Factors influencing the degree of participation in surgical decision-making among Chinese patients with prostate cancer:A qualitative research
Jie Co ,Chunxue Peng ,Xioying Lu ,Lingjun Zhou ,Jing Wu
a Department of Urology,Changhai Hospital,Naval Medical University,Shanghai,China
b Department of Nursing,Changhai Hospital,Naval Medical University,Shanghai,China
c School of Nursing,Naval Medical University,Shanghai,China
KEYWORDS Prostate cancer;Participation;Decision-making;Surgery;Influence factors;Qualitative research
Abstract Objective:There was increasingly demand of participation in surgical decisionmaking among Chinese patients with prostate cancer.However,due to the complex healthcare system and advanced care settings,it is quite challenging for the patients to gain sufficient support from the institute and the government.This research aimed to investigate the factors that impact the degree of participation in surgical decision-making among Chinese prostate cancer patients.Methods:A phenomenological approach of qualitative research based on the results of semistructured interviews was adopted,to explore the influencing factors which hinder the participation in surgical decision-making.Consolidated Criteria for Reporting Qualitative Research were utilized.Up to 160 post-operative patients who had undergone radical prostatectomy along with 68 medical and nursing staffs,were purposively recruited in this research.This retrospective study was carried out from September 2018 to August 2019.After recording and transcribing the interviews,the interview materials were evaluated via the Colaizzi’s seven step approach and the NVivo Version 10 software to analyze the interview content.Results:According to the analysis and summary of the interviews,there were three factors affecting the degree of participation in surgical decision-making.Firstly,insufficient information was provided by medical and nursing staffs because of their lack of time,proper communication skills,and career experience,as well as difficulties in the development of patient decision aid and inconsistent resource availability.Secondly,the cognitive level of decisionmaking among patients was relatively low due to poor psychological endurance,insufficient amount of education,senility,and less knowledge and information demand.Ultimately,decisions were constantly made by family members with/without patients.Conclusions:The degree of participation of Chinese prostate cancer patients in the surgical decision-making had much space for improvement.?2022 Editorial Office of Asian Journal of Urology.Production and hosting by Elsevier B.V.This is an open access article under the CC BY-NC-ND license(http://creativecommons.org/licenses/by-nc-nd/4.0/).
1.Introduction
Prostate cancer(PCa)is one of the most common human malignant tumors and the second leading cause of death in male worldwide[1].With the trend of an aging society,the prevalence of PCa is increasing every year,and has become the ninth leading cause of cancer deaths in China[2].The surgical methods of PCa are diversified,and the patient’s autonomy and right to choose the surgical method also need to be fully embodied.
In the 1990s,Charles et al.[3]firstly proposed the idea of shared decision-making.It was based on good communication,during which doctors determine the surgical decision-making and treatment options in combination with patients’preferences[4].Shared decision-making can encourage patients’participation to arrive at the best decision so as to promote a good medical outcome and prevent patients’regret afterwards[5].To achieve the goal of shared decision-making,the following standards must be met:Both the doctors and the patients have a clear understanding of the patient’s condition;all information and consultations about the disease are amongst open access resources;the doctors and the patients have a unified goal on the outcome of patient treatment;all kinds of medical treatment should be deliberate between the doctors and the patients;both the doctors and the patients are aware of the consequences of different medical treatments.
Domestic researches[6,7]on cancer patients’participation in decision-making showed that patients’actual participation was relatively less than sufficient,and we still lack tools and clinical applications to shared decisionmaking amongst cancer patients[8].Studies abroad showed that the options of surgical treatments for PCa patients were mainly determined by urologists and influenced by the level of stress the patient’s family[9].At present,there is no qualitative study on the degree of PCa patients’participation in surgical decision-making in China.This study focused on the influencing factors of surgical decision-making of PCa patients through interviews with patients who were informed with the diagnosis of PCa,as well as with the medical and nursing staffs who were specialized in the treatment of PCa,in order to offer better clinical patient decision aid(PDA).
2.Methods
A phenomenological approach was applied to the qualitative study,and the data were collected through individual in-depth interviews. The goal of phenomenological research is through describing the complexity of the world experienced by the participants in order to discover the common meanings underlying empirical variations of a given phenomenon,and the ultimate purpose is to discover the essence[10].
