Clinical efficacy of umbilical therapy with herbal cakes of different dosages for damp-heat diarrhea in young children
XU Yinyin (徐蔭蔭), ZHENG Xianhui (鄭賢輝), ZHANG Xiaowen (張孝文), LAN Yu (藍(lán)玉), WANG Jiali (王佳麗),SHEN Jian (沈健)
Shuguang Hospital, Shanghai University of Traditional Chinese Medicine, Shanghai 201203, China
Abstract
Keywords: Point, Shenque (CV8); Administration on Umbilicus; Acupoint Sticking Therapy; External Therapies; Ge Gen Qin Lian Tang; Dampness-heat; Diarrhea; Child
Manifesting as increased bowel movement frequency and mushy or watery excrement[1], infantile diarrhea may happen at any time but is more likely to hit in the summer and autumn. Its main target is kids aged six months to two years. Infantile diarrhea is a major cause of malnutrition, impaired growth, and even death in kids[2]. In China, this disease ranks second among children’s common diseases (respiratory infection ranks first)[3]. As this issue develops under the joint action of multiple mechanisms[4], modern medicine manages it with comprehensive treatments. The guiding principle includes preventing or correcting dehydration,regulating diet patterns, rationalizing medications,preventing complications, and enforcing nursing care[5-6].Kids usually have a pure Yang constitution. Given the specific geographic feature of Shanghai, adjacent to seashores and located in humid subtropical areas, it is easy for kids to contract damp-heat pathogen externally and internally, damaging the spleen and stomach and consequently causing diarrhea. Traditional Chinese medicine (TCM) can improve the symptoms and shorten the disease duration in treating infantile diarrhea.Moreover, it can also ameliorate kids’ constitution and enhance their immunity[7]. Ge Gen Qin Lian Tang originates fromShang Han Lun(Treatise on Cold Damage Diseases) by ZHANG Zhongjing. Although this prescription can effectively treat damp-heat diarrhea in young kids, orally taking it is a big challenge. In this study,we observed the clinical efficacy of umbilical application with herbal cakes made of Ge Gen Qin Lian Tang prescription in treating damp-heat diarrhea in young kids.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Diagnostic criteria in Western medicine
We referred to theZHU Futang Practice of Pediatrics[3]andDiagnosis and Treatment of Childhood Diarrhea Disease[8]to formulate the diagnostic criteria in Western medicine for this study. Watery or liquid stools, mucous stools, or stools with pus and blood; more frequent bowel movements, ≥3 times a day; abdominal bloating,vomiting, poor appetite, or significant bowel sounds;acidosis, electrolyte disorder, and dehydration; the blood routine test discovered abnormal white blood cell (WBC)count and increased lymphocyte count; feces examination may show normal or a small amount of WBCs and fat globules, while stool culture showed negative.
1.1.2 Syndrome differentiation criteria in TCM
The TCM syndrome differentiation criteria were established based on the content about damp-heat diarrhea in thePediatrics of Traditional Chinese Medicine[9]. Primary symptoms: increased bowel movement frequency, 3-5 times a day, or even 10 or more times a day; altered stool form, watery, liquid, or mushy, may contain mucus. Secondary symptoms:abdominal pain, abdominal bloating, nausea, vomiting,loss of appetite, irritation, thirst, short and dark urine,and burning sensation in the anus. Tongue and pulse: a red tongue body with greasy and yellowish coating,slippery and rapid pulse beats. The diagnosis was confirmed when the primary symptoms and two secondary symptoms were met with the tongue and pulse as a reference.
1.2 Inclusion criteria
Conformed to the Western medicine diagnostic criteria and syndrome differentiation criteria for dampheat diarrhea in TCM mentioned above; mild type(neither dehydration nor toxic condition presented);unlimited gender, ages six months to twelve years; the disease started no more than 72 h, and it was the patient’s first visit; the parents or guardians were informed of the content of the trial and voluntarily signed the informed consent.
1.3 Exclusion criteria
Dermatological conditions such as infection, wounds,and bleeding, making it impossible to perform the umbilical application; allergic to the medicines used in this study or had other contraindications; already used similar external or internal medications before the recruitment; poor compliance (inconvenient traffic or not a local dweller); diarrhea caused by cholera,dysentery, malignant tumors, parasitic infections, or other primary digestive diseases; coupled with primary disorders involving liver, kidney, or hemopoietic system;psychiatric disorders.
