Application of "dredging meridians and dispersing lung exercises" based on meridian theory of traditional Chinese medicine in patients with stable chronic obstructive pulmonary disease
Pei-Xia Zhou,Xiao-Ye Ma,Fang-Hui Xu,Fei-Fan Xu,Kun Wang,Hai-Bo Hu,Xue-Chao Lu,Li Wang*
1Qingdao Hospital of Traditional Chinese Medicine, PCCM (Pulmonary Medicine) Center,Qingdao 266033, China. 2Department of Nursing, Qingdao Hospital of Traditional Chinese Medicine,Qingdao 266033,China.
Abstract
Keywords: chronic obstructive pulmonary disease at stable stage; Tongjing xuanfei exercise; pulmonary rehabilitation; pulmonary function
Background
Chronic obstructive pulmonary disease (COPD) is a common and frequently occurring respiratory system disease. The prevalence of COPD in China among people over 40 years old accounts for 13.7%,and the incidence of COPD tends to be in younger patients impacting social, health, and economy [1]. There is no radical cure for COPD.The key is to prevent an acute attack, protect, and improve pulmonary function. Stable stage COPD rehabilitation therapy is of great significance in preventing acute exacerbation of COPD, delaying decline of pulmonary function, improving quality of life, and improving prognosis. Studies have shown that appropriate rehabilitation treatment COPD stable stage promotes the improvement of disease‐related symptoms and pulmonary function [2, 3].Traditional Chinese medicine (TCM) has played an important role in the prevention and treatment of COPD. Many appropriate techniques of TCM have been widely used in stable stage COPD, and they are especially effective in pulmonary rehabilitation, prevention and treatment of stable stage COPD, such as “treating winter diseases in summer,” and “Sanfu (the dog days) patch”. Based on the Theory of Meridians and Collaterals from theInternal Classic, the study group creatively proposed the treatment of COPD via Tongjing Xuanfei exercises, which has been applied in clinical research.
Data and methods
Ethical approval
All the participants signed informed consent form. The study was approved by the hospital's ethics committee (2019HC12LS060) and signed informed consent was provided by patients or their families.
General data
A total of 130 patients with stable stage COPD who were hospitalized at the Department of Pulmonary Diseases of Hiser Medical Center of Qingdao from September 2018 to September 2020 were selected as the study objects. The block randomization method developed the random assignment scheme. Random numbers were used for block randomization according to the random number table, and the random enrollment assignment scheme table was formulated. Patients were equally divided into the observation group, and the control group. Clinicians grouped the patients randomly as per the randomization scheme, and according to the order in which the patient was enrolled. The differences were not statistically significant(P>0.05) after two groups were compared, see Table 1.
Diagnostic criteria
The 2019 Global Initiative for the Diagnosis, Treatment and Prevention of Chronic Obstructive Pulmonary Disease (GOLD Guideline 2019 Edition) [4] was the reference for the diagnosis and staging of COPD.
Inclusion and exclusion criteria
Inclusion criteria (1) Patients who met the diagnostic criteria for COPD in Western medicine; (2)Patients with mild to moderate disease condition at a stable stage; (3) Between 40 and 65 years of age; (4)Patients with normal thinking ability, and verbal and written communication skills; (5) Patients who signed the informed consent form.
Exclusion criteria (1) Patients who did not meet the above diagnostic criteria or inclusion criteria; (2) Critical stage disease patients who were at a, or who were accompanied by pulmonary heart disease, or respiratory failure; (3) Patients with other respiratory diseases such as bronchial asthma, bronchiectasis, cystic pulmonary fibrosis,tuberculosis, and lung cancer; (4) Patients with major disease in the heart, brain, kidneys, digestive system or other systems; (5) Patients with mental retardation or psychiatric disorders who cannot cooperate with the investigation; (6) Patients who could not comply with the study protocol.
Withdrawal and drop-out criteria Patients who did not meet the requirements and were found after enrollment. Patients who met the inclusion criteria but did not complete all of the trial due to various reasons and those with incomplete observation data were deemed as drop‐out cases.