2.1.Participants
Participants were recruited in a urology center of a general tertiary hospital in Shanghai because of its outstanding clinical and research performance.The research was conducted from September 2018 to August 2019.The patients were screened by the investigators with the target sampling method according to the outpatient appointment list of urological experts.The investigators then determined the eligibility of patients for the study.Patients were included if they were(a)aware of their disease and conditi on,(b)fully conscious without any communi cati on dysfunctions,(c)scheduled for radical prostatectomy,(d)fully informed of the research contents.Patients were excluded from this study if they had difficulties in communicating using Mandari n,mental illnesses,severe cogni tive impairments,or difficulties in communication.Researchers also invited medical and nursing staffs with different professional titles, educational backgrounds, and experience in the urology center to participate in this study.General information of patients with PCa,as well as medical and nursing staffs were collected(Appendix 1).The number of participants was determined by data saturation,until no new themes emerged during the coding process[11].We interviewed 160 patients and 68 medical and nursing staffs.The unqualified interview material s(such as the content deviation from the research topic and vague expression) were excluded,and finally the i nterview data of 34 patients and 16 medical and nursing staff were included.The patients’characteristics are shown in Table 1 and medical and nursing staffs’characteristics are shown in Table 2.
2.2.Preparation before interview
2.2.1.Researchers
The researchers consisted of two professors and four clinical workers with qualitative research experience.They are good at communicating with patients and understanding the real situation of patients and clinical work,which is conducive to obtaining true and comprehensive information in the research.
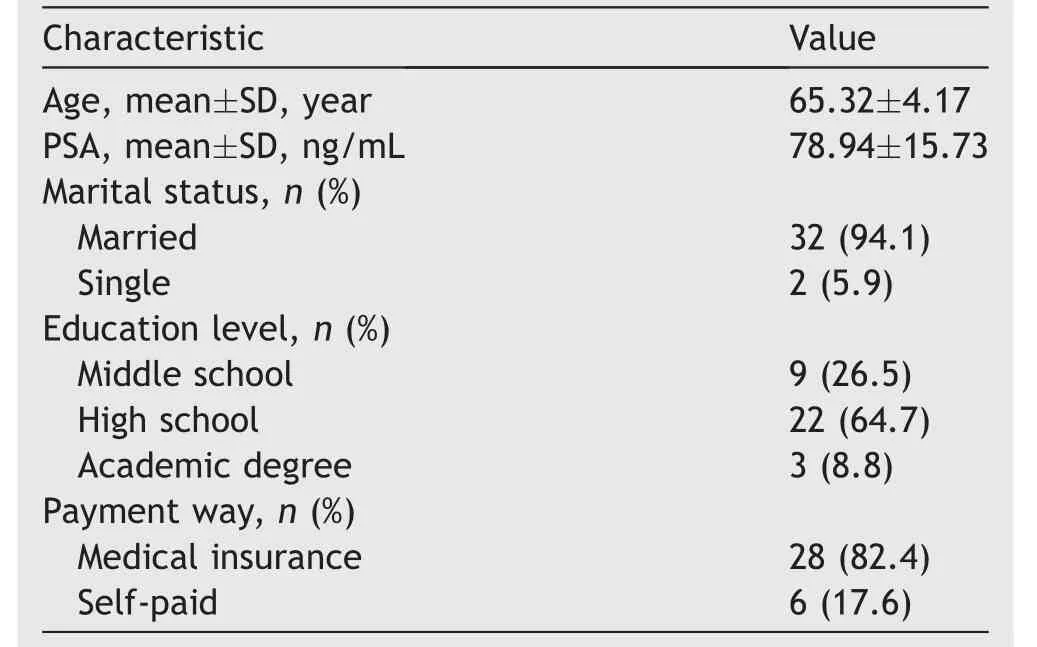
Table 1 Characteristics of patients(n=34).