1.4 Elimination and dropout criteria
Allergic reactions, significant adverse events, or other medical conditions occurred, so the treatment had to terminate; during the trial, the families or guardians gave the kid medications uninvolved in this study, which may affect the evaluation of the study results; failed to receive the treatment or examinations as required,which may affect the effectiveness or safety ratings;those who quitted or were lost to visit despite the reason.
1.5 Statistical methods
We adopted SPSS version 25.0 statistical software to conduct statistical analysis. The measurement data in line with normal distribution and homogeneity of variance were expressed as mean ± standard deviation(±s) and checked by thet-test; those not conforming to normal distribution were expressed as median(minimum, maximum) [M (min, max)] and checked by the non-parametric test. The enumeration data were expressed as frequency, rate, or constituent ratio. The Chi-square test was applied to the between-group comparison of dichotomous variables. The rank-sum test was used to examine the between-group comparison of ordered polytomous variables.P<0.05 indicated statistical significance.
1.6 General data
The Ethics Committee of Shuguang Hospital, Shanghai University of Traditional Chinese Medicine approved this trial (Approval No. 2015-434-62-01). Seventy-two kids with diarrhea of damp-heat pattern were recruited from the Pediatric Outpatient of Shuguang Hospital, Shanghai University of Traditional Chinese Medicine, between January 1, 2017 and December 31, 2019. The kids were divided into a high-dosage group and a low-dosage group using the random number table method, with 36 cases in each group. After unblinding, we found that the two groups each had one dropout case due to poor compliance at the end of the observation. After eliminating the relevant data, 70 cases were finally enrolled for statistical analysis, with 35 cases in each group. There were no significant differences in gender,age, or body mass index (BMI) between the two groups,suggesting the comparability. The details are displayed in Table 1.
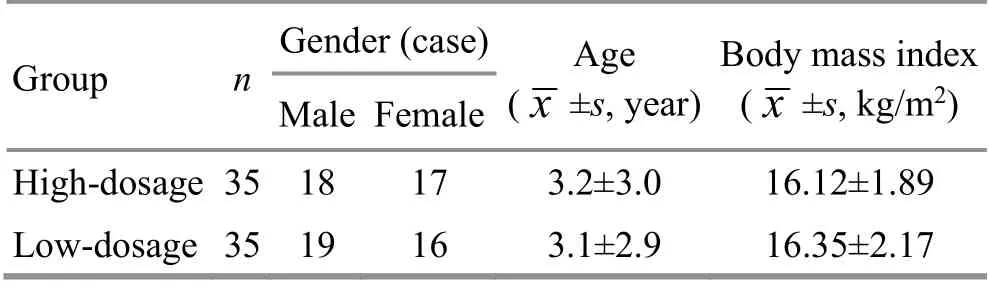
Table 1. Comparison of the general data
2 Treatment Methods
2.1 Primary treatment
Ibuprofen suspension [State Food and Drug Administration (SFDA) Approval No. H19991011, 100 mL(2 g), Shanghai Johnson & Johnson Pharmaceutical Co.,Ltd., China] was offered to those with a temperature over 38.5 ℃ via oral administration (body mass 10-15 kg,4 mL each time; body mass 16-21 kg, 5 mL each time;body mass 22-27 kg, 8 mL each time; body mass 28-32 kg, 10 mL each time) every 4-6 h, no more than 4 times within 24 h. In addition, the kids were asked to take light digestible food in small portions but more times. No other medications were allowed during the observation.
2.2 High-dosage group
Acupoint: Shenque (CV8).
Method: In addition to the primary treatment, the patients were given umbilical application with herbal cakes made of Ge Gen Qin Lian Tang powder [Ge Gen(Radix Puerariae Lobatae),Huang Qin(Radix Scutellariae),Huang Lian(Rhizoma Coptidis), andZhi Gan Cao(Radix et Rhizoma Glycyrrhizae Praeparata cum Melle)] (Tianjiang Pharmaceutical Co., Ltd., China). These Chinese herbal medicines were mixed at 5:3:3:2 and blended with purified water at 3:1 to make cakes of 1 cm in thickness. The age of the kids determined the diameter of the cakes (1 month to 1 year old, 0.5 cm in diameter; 1-2 years old, 1 cm in diameter; 2-3 years old,1.5 cm in diameter; >3 years old, 2 cm in diameter). The herbal cake was placed at Shenque (CV8) and affixed by self-adhesive wound dressings (specification: 5 cm × 7 cm, Taizhou Jingwei Medical Instrument Co., Ltd., China).The treatment was given once a day, 6-8 h each time.