Intervention method Control group patients received routine pulmonary rehabilitation care given by department nurses including daily care during hospitalization and discharge education. The content of discharge education included post‐discharge rehabilitation training,respiratory training, diet, exercises, medication, reexamination, etc.,where the details included: (1) Exercise training: approximately 10 minutes once daily in the morning and evening. (2) Respiratory exercises: approximately 20 minutes of diaphragmatic and pursed‐lip breathing once daily in the morning and evening. (3) Oxygen therapy:1–2 L/min with oxygen inhalation time > 15 h/d via nasal catheter for oxygen inhalation. Observation group (1) Patients were taught Tongjing Xuanfei exercises in addition to the routine pulmonary rehabilitation care, practicing once daily in the morning and evening.See Table 2 for the details of the exercises. (2) To help patients learn and master the exercises, CDs for practicing Tongjing Xuanfei exercises were made and distributed to the discharged patients. (3)Follow‐up plan: two home visits within 90 days after discharge, which were usually performed once within one week after discharge, and once between 10 and 12 weeks after discharge. Telephone follow‐ups were performed once every two weeks.
Observation indicators
(1) Using German MasterscreenPFT Jaeger pulmonary function instrument, the pulmonary function of the two groups of patients were measured. Forced expiratory volume in 1 second (FEV1), forced vital capacity (FVC), forced expiratory volume in 1 second as a percentage of the predicted value (FEV1%pred), and the ratio value in 1 second after inhalation of bronchodilator (FEV1/FVC) were measured.
(2) The 6‐min walking distance was tested for the two groups of patients under medical staff supervision, and the maximum walking distance within 6 min was recorded to evaluate the exercise capacity of patients.
(3) The common symptoms such as cough, expectoration, chest tightness, shortness of breath, asthenia, and cyanosis were scored with reference to theGuidelines for Clinical Research of New Chinese Medicines (Trial), with 0–3 points for each item and 0–21 points in total. The higher the cumulative score, the worse the symptoms.
(4) The scores of patients in the two groups were recorded according to the scoring requirements of“CAT Scale,”and COPD mMRC dyspnea index score.
The above indicators were observed and recorded once in Month 0 and Month 12 after treatment, respectively.
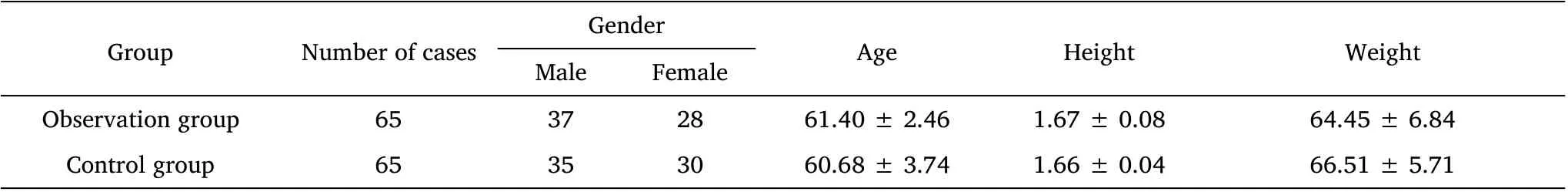
Table 1 Comparison of general baseline data of the two groups of patients

Table 2 Specific steps of Tongjing Xuanfei exercises
Efficacy criteria
With reference to theGuidelines for Clinical Research of New Chinese Medicines (Trial),it is proposed that: (1) Significantly improved: the cumulative score decreased by ≥70%; (2) Partially improved: the cumulative score decreased by ≥30% and <70%; (3) Not improved:the cumulative score did not change, or with a change <30%; (4)Worsened: the cumulative score increased by ≥ 30%. Overall response rate (%) = (Number of significantly improved cases +Number of partially improved cases)/Total number of cases× 100%.
Statistical processing
IBM SPSSstatistics25.0 statistical software was used for processing and analysis. Enumeration data were expressed as frequency, and χ2test was used. Measurement data were expressed as± s. Comparison before and after treatment showed that it was in line with normal distribution and homogeneity of variance. T‐test was used.P<0.05 indicated that the difference was statistically significant.
Results
Pulmonary function and exercise capacity
The comparison of pulmonary function and exercise capacity between the observation group and the control group before treatment showed that the differences were not statistically significant (P>0.05). FEV1,FVC, FEV1%pred, FEV1/FVC, and 6‐min walking distance of the patients in the observation group and the control group were significantly increased as compared to before treatment (P<0.05)after treatment. These indicators were significantly higher in the observation group than in the control group (P<0.05). See Table 3.
TCM clinical symptom score, CAT score, and COPD mMRC dyspnea index score
The CAT score before treatment, mMRC dyspnea index score, and TCM clinical symptom score were compared between the two groups.The differences were not statistically significant (P>0.05). The CAT score, mMRC dyspnea index score, and TCM clinical symptom score of the patients in the observation group and the control group were significantly decreased as compared to before treatment (P<0.05)after treatment. These scores were significantly lower in the observation group than in the control group (P<0.05). See Table 4 and Table 5.