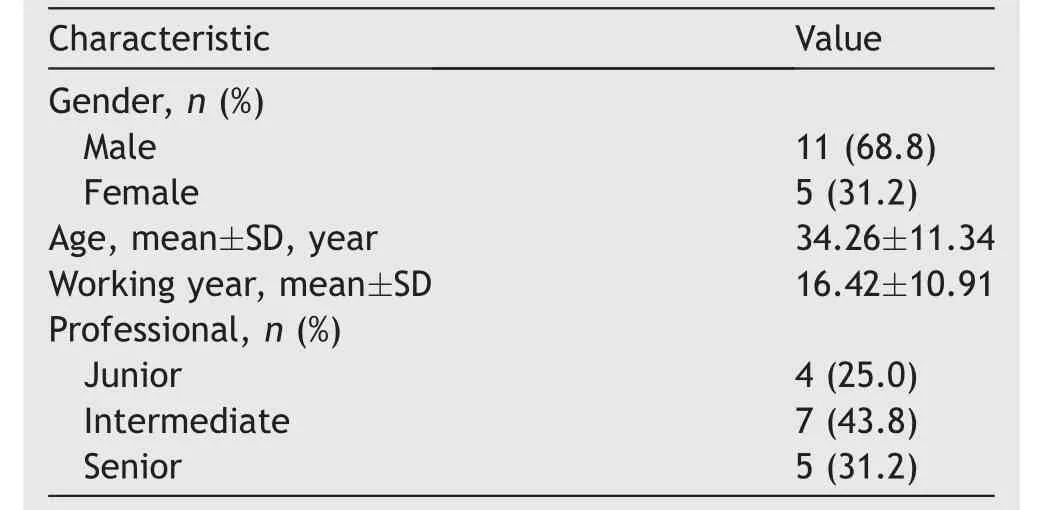
Table 2 Characteristics of medical and nursing staffs(n=16).
2.2.2.Research tools
Prepare some notebooks,neutral pens,a laptop,and a voice recorder.
2.2.3.Interview outline
Through searching the relevant data at home and abroad about the decision-making factors of PCa surgery,we reviewed the published researches,consulted the medical experts who specialized in the treatment of PCa,combined the researchers’clinical experience,and then designed the preliminary interview outline.Before the interview,experts with qualitative research background were invited to provide guidance to researchers from the aspects of communicating skills and data analyses.The researchers firstly conducted a pilot interview with three participants(one patient,one medical faculty,and one nursing staff),and modified the questions which were answered vaguely by the participants.In the process of interview,we paid attention to the direction and scope of the interview,avoided the interviewers’digression from the topic and omission of important contents,revised the ambiguous problems in the outline,and supplemented the missing contents.After the revision,the interview entries included more specific questions that enabled the participants to express their feelings more clearly.Questionnaires of patients’participation in surgical decision-making,and questionnaires of medical and nursing staffs on patients’participation in surgical decision-making are shown in Appendix 2.
2.3.Data collection
The researchers contacted the interviewees in advance,made an appointment,and arrived at the interview place in advance.Before the interview,they checked whether the equipment was in good condition and debugged to ensure that the research tools were in functional state.The interview was carried out in a quiet room in the outpatient department,in order to let the participants express their feelings more comprehensively and to get information as complete as possible.
Semi-structured interview is the preferred method of data collection in phenomenological analysis and recording.This method enables participants to reflect through communication,thus facilitating more in-depth discussion.Before the interview,the researchers briefly introduced the purpose and content of the research,so that they had a preliminary understanding of the research.The investigators adopted an open-ended interview in a process that the order of the questions was used flexibly depending on the flow of the interview.
The interview began with the questions:“Please tell me about your decision-making experience?”“How did you make the decision on your surgery?”“How much did you participate in making this surgical decision?”.The interviewer paid careful attention to participants’responses,and then asked the following questions:“In which aspect would you like to participate?”“were your initial ideas consistent with your final decision?”“Did you communicate with doctors about the surgical decision-making plan?”“Did you understand the information related to decision-making provided by the medical staffs?”“Did the doctor take your points and ideas into consideration?”“were you satisfied with your decision during the entire surgical procedure?”.This approach allowed the interviewer to probe into detailed experience of participants further[12].When switching questions,the researchers firstly made an appropriate summary of the previous narrative,and then transitioned to the next one naturally.We commenced the interview with simultaneous recording,and each interview time was controlled approximately 30 min to 1 h.Participants were encouraged to express their feelings and thoughts as much as possible in the process.Interviewers listened carefully and proposed questions in a timely manner with an objective language with no guidance or comment.Meanwhile,we recorded the interviewees’gestures and emotions objectively in order to analyze the data later.
At the end of the interview,the interviewees filled in the general information questionnaire,and then confirmed the contact information to facilitate the verification at the later stage.
Finally,the data of 34 patients and 16 medical and nursing staffs were analyzed and returned to each interviewee in the form of documents to verify the authenticity and accuracy of the contents.