2.3 Low-dosage group
In addition to the primary treatment, the kids were treated with application with low-dosage herbal cakes made of the same prescription at the same proportions at Shenque (CV8). Nevertheless, the Ge Gen Qin Lian Tang powder was mixed with auxiliary materials (corn starch) at 1:9. The size of the cakes and method were also as same as those in the high-dosage group.
The two groups were treated for 3 d and followed up for 7 d.
2.4 Contingency plan for skin allergy
For skin flush, itching, or any other discomfort occurring at the umbilicus, the operator should remove the medicinal application immediately and clean the skin with water. No more treatment is needed if the discomforts are gone in the next 2 h. However, the calamine lotion or erythromycin ointment should be applied externally if the allergy does not get better; the boric acid solution is used for exudation.
3 Therapeutic Efficacy Observation
3.1 Observation items
3.1.1 Clinical efficacy
The efficacy evaluation criteria in this study were made based on theGuiding Principles for Clinical Study of New Chinese Medicines[10].
Markedly effective: The general symptoms were gone within the 72 h of treatment; the stool form and bowel movement frequency became normal.
Effective: The general symptoms improved significantly within the 72 h of treatment; the stool form and bowel movement frequency were also notably ameliorated.
Invalid: The general symptoms showed no improvement or even worsened after the 72 h of treatment; no improvement was found in stool form or bowel movement frequency.
3.1.2 Antidiarrheal rate
The antidiarrheal rate was calculated at treatment days 1, 2, and 3, respectively. Normal stool form for two consecutive times or no desire to defecate and no defecation for 24 h indicated the cease of diarrhea[11].Antidiarrheal rate = The number of antidiarrheal kids ÷The total number of cases in this group × 100%.
3.1.3 Effective rates of TCM symptoms and signs
The TCM symptoms and signs variation evaluation scale was developed according to theTechnique Guidance on the Clinical Trial Design and Evaluation forNew Medications for Common Pediatric Diseases[12]andGuiding Principle of the Clinical Research Technique for New Symptomatic Chinese Medications[13]. The following symptoms and signs were observed. Greasy and yellowish tongue coating, bowel movements ≥3 times a day, watery stools, short and dark urine, red tongue body,vomiting, thirsty, drowsiness, dysphoric heat in the five centers, bowel sounds, poor appetite, and abdominal bloating. The effective rate of TCM symptoms or signs =The improved number of cases after the treatment ÷ The number of cases experiencing the symptom ×100%.
3.1.4 TCM symptoms score
The TCM symptoms scoring scale was made based on theTechnique Guidance on the Clinical Trial Design and Evaluation for New Medications for Common Pediatric Diseases[12]andGuiding Principle of the Clinical Research Technique for New Symptomatic Chinese Medications[13].This scale was used to score the primary and secondary TCM symptoms. The sum of the component scores of these symptoms made the total TCM symptoms score,and the higher the score, the more severe the symptom.The details are shown in Table 2 and Table 3.