Comparison of efficacy
The observation and control group overall response rate was 92.30%78.46%, respectively. The difference between the two groups was statistically significant (P<0.05). See Table 6.
Table 3 Comparison of pulmonary function and exercise capacity between the two groups( ± s), (n =65)
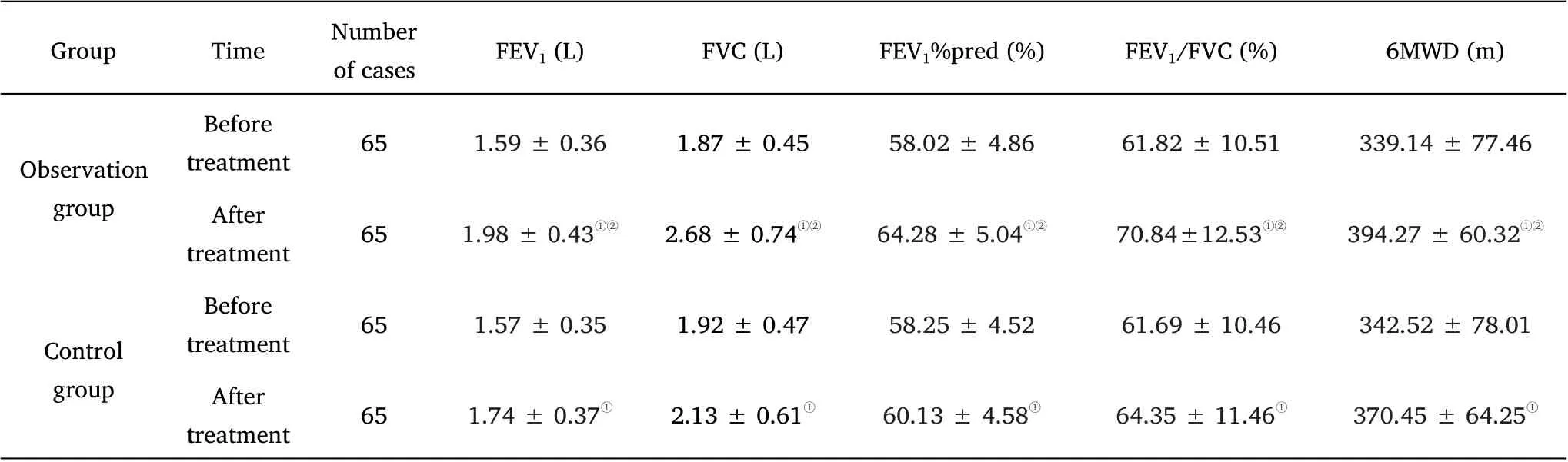
Table 3 Comparison of pulmonary function and exercise capacity between the two groups( ± s), (n =65)
Note:①Compared with the same group before treatment, P <0.05;②Compared with the control group after treatment, P <0.05
GroupTimeNumber of casesFEV1(L)FVC (L)FEV1%pred (%)FEV1/FVC(%)6MWD (m)Observation group Before treatment651.59 ± 0.361.87 ± 0.4558.02± 4.8661.82 ±10.51339.14 ± 77.46 After treatment651.98 ±0.43①②2.68 ± 0.74①②64.28 ± 5.04①②70.84±12.53①②394.27± 60.32①②Control group Before treatment651.57 ± 0.351.92 ± 0.4758.25± 4.5261.69 ±10.46342.52 ± 78.01 After treatment651.74 ± 0.37①2.13 ± 0.61①60.13± 4.58①64.35 ± 11.46①370.45 ± 64.25①
Table 4 Comparison of CAT score, mMRC dyspnea index score,and TCM clinical symptom score between the two groups of patients(±s), (n = 65)

Table 4 Comparison of CAT score, mMRC dyspnea index score,and TCM clinical symptom score between the two groups of patients(±s), (n = 65)
Note:①Compared with the same group before treatment, P <0.05;②Compared with the control group after treatment, P <0.05
GroupTimeNumber of casesCAT scoremMRC scoreTotal score of TCM clinical symptoms Observation group Before treatment6528.67 ± 4.372.83 ± 1.1013.58± 1.24 After treatment6514.26 ± 3.69①②1.39 ± 0.64①②8.01 ± 0.56①②Before treatment6527.69 ± 4.192.78 ± 1.1313.44± 1.24 Control group After treatment6518.73± 4.12①1.97 ± 0.73①11.56 ± 0.29①
Table 5 Comparison of single-item score of TCM clinical symptoms between the two groups of patients (± s), (n = 65)
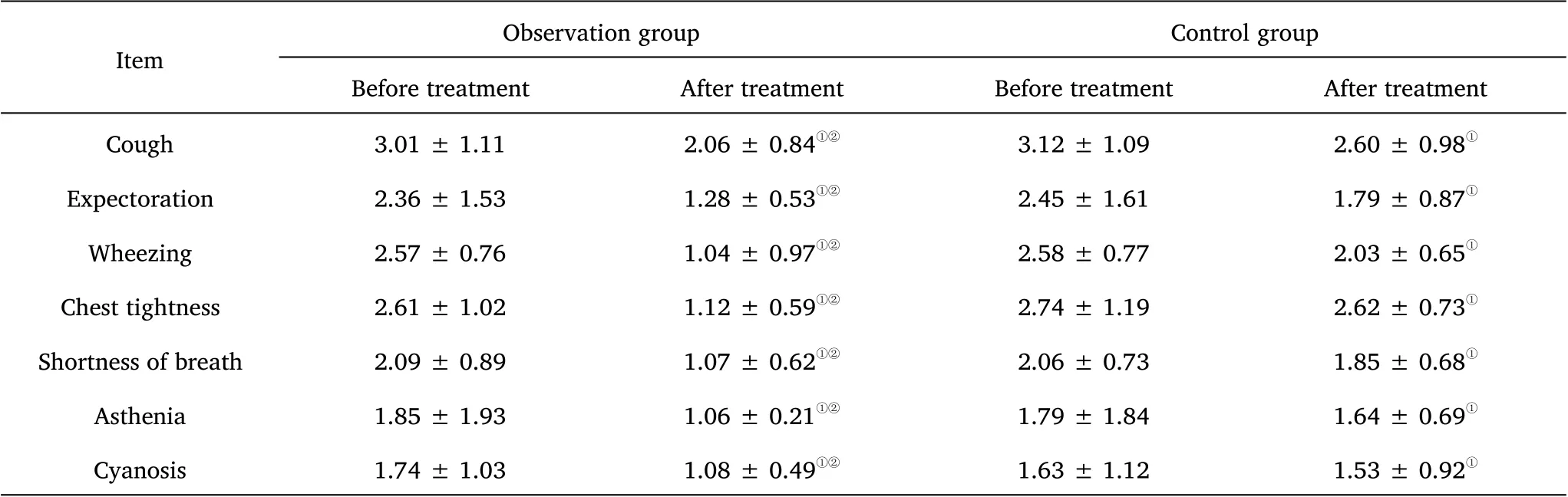
Table 5 Comparison of single-item score of TCM clinical symptoms between the two groups of patients (± s), (n = 65)
Note:①Compared with the same group before treatment, P <0.05;②Compared with the control group after treatment, P <0.05