2.4.Data analysis
Each interview was transcribed verbatim from the audio recordings within 48 h of the interview session.The interview materials were evaluated with the Colaizzi’s seven-step framework[13,14]:(1)The researchers read each interview carefully to obtain an overall understanding of the decision-making process of each patient;(2)the important sentences in the interview materials were inspected and the most meaningful statements were extracted;(3)the meaningful statements were carefully studied and coded,such as“insufficient time”“l(fā)ack of communication skills”“difficulties in the development of PDA” “insufficient career experience” “inconsistent resource availability”;(4) the coded phrases were emerged as three themes and 11 subthemes,such as inadequate information provided by medical and nursing staffs;(5)the themes and subthemes were integrated into the patient’s surgical decision-making process and described in detail;(6)the basic structure of the factors affecting patients’surgical decision-making was established;(7)finally,the themes were returned to 34 patients and 16 medical and nursing staffs to verify the authenticity of the results.
The researchers used NVivo Version 10 software(QSR International,Melbourne,Australia)to analyze the meaningful statement and coded.The data collection and analysis occurred concurrently.The coding process included three distinct phases:(1)Open coding—this phase separated the theme or concept from the data,and then generated codes,during which we were able to encode using our own language or the original content;(2)axial coding—the researchers selected the content of the initial codes,carried on the clustering process,and made connections between the categories;(3)select coding—we collated and refined the code for each category,and established the relationship between categories and subcategories[15].Any discrepancies about the theme were discussed until a consensus had been reached.The words used for coding were based on the researchers’explanation and terms from related literature.As a result,there were three central categories in this study.We described the formulation of the three central categories exhaustively,quoted the original descriptions for authenticity,and established the fundamental structure of the research.The final obtained results were shared with the participants to ensure reliable results,and the researchers would confirm the findings with the participants.Interview replies,the transcription,and results of data analysis were cross-verified to reach data triangulation.Applied triangulation can decrease researcher bias,provide a variety of perspectives for the phenomena under the study,and increase its validity[16].
In this study,the use of phenomenology had not only promoted the rigorous of this research,but also provided a deeper understanding of the interview context.The intention was to investigate the influence factors in the degree of participation in surgical decision-making among Chinese PCa patients.Criteria for reporting qualitative research,which contained a 32-item checklist for interviews and focus groups[17],were adhered when writing the manuscript(Appendix 3).
2.5.Rigor
For the trustworthiness of the qualitative study,we followed the Lincoln and Guba’s criteria[18]:Credibility,transferability,dependability,and confirmability.Credibility was achieved in the study through triangulation.Transferability was set up based on massive data collection and exhaustive description of data.The dependability and confirmability were established by the researchers with qualitative experiences applying triangulation in the data collection and analysis.In order to decrease the bias,the study group held meetings frequently to discuss the differences among them until arriving at the final consensus,so as to ensure that the interpretation of the theme cluster was meaningful and reasonable.
3.Ethical considerations
In this study,we adhered to the ethical principles,including respect,competence,responsibility,and integrity.Before receiving the interview,information about the study,voluntary participation principle,and the confidential handling of the interview content were described to each interviewee.Then,patients,their family members,as well as medical and nursing faculties were given informed consents for participation.Permission to conduct this study was provided by the Nursing department of Changhai Hospital,received Institutional Review Board(IRB)approval of Changhai Hospital(approval No.CHEC2020-111).
4.Results
After analyzing and summarizing the data through interviews,three themes were summarized:(a)Inadequate information provided by medical and nursing staffs;(b)low cognitive level of patient’s decision-making;(c)influence of family members in patients’decision-making.
4.1.Inadequate information provided by medical and nursing staffs
4.1.1.Insufficient time
Although medical and nursing staffs were considered the most important and reliable providers of medical information[19],we spotted that due to lack of sufficient communication,the information exchange between patients and medical and nursing staffs before surgery was insufficient.
Doctor 18:“We need to go to the operation room immediately after we make the rounds,so we do not have much time to explain to the patient clearly.”
Doctor 3:“There are many operations every day,and we are too tired to talk after the operation.”
Nurse 1:“The clinical workload is overwhelming,and there is no more time to think about how to make every point clear to the patients.”
Nurse 26:“We have been trotting at work.We can’t get off work on time if we work too slowly.As for those elderly patients with problem of understanding or hearing,explaining the surgical knowledge takes a lot of time,and it will increase our workload.”