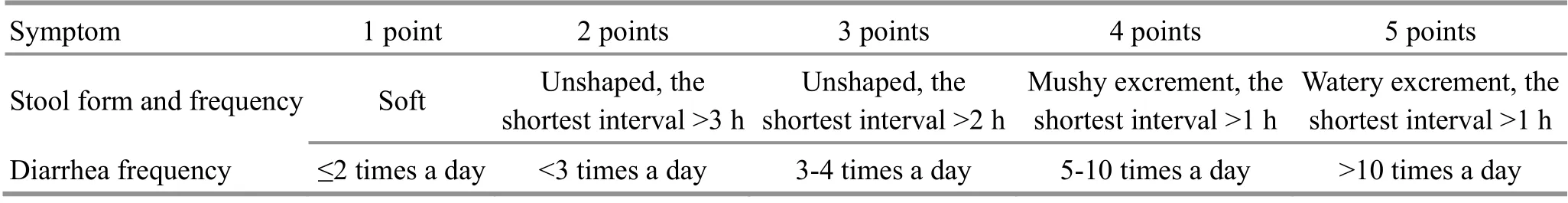
Table 2. Scoring criteria for the primary TCM symptoms
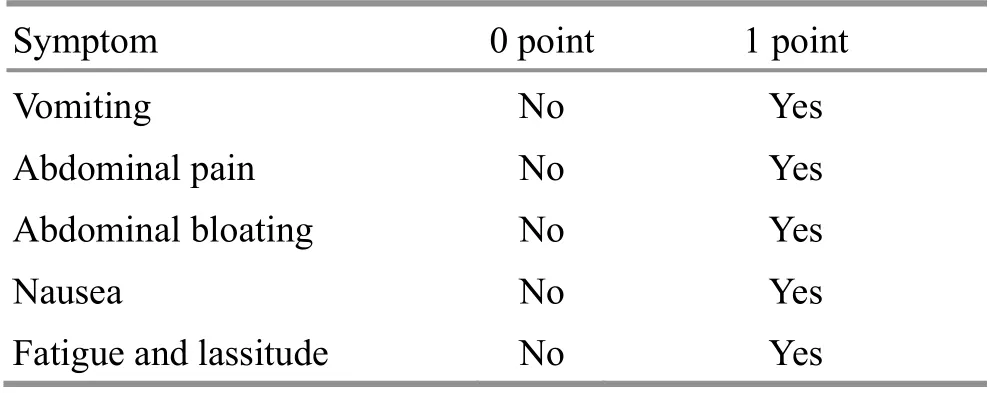
Table 3. Scoring criteria for the secondary TCM symptoms
3.1.5 Safety indicators
The aspartate transaminase (AST), alanine aminotransferase (ALT), blood urea nitrogen (BUN), and creatinine (Cr) levels were determined once before and after the treatment. A level beyond the normal range indicated liver or kidney function impairments, meaning that the medication is unsafe. Otherwise, it is safe to use.
3.2 Results
3.2.1 Comparison of the clinical efficacy
The rank-sum test showed a significant difference in the clinical efficacy ranking between the two groups(Z=-2.574,P=0.01). See Table 4 for the details.
3.2.2 Comparison of the antidiarrheal rate
There were no significant differences in the antidiarrheal rate between the two groups at treatment day 1 and day 2 (P>0.05). However, at treatment day 3, a significant difference was found in the antidiarrheal rate between the two groups (P<0.05). It is suggested that the high-dosage group has a better antidiarrheal effect after the 3-day treatment. See Table 5 for the details.
3.2.3 Comparison of the effective rates of TCM symptoms and signs
Before the treatment, there were no significant differences in the incidence of TCM symptoms or signs between the two groups (P>0.05). After the treatment,significant differences were found in the effective rates of all symptoms and signs between the two groups except thirst, drowsiness, and poor appetite (P<0.01 orP<0.05). See Table 6 for the details.
3.2.4 Comparison of the TCM symptoms score
Before the treatment, there was no significant difference in the TCM symptoms score between the two groups (Z=-0.454,P=0.065). The TCM symptoms scores notably declined after the treatment in both groups(P<0.01), and there was a significant between-group difference (Z=-1.985,P=0.047). See Table 7 for the details.
3.2.5 Comparison of the safety rating
The AST, ALT, BUN, and Cr levels were within the normal ranges before and after the treatment in both groups.