Observation groupControl group Before treatmentAfter treatmentBefore treatmentAfter treatment Cough3.01 ± 1.112.06 ± 0.84①②3.12 ± 1.092.60 ± 0.98①Expectoration2.36 ± 1.531.28 ± 0.53①②2.45 ± 1.611.79 ± 0.87①Wheezing2.57 ± 0.761.04 ± 0.97①②2.58 ± 0.772.03 ± 0.65①Chest tightness2.61 ± 1.021.12 ± 0.59①②2.74 ± 1.192.62 ± 0.73①Shortness of breath2.09 ± 0.891.07 ± 0.62①②2.06 ± 0.731.85 ± 0.68①Asthenia1.85 ± 1.931.06 ± 0.21①②1.79 ± 1.841.64 ± 0.69①Cyanosis1.74 ± 1.031.08 ± 0.49①②1.63 ± 1.121.53 ± 0.92①Item

Table 6 Comparison of clinical efficacy between the two groups of patients
Discussion
Chronic obstructive pulmonary disease, COPD, is an incompletely reversible and progressive disease with airflow restriction [4]. COPD patients often reduce physical activity due to exertional dyspnea,resulting in decreased physical exercise capacity [5]. It leads to depression, despair, and other negative psychological conditions,resulting in a decline in patients’ quality of life, and reducing the capability of patients to participate in social activities [6, 7]as a result of its long course of disease and repeated hospitalizations. The treatment of COPD is mainly drug therapy in the acute stage. Stable stage treatment is often ignored by clinicians. As a non‐drug means,Pulmonary rehabilitation is of great significance for the treatment of COPD in the stable stage. Pulmonary function decline delay, improve dyspnea, improve quality of life, and reduce the number of acute exacerbations and re‐hospitalizations[8, 9] in patients with COPD can be achieved through effective pulmonary rehabilitation therapy.Stable stage rehabilitation treatment is more significant than that in other stages, and the clinical effect of different rehabilitation treatment measures are different [10, 11]. COPD belongs to the category of “l(fā)ung distension” in TCM. It is mainly characterized by deficiency syndrome of both the lung and the kidney in the stable stage. Qi stagnation will result from the failure of the lung to control qi. Reversed qi flow will result from failure of the kidney to promote respiration. Abnormalities in disseminating vital energy throughout and promoting inspiration by the lung and the kidney, which is manifested as asthma,will cause disorder of ascending and descending functions, resulting in dysfunction of qi. Therefore, it is important treatment to address qi disorder for stable stage COPD patients[12].