Patients expected to obtain adequate information about their diseases before surgery and communicate with the surgeons or nurses.However,when patients saw that the medical and nursing staffs were busy,they gave up consulting the problem or seeking help.Because some patients were unable to receive sufficient medical information during consultations,these patients would be less involved in decision-making.
Patient 9:“No way.The doctor is busy.I should not bother him.I can understand it by myself.If I do not understand the procedures of the surgery,I will ask the nurse when it is convenient for her”.
Patients 11:“I can see the attending doctor once a day;sometimes they have already finished the daily rounds of ward before I wake up.When I want to ask them,I could not find the doctor.”
Patient 48:“The doctor told me about my operation.I thought the doctor was busy.Even if I did not understand,I would not ask him again.”
4.1.2.Lack of communication skills
Good doctor-patient communication can promote the patient’s participation in surgery decision-making.This study found the lack of communication skills for some medical and nursing staffs,which was not conducive for patients to obtaining sufficient information to assist in decisionmaking.
Doctor 21:“Maybe there are many medical terminologies in our expression,and many patients can’t understand them.I will tell the patient the operative procedures by sketching,but I don’t know if they can understand.”
Nurse 3:“I want to introduce the knowledge of the disease to patients,but I don’t know how to explain it to patients more easily.It’s too abstruse for them.”
Nurse 33:“Sometimes if they can’t understand what I said,they would ask me repeatedly,but I don’t know how to explain it in a plain language.”
Poor communication increased patients’fear of illness,hindered patients’participation in decision-making,and was not conducive to the consensus of decision-making between doctors and patients.
Family member of Patient 15:“After the doctor talked with my father,my father was confused and shocked,and he was worried that all the complications would happen to him after the operation,so he asked me to make decision with the doctor.”
4.1.3.Insufficient career experience
This study found that senior medical and nursing staffs experienced in clinical work could guide patients to make decisions in accordance with their condition.The knowledge and experience of junior medical and nursing staffs were relatively insufficient,who could not provide detailed information about the illness,as well as the diagnosis and treatment for the patients.The surgeons with less clinical experience felt uncertainty when they faced the complex condition.
Surgeon 40:“Sometimes I can’t say anymore.If the content I said is inconsistent with the professor,I will lose the trust of my patient;I have to know more about it first.”
Nurse 5:“I’m senior and know more about the disease.I often help them to explain and communicate with patients.Some of junior nurses’basic knowledge is insufficient,let alone to ask them to guide patients.”
Nurse 19:“Only by accumulating more knowledge and participating in learning can we provide patients with high-quality nursing care.”
4.1.4.Difficulties in the development of PDA
PDA can be a valuable tool in providing information on different treatment options and improving the quality of care[20].However,their implementation in practice is hampered by several barriers perceived by clinicians,such as a lack of confidence in the PDA and the concerns of occupying too much time.Patient-centered design has been proposed as a way to make PDAs more suitable for clinical implementation[21],but there is a lack of PDA for PCa patients in China.This study indicated that some medical and nursing staffs wanted to promote the development of clinical PDAs.Due to the lack of financial support,many PDAs have not been developed.
Surgeon 21:“We can spare some time to make health panels,manuals,and a web-based tool,so that patients can know more about disease knowledge,but our funds are limited.”
Nurse 54:“I also designed and made the illustrated manuals of PCa.It was printed out in brochures and was taken by the patient’s family quickly.The color print was expensive,especially when there was no special funding.”
4.1.5.Inconsistent resource availability
Surgeons hold a prevailing opinion that hospitals in China provide various equipment along with different approaches,such as the advanced Da Vinci system.In the academic hospitals,the surgeons can learn more advanced medical knowledge and technology.
Training surgeon 22:“I have never done this kind of surgery in our hospital,let alone lecturing them,so I came this academic hospital to learn advanced knowledge and technology.”
Training surgeon 9:“Due to the restrictions of funding and policy,our hospital is unable to introduce Da Vinci Robot;I hope I can learn this operation approach in this advanced hospital.
4.2.Low cognitive level of patient’s decisionmaking
4.2.1.Poor psychological endurance
The patients were worried about the postoperative recovery and quality of life,and they would regret for the choice of the surgery decision.
Patient 9:“I heard fromthe professor that there might be many complications after the operation.I think my body may become worse after surgery than it is now.Since I am 71 years old,my body can’t endure this process.”
Surgeon 5:“Some patients worry about the serious complications occurring to themselves,so we can’t talk more about the complications,otherwise they will be very anxious.”