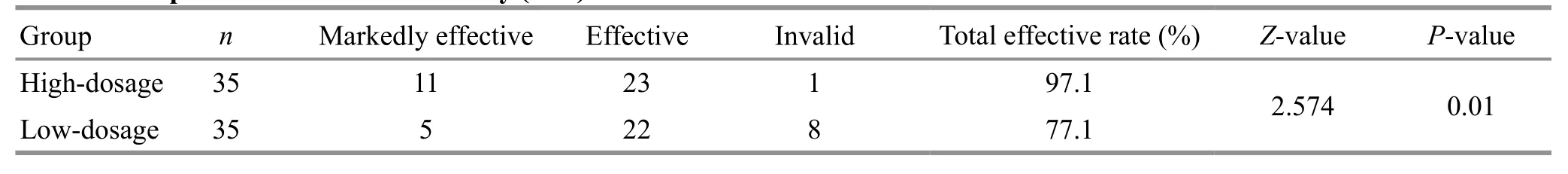
Table 4. Comparison of the clinical efficacy (case)
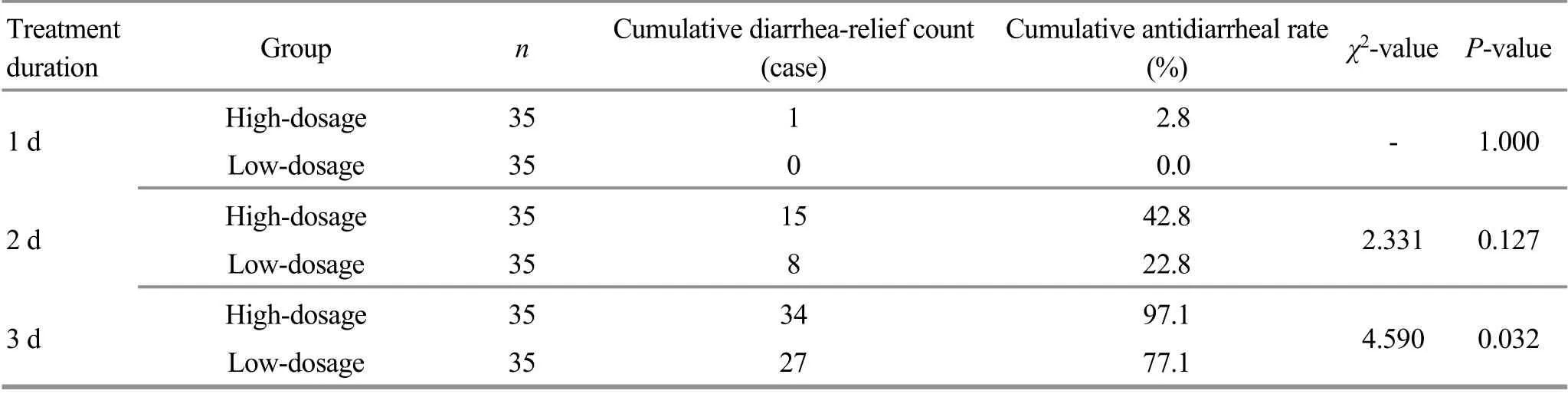
Table 5. Comparison of the antidiarrheal rate
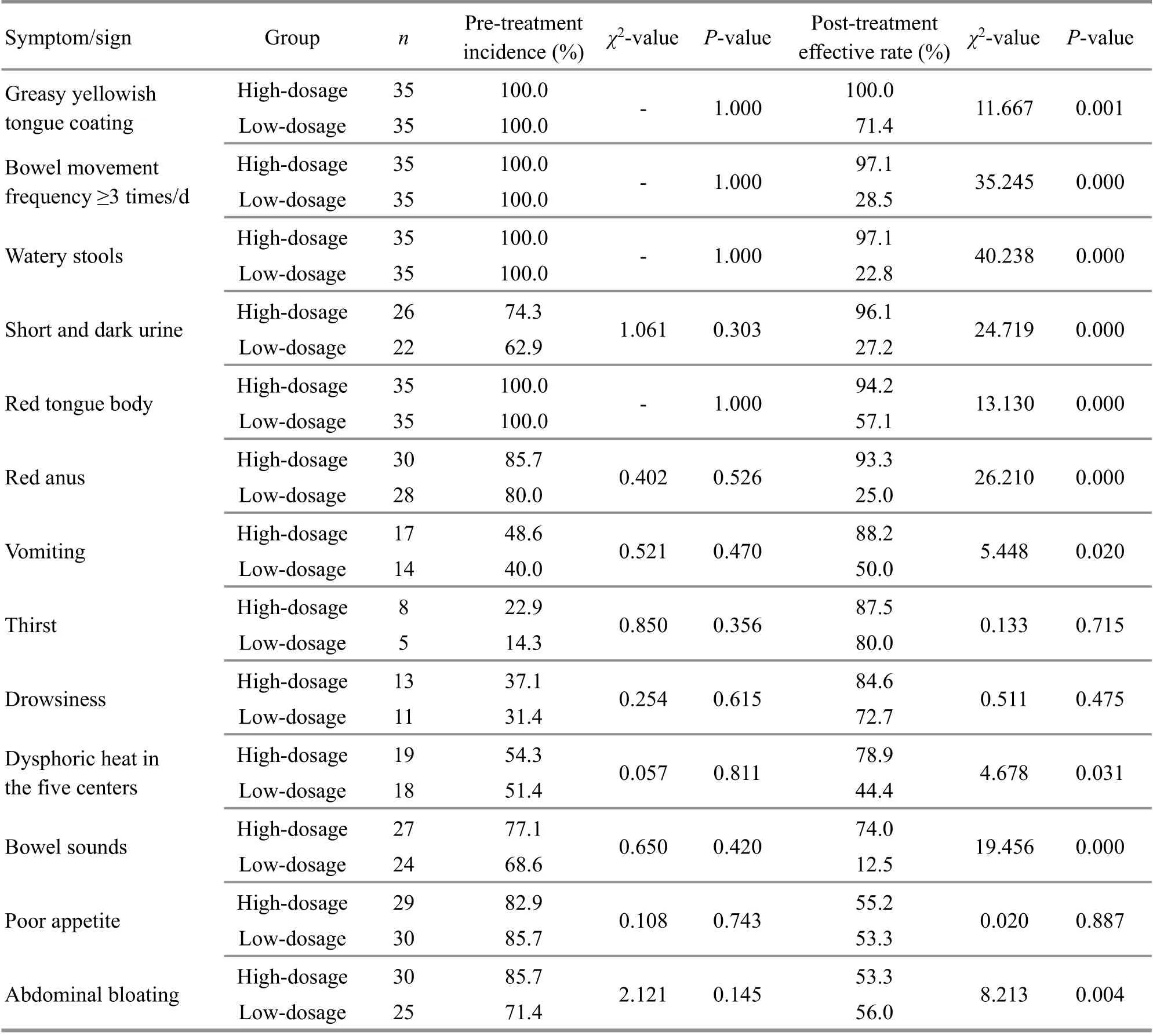
Table 6. Comparison of the effective rates of TCM symptoms and signs (%)

Table 7. Comparison of the TCM symptoms score before and after the treatment [M (min, max), point]
4 Discussion
The umbilical cord is the only channel for the fetus to obtain nutrients to sustain life from the stage of fertilized egg till delivery. Anatomically, the umbilical skin is the thinnest, with no fat tissue underneath but capillaries and venous network[14]. Besides, there distribute rich nerve endings, which means sensitive nervous reflexes.Therefore, it is fast for the umbilical skin to absorb medication to take effect. Moreover, umbilical application avoids the first-pass effect in the liver and stimulation to the gastrointestinal system caused by oral administration. Umbilical therapy is painless, easy to operate, inexpensive, and readily accepted by kids[15].Umbilicus locates the acupoint Shenque (CV8).According to the theory that the Conception, Governor,and Thoroughfare Vessels share the same origin, and the meridian Qi of these meridians all connects with Shenque (CV8), which inspires the saying that “the umbilicus connects to hundreds of collaterals”. External application of medications at the umbilicus can treat internal diseases. Compared with other body areas,numerous physicians have recognized the umbilicus as the optimal region for transdermal administration to get long-term effects.
