contrary a few of the factors protective towards depression were lesser time spent on the internet, adequate coping mechanisms, increased exercise time, and having a sibling[19,20]. It should come as no surprise that the pandemic meant more children/adolescents, and adults alike ended up spending increased time on the internet and lesser time outdoors. Similarly, children and adolescents with worry and fear about COVID-19 had higher rates of depression, whereas remaining optimistic amidst these times had the opposite effect[2].
CONCLUSION
The included articles in all subsections concluded that symptoms of these common childhood psychiatric disorders have generally been exacerbated by the COVID-19 pandemic. This was primarily attributed to the restricting quarantining regulations and the public fear of SARS-CoV2 infection. For instance, the routine learning schedule implemented at public schools that had helped to provide structure to children with ADHD have been lost while quarantining at home. This in turn led to worsening ADHD symptoms and behaviors. The public fear of COVID-19 and the widespread encouragement of frequent handwashing have both exacerbated contamination fears in those with OCD experience and worsened repetitive sanitizing behaviors. While children with Tourette’s Disorder may have experienced less psychosocial distress over their tics by being away from school, they may still face difficulties with controlling symptoms because of increased anxiety over their tic behaviors breaking social-distancing rules.
This review portends that quarantine and the consequent isolation have had multiple significant and consistent negative implications on the mental health of children and adolescents. The stigmata of these consequences can be detected even months later beyond quarantine[25]. In general, a lack of vigilance and treatment for pandemic-associated effects on childhood psychiatric disorders may propagate significantly negative and refractory long-term sequelae into adulthood. Our study indicates that there should be increased vigilance among clinicians and families to mitigate the negative psychological effects that the COVID-19 pandemic has on children with common childhood psychiatric disorders. This calls for pediatricians,psychiatrists, and all healthcare providers alike to remain cognizant of these effects and work collaboratively towards measures to reduce the psychological impact of this already menacing physical ailment.
 World Journal of Meta-Analysis2021年5期
World Journal of Meta-Analysis2021年5期
- World Journal of Meta-Analysis的其它文章
- Maturation of robotic liver resection during the last decade: A systematic review and meta-analysis
- Weight regain after bariatric surgery: Promoters and potential predictors
- Current and future of anterior cruciate ligament reconstruction techniques
- COVID-19 and psychiatry training: A cross-national trainee perspective