Some patients heard the sufferings of relatives and friends who had undergone the same surgery,it would reduce patients’initiative for participating in surgical decision.
Patient 34:“My friend’s father suffered from the same disease,who relapsed quickly after the operation,and his situation is not very good.My father is afraid that the postoperative situation will be the same with him,so he is reluctant to have the operation now.”
4.2.2.Low level of literacy
Patients with bachelor’s degree or above would understand the knowledge and treatment of diseases well,and did not want to be in a passive position in the decision-making process[22].In this interview,we found that patients with high education level had strong willingness to take part in surgery decision-making.
Patient 31:“My health is up to me;I will take the initiative to ask the doctor to help me understand my condition,and otherwise how can I confirm anything else!”
Patient 17:“I read the book of Professor*(the professor’s last name was omitted here)before I was hospitalized and inquired the information on the internet;I found the best professor,so I came here.I’ll communicate with the professor for the treatment plan on my mobile phone.”
Patients with low educational level were unable to understand the medical terms and complex conditions because of lack of knowledge about diseases.Therefore,patients preferred to listen to doctors or family members.
Patient 18:“What the doctor said is too professional to understand,but I think the hospital is very good and we believe them.”
Patient 7:“I have few knowledges about my disease and have to trust the surgeons.I’ll do what the doctor said.”
4.2.3.Elder age
Because of the impairment of understanding and cognitive function,the awareness of acquiring knowledge and treatment of disease is not strong in elderly patients.Medical and nursing staffs are reluctant to spend much time communicating with them.In decision-making,patients want help from relatives and friends,resulting in a passive attitude of elderly patients in the decision-making process[23].
In this study,we found that the elder age,as a group characteristic of patients,hindered patients from participating in surgery decision-making due to the degeneration of physiological function.
Patient 61:“My hearing is not good;I had difficulty in communicating with the doctor and my daughter had to translate between us,so I left the talk to them.”
Patient 10:“As an old man like me,I do not expect to live for many years,so I do not worry.Let doctor and my children decide.”
4.2.4.Less knowledge and information demanded
Some patients reduced the need for information on disease diagnosis and treatment because they had difficulty in understanding complex medical knowledge.Patients could not perceive the risk of their disease or the significance of treatment accurately,nor could they participate in decision-making actively.
Patient 28:“I didn’t understand what they said,so I left all my decisions to my son.”
Surgeon 2:“Sometimes I want the patients to listen to how the operation is done,what condition of the disease is,and what risks they will take for surgery.They would say they do not need to listen to it.His family makes decisions and I cannot force them to listen.
4.3.Influence of family members in patients’decision-making
4.3.1.Family members and patients made decisions together
Influenced by Chinese traditional cultural background and social situation,every family member feels obligated to take care of others,especially when the family member is ill or encounters difficulties[24].Family members helped patients collect relevant information and treatment methods of the disease from many aspects,and chose the appropriate therapy for the patient.
Family member of Patient 34:“When I knew that my father was ill,I asked for help from my relatives and friends and visited the Hao Daifu(it means“good doctors”in English)website to know something about the relevant information and therapy about my father’s disease.”
Patients acquired information about disease treatment decisions and preferred to consult relatives and friends,instead of doctors[17].They wanted relatives or friends to participate in doctor-patient communication and help make surgery decisions.
Patient 14:“The surgery decision is yet to be discussed
by my families.”
Patient 17:“Our parents have passed away,so we have to consult with my relatives and make a joint decision.”
Patient 18:“How can I decide such an important thing by myself?It must be decided by my family together.”
4.3.2.Family members made decisions for the patient instead
However,we found that some family members worried about the patients’losing control over their emotions after they knew their actual situation and couldn’t communicate well with doctors,so some family members deprived the patients of their decision-making autonomy and made decisions directly.
Patient 27:“My son said that I would be all right after the operation and that I could live like a normal person in the future.”
Family member of Patient 4:“My dad listened to my advice.I always find the best doctor to treat him.Therefore,he does not worry about the operation.”
Patient 39:“My son said that he would take care of everything.I am old so I depend on my son.What should I worry about?”