The Ge Gen Qin Lian Tang prescription consists ofGe Gen,Huang Qin,Huang Lian, andZhi Gan Cao. The main effective compound ofGe Genis puerarin. MO J M[16]discovered that puerarin has a strong transdermal effect.The main effective compound ofHuang Qinis baicalin.HU L X,et al[17]found that baicalin can produce a significant transdermal effect on mice’s skinin vitro. The main effective compound ofHuang Lianis berberine. MA Y G,et al[18]conducted anin vitrotransdermal absorption experiment on mice’s abdominal skin and found that berberine can penetrate the skin, and the volatile oil ofHuang Liancan bolster the transdermal effect. The effective compound ofZhi Gan Caois glycyrrhetinic acid.SONG Y L,et al[19]found that glycyrrhetinic acid is second only to baicalin comparing the transdermal speed.According to the research mentioned above, the main ingredients of Ge Gen Qin Lian Tang prescription are all transdermal and thus can be used externally. Hence, it is theoretically and practically feasible to treat damp-heat diarrhea in kids with umbilical therapy with herbal cakes made of Ge Gen Qin Lian Tang prescription.
After the 3-day treatment, the total effective rate was 97.1% in the high-dosage group and 77.1% in the lowdosage group, suggesting that umbilical therapy with Ge Gen Qin Lian Tang herbal cakes is effective in treating damp-heat diarrhea in young kids. Furthermore, the higher efficacy in the high-dosage group shows that this treatment method’s effectiveness is dosage-dependent,though the exact dose-effect relationship requires further study.