The meridians and collaterals are closely connected with the internal organs, limbs and bones, the five sensory organs, the nine body orifices, skin, muscles, tendons, joints and other tissues and organs of the human body is detailed in The Theory of Meridians and Collaterals in theInternal Classic[13].They play a vital role in running qi and blood, regulating qi function, communicating up and down,inside and outside, and regulating the functional activities of the human body [14]. Topical medication of meridians or acupoint therapies [15] have been shown by studies to treat diseases. One of the twelve meridians is the the Lung Meridian of Hand Taiyin,and one of the three yin meridians of the hand. It is interiorly‐exteriorly related to the Large Intestine Meridian of Hand Yangming. The upper part of it is connected to the Liver Meridian of Foot Jueyin in the lung,and the lower part of it is connected to the Large Intestine Meridian of Hand Yangming at the forefinger [16]. Cough, shortness of breath,wheezing, fidgetiness, chest tightness, soreness or coldness at the medial anterior edge of the upper arm and forearm, or pyrexia in the palms are symptoms treated by this meridian and its acupoints related to “the lung”. Meridian patting can stimulate the flow of qi and blood of the meridians, open the channels of the meridians, target both the exterior and interior, and achieve the functions of strengthening vital qi to eliminate pathogenic factors and balance yin and yang. Lung Meridian patting can exert the functions of removing the obstruction in the meridians and collaterals, dispelling cold, and eliminating pathogenic factors, which is helpful to alleviate the symptoms [17,18].
The “Tongjing Xuanfei exercises” are creatively proposed based on the TCM Theory of Meridians and Collaterals. Pushing and kneading massage at the acupoints combined with patting massage along the running direction of the Lung Meridian of Hand Taiyin is adopted to promote the dissemination of lung qi, stimulate the flow of qi and blood in meridians and collaterals, and open the channels of meridians to achieve the functions of dispersing lung qi, stopping cough,dispelling phlegm, and relieving asthma and cough. This is helpful in alleviating symptoms, and more COPD patients can benefit from it.
FEV1, FVC, FEV1%pred, FEV1/FVC, exercise capacity, CAT score,mMRC dyspnea index score, TCM clinical symptom score, and the improvement in quality of life of the patients in the observation group was shown in this study to be significantly better than those in the control group receiving pulmonary rehabilitation care alone. This suggests that the clinical effect of Tongjing Xuanfei exercises in stable stage COPD patients is significant, and such exercises are of great significance to improve pulmonary function, exercise capability, and clinical symptoms.
In conclusion, value of Tongjing Xuanfei exercises in stable stage COPD patients is high. It can effectively improve pulmonary function,clinical symptoms and quality of life of patients, providing new treatment ideas, and basis for the disease course management of COPD patients in the stable stage.
This study also has some limitations. The sample size is relatively small, and the observation indicators are few. Observation time can be extended to evaluate the impact of Tongjing Xuanfei exercises on the number of acute exacerbations and the number of readmissions, so as to further determine its value.
 Nursing Communications2022年13期
Nursing Communications2022年13期
- Nursing Communications的其它文章
- Delphi and Analytic hierarchy process for the construction of a risk assessment index system for post-stroke shoulder-hand syndrome
- A review of obstacles and facilitating factors of implementing Clinical Ladder Programs in nursing
- Spiritual health, empathy ability and their relationships with spiritual care perceptions among nursing students in China:A cross-sectional correlational study
- Qualitative study on influencing factors of refusal of gastric tube placement in stroke patients with dysphagia
- The influence of professional identity and ageism on turnover intention in nursing homes: a cross-sectional study from suzhou, China
- The relationship of family separation and nutrition status among under-five children: a cross-sectional study in Panti Public Health Center, Jember Regency of East Java, Indonesia