5.Discussion
Our research showed that Chinese PCa patients were not enthusiastic participants in the surgical decision-making process,showing negative and passive attitude.The decision-making process was described as the interaction of three aspects consisting of a doctor,a patient,and a background factor[24].As far as patients are concerned,participating in shared decision can have a comprehensive understanding of their disease and treatment methods,and improve prognosis;for doctors,they do not have to take all peri-operative risks by themselves.They can not only get the understanding of patients and their families,but also be free from some difficult treatment options,which is also conducive to the clinical work.
5.1.Strengthen medical staff’s professional knowledge and interpersonal communication skills and promote the implementation of shared decision-making
The implementation of shared decision-making requires the participation of multidisciplinary teams.Specialized medical and nursing staffs can provide professional information,evaluate patients’needs for decision-making,and supervise the implementation of PDAs in patients’decisionmaking process,so as to promote the implementation of shared decision-making effectively[25].This study found that the junior nurses could not communicate with patients effectively because of the limitation of their professional knowledge,thus affecting the degree of patients’participation in decision-making.
Managers need to strengthen the training of junior medical and nursing staffs.In addition,Giguere et al.[26]have concluded that improving the communication skills of medical and nursing staffs can improve the enthusiasm of patients to participate in decision-making.When communicating with the patients,they feel that they are treated with dignity and friendliness.Specialized medical and nursing staffs also need to enhance interpersonal communication skills,which can not only change the traditional concept of doctors leading diagnosis,but also promote patients to communicate with medical and nursing staffs actively,express their thoughts,and participate in decision-making.
5.2.Ensure the patient’s autonomy to participate in surgery decision-making and improve shared PDAs
The study found that due to the influence of patients’educational level and age,and the constraints of traditional culture,some patients’surgery decisions were made directly by relatives and friends.Sometimes even the patients themselves were excluded from the decision,which was a deprivation of patient autonomy in decision-making.Specialized medical and nursing staffs introduced the basic treatment information and nursing measures to patients in a simple and easy language,and analyzed the advantages and disadvantages of all optional treatment by the decision-making manuals,videos,and health knowledge lectures.At present,diversified health education has been introduced,such as rehabilitation assistance,WeChat,and multimedia based on information platform.It has been helpful in clinical work and aids to meet the needs to acquire health knowledge for patients[27].However,the quality of health education knowledge is unbalanced,and some professional terms are still difficult to understand,and there are many limitations in the application of PDAs,such as high cost,complexity in operation,and prolonged time for clinical application[28].Therefore,it is urgent to develop an intuitive and easy approach of implementing PDAs to improve the application effect in the outpatient clinic for PCa patients in China.At the same time,different levels of PDAs should be implemented according to the patients’wishes and health literacy level.For example,for patients with low level of health literacy,the intuitive and illustrated brochures on prostate knowledge could be offered,and they could be guided to read the publicity column on the treatment of PCa in the department and provided with explanation of professional knowledge by nurses;for patients with intermediate level of literacy,specially designed manual on the comprehensive treatment of PCa and multimedia lectures on health education could be given to them;for the patients with high level of literacy,books with detailed disease description could be offered to them.Measures above may contribute to improving quality in medical service for patients,as well as their ability to participate in a better decision-making.
6.Conclusion
The degree of participation of Chinese prostate cancer patients in the surgical decision-making has much space for improvement.It is necessary for clinicians to provide appropriate assistance during patient decision-making by offering a shared decision-making system based on clinical practice so as to enable patients to obtain the essential information throughout the treatment,and to ultimately improve patients’degree of participation.
Author contributions
Study design:Jie Cao.
Data acquisition:Lingjun Zhou,Jing Wu,Chunxue Peng.
Data analysis:Xiaoying Lu.
Drafting of manuscript:Jie Cao,Chunxue Peng.
Critical revision of the manuscript:Xiaoying Lu.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgements
This study was supported by the National Natural Science Foundation of China(NSFC-81903182)and Top-Notch Project of Youth Cultivation Project of Nursing Peak Discipline of Naval Medical University(18QPBJ12).
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajur.2021.08.003.
 Asian Journal of Urology2022年2期
Asian Journal of Urology2022年2期
- Asian Journal of Urology的其它文章
- Manuscript Guide for Authors
- Encrusted cystitis and ascites due to urethral calculus
- Clinical features and management of ureteric stump syndrome:Singlecentre experience and contemporary literature review
- Impact of coronavirus disease 2019 on semen parameters
- Clinical lesson learned from genetic analysis in patients prior to surgical repair of hypospadias
- Impact of delay from transperineal biopsy to radical prostatectomy upon objective measures of cancer control