4.1 Umbilical application with high-dosage Ge Gen Qin Lian Tang herbal cakes shortens the time to stop diarrhea
Infantile diarrhea is a self-limited disease, but it often brings about dehydration, electrolyte disorder, and metabolic acidosis. Moreover, persistent diarrhea may lead to hypokalemia, hyponatremia, hypocalcemic convulsion, coma, or shock[20]. Therefore, it is crucial to cease diarrhea opportunely. In this study, the antidiarrheal case number was markedly larger in the high-dosage group than in the low-dosage group after the 3-day treatment (P<0.05), indicating that umbilical therapy with Ge Gen Qin Lian Tang herbal cakes can shorten the diarrheal duration and thus prevent secondary symptoms and complications.
4.2 Umbilical application with Ge Gen Qin Lian Tang herbal cakes improves the TCM symptoms and signs in diarrhea of damp-heat pattern
After the treatment, the TCM symptoms scores changed significantly in both groups (P<0.01), implying that the TCM symptoms improved in both groups. After the treatment, the score was lower in the high-dosage group than in the low-dosage group (P<0.05), and the high-dosage group performed better in improving the symptoms, including greasy and yellowish tongue coating, bowel movement frequency, watery stools,bowel sounds, red and dark urine, and red anus (P<0.01).It indicates that umbilical therapy with Ge Gen Qin Lian Tang herbal cakes can significantly ameliorate the TCM symptoms and signs in damp-heat diarrhea, and the high-dosage ones work better.
4.3 Umbilical application with Ge Gen Qin Lian Tang herbal cakes is safe and reliable
The two groups each had one dropout case due to the kids’ poor compliance. However, no adverse reactions ever occurred during the whole process. Besides, the liver and kidney function indicators were within the normal ranges, so that umbilical therapy with Ge Gen Qin Lian Tang herbal cakes does not impair liver or kidney functions and thus has an excellent safety rating.
In summary, umbilical therapy with Ge Gen Qin Lian Tang herbal cakes can produce satisfactory efficacy for damp-heat diarrhea in young kids and is safe and reliable.Furthermore, it can effectively improve the symptoms and signs, avoid kids’ aversion to oral medications and reduce their discomforts and sufferings, thus more beneficial to early recovery. Meanwhile, we find that the high-dosage herbal cakes produce more significant efficacy than the low-dosage ones, suggesting that the antidiarrheal effect may be dosage-dependent. However,the exact dose-effect relationship requires further study to reveal.
Conflict of Interest
The authors declare that there is no potential conflict of interest in this article.
Acknowledgments
This work was supported by Inheritance and Innovation of Traditional Chinese Medicine Talent Project Millions of National Training Program for Innovative Key Talents of Traditional Chinese Medicine (中醫(yī)藥傳承與創(chuàng)新“百千萬(wàn)”人才工程全國(guó)中醫(yī)藥創(chuàng)新骨干人才培訓(xùn)項(xiàng)目,No. 19Z-1-18); Fund of the Science and Technology Commission of Shanghai Municipality (上海市科委基金資助項(xiàng)目, No. 15401971100); Major National Science and Technology Projects During the 13th Five-year Plan (國(guó)家十三五科技重大專(zhuān)項(xiàng)-腹瀉癥候群中醫(yī)和中西醫(yī)結(jié)合診療方案研究, No. 2017ZX10305501-007).
Statement of Informed Consent
The Ethics Committee of Shuguang Hospital, Shanghai University of Traditional Chinese Medicine approved this trial (Approval No. 2015-434-62-01). Informed consent was obtained from the guardians of the recruited children in this study.Received: 18 November 2020/Accepted: 28 April 2021
 Journal of Acupuncture and Tuina Science2022年1期
Journal of Acupuncture and Tuina Science2022年1期
- Journal of Acupuncture and Tuina Science的其它文章
- Literature review and application experience of needling the Belt Vessel for low back pain
- Investigating the influence of moxibustion on colonic mucosal barrier in rats with dextran sulfate sodium-induced ulcerative colitis
- Clinical study of acupuncture plus Dang Gui Bu Xue Qu Feng Tang for benign essential blepharospasm
- Clinical study on Tuina plus Shen Ling Bai Zhu San in treating children with diarrhea due to spleen deficiency
- Observation of the efficacy and safety of the Song-Relaxing and Zhen-Vibrating abdomen manipulation for patients with prediabetes
- Effects of acupuncture combined with Brunnstrom staging on upper-limb motor function, cerebral arterial blood flow velocity, and brain function remodeling after stroke
