Shrinking lung syndrome in autoimmune inflammatory diseases: A case series and review of literature
Xiao-chan Chen, Shan He, Jing Xue
1 Department of Rheumatology, the Second Affi liated Hospital of Zhejiang University School of Medicine, Hangzhou 310009, China
2 Department of Rheumatology and Immunology, the Affi liated Jinhua Hospital of Zhejiang University School of Medicine,Jinhua 321000, China
Dear editor,
Shrinking lung syndrome (SLS), a rare complication of autoimmune inf lammatory diseases, is mainly associated with systemic lupus erythematosus (SLE), with an occurrence in 1%–2% of cases.It is characterized by restrictive defects on pulmonary function tests (PFTs)associated with reduced lung volume. SLS has also been reported in cases of primary Sj?gren syndrome (pSS),scleroderma,rheumatoid arthritis,mixed connective tissue disease,and undifferentiated connective tissue disease. Herein, we present three case reports of SLS,including two patients with SLE and one patient with adultonset Still’s disease (AOSD) (Table 1).
CASE 1
A 14-year-old girl with fever, facial erythema, arthritis,and proteinuria was diagnosed with SLE in 2006. In May 2018, she presented with exertional dyspnea, cough, and rash recurrence. Chest computed tomography (CT) showed right lower lobe atelectasis, elevated right diaphragm, mild bilateral pleural effusion, and pleural thickening, without interstitial pneumonia (Figure 1). PFTs showed forced vital capacity (FVC) 62.5%, total lung capacity (TLC) 69.9%,forced expiratory volume in the f irst second (FEV1) 67.3%,and diffusing capacity of the lungs for carbon monoxide(DLCO) 42.4%, consistent with a restrictive pattern. SLE disease activity index (SLEDAI) was 10 (high disease activity). Methylprednisolone (MP) 60 mg/d was initiated and her dyspnea and cough were signif icantly improved after 2 weeks. Chest CT also showed improvement in atelectasis and elevated diaphragm. Pulse therapy of cyclophosphamide(CYC) was performed monthly. In January 2019, MP was maintained at 8 mg/d and CYC was discontinued after the accumulated dose reached 5.4 g. PFTs revealed FVC 78.6%,TLC 76.6%, FEV1 73.0%, and DLCO 49.9%, representing marked improvements. At the most recent evaluation in May 2021, she was in good condition on MP 4 mg/d,hydroxychloroquine 0.2 g/d, and tacrolimus 2 mg/d.
CASE 2
In January 2021, a 53-year-old woman diagnosed with SLE presented with dyspnea, pleuritic chest pain,and lower extremity edema, without fever or cough. Chest CT showed right lower and left upper lobe atelectasis and bilateral pleural effusion, without interstitial pneumonia(Figure 1). PFTs confirmed a restrictive pattern with FVC 59.1%, TLC 72.2%, FEV1 65.0%, and DLCO 55.2%. She had kidney and heart involvement at the same time and very high SLEDAI of 20. MP 500 mg/d and intravenous immunoglobulin 20 g/d for 3 d were given simultaneously,followed by MP 80 mg/d and CYC 0.8 g monthly as continued therapy. Her symptoms, including dyspnea and pleuritic chest pain, improved significantly. Repeated chest CT showed improvement in atelectasis and pleural eff usion.In September 2021, 8 pulses of CYC (accumulated dose 6.4 g) were completed and MP was gradually tapered to 8 mg/d. FVC increased to 76.6% with TLC 79.9%, FEV1 81.5%, and DLCO 69.5%, and lung CT showed complete recovery from atelectasis and pleural eff usion.
CASE 3
A 68-year-old woman presented with remitting fever and transient rash since September 2020, and was diagnosed with AOSD according to the Cush criteria. She had a good response to full-dose MP, but fever and rash recurred when glucocorticoid was withdrawn by herself. In January 2021,she developed progressive aggravating dyspnea. Chest CT showed obvious elevated right diaphragm and right lower lobe atelectasis (Figure 1). PFTs confirmed a restrictive pattern with FVC 72.4%, TLC 66.9%, FEV1 74.8%, and DLCO 50.4%. Electroneurographic studies of the phrenic nerves showed bilateral partial motor neuropathy that was more severe on the right side. The patient initiated treatment with MP 160 mg/d and CYC 0.8 g monthly. Fever and rash were gradually relieved. Unfortunately, CYC was discontinued after 3 pulses because of side effects. In the following 6 months, MP was gradually tapered to 8 mg/d.Dyspnea was mildly alleviated, but there were no signif icant improvements in PFTs and chest CT.
DISCUSSION
We searched the National Library of Medicine PubMed database for relevant literature using the key term “shrinking lung syndrome”. A total of 223 SLE patients and 9 non-SLE patients (supplementary Table 1) were obtained from 70 articles published between 1965 and June 2021 in English, French, and Spanish. Together with the three patients reported in this article, the demographic and clinical characteristics of 225 SLE patients and 10 non-SLE patients are summarized in Table 2.
The physiopathology of SLS has not been well described. The following hypotheses have been developed: (1) excessive surface tension related to loss of surfactant on alveolae; (2) respiratory muscle weakness; (3) diaphragmatic myopathy; (4) phrenic nerve dysfunction; (5) pleural adhesion; and (6) pleural inflammation-related inhibition of deep inspiration by neural reflexes.Unfortunately, none of these hypotheses have been confirmed to date. Among them,phrenic nerve dysfunction is considered an important cause of SLS, existing in 30% of reported cases. Phrenic nerve involvement is one of the localizations for mononeuritis multiplex that can be induced by primary diseases like SLE and pSS. Neurological complications have also been described in AOSD, with involvement of the peripheral and cranial nerves.Case 3 presented with recurrent fever and progressive aggravating dyspnea without pleuritic chest pain and pleural eff usion. Therefore, phrenic nerve dysfunction may be responsible for her SLS.

Figure 1. Chest computed tomography of the three patients in this case series.

Table 1. Main clinical characteristics of the three patients in this study
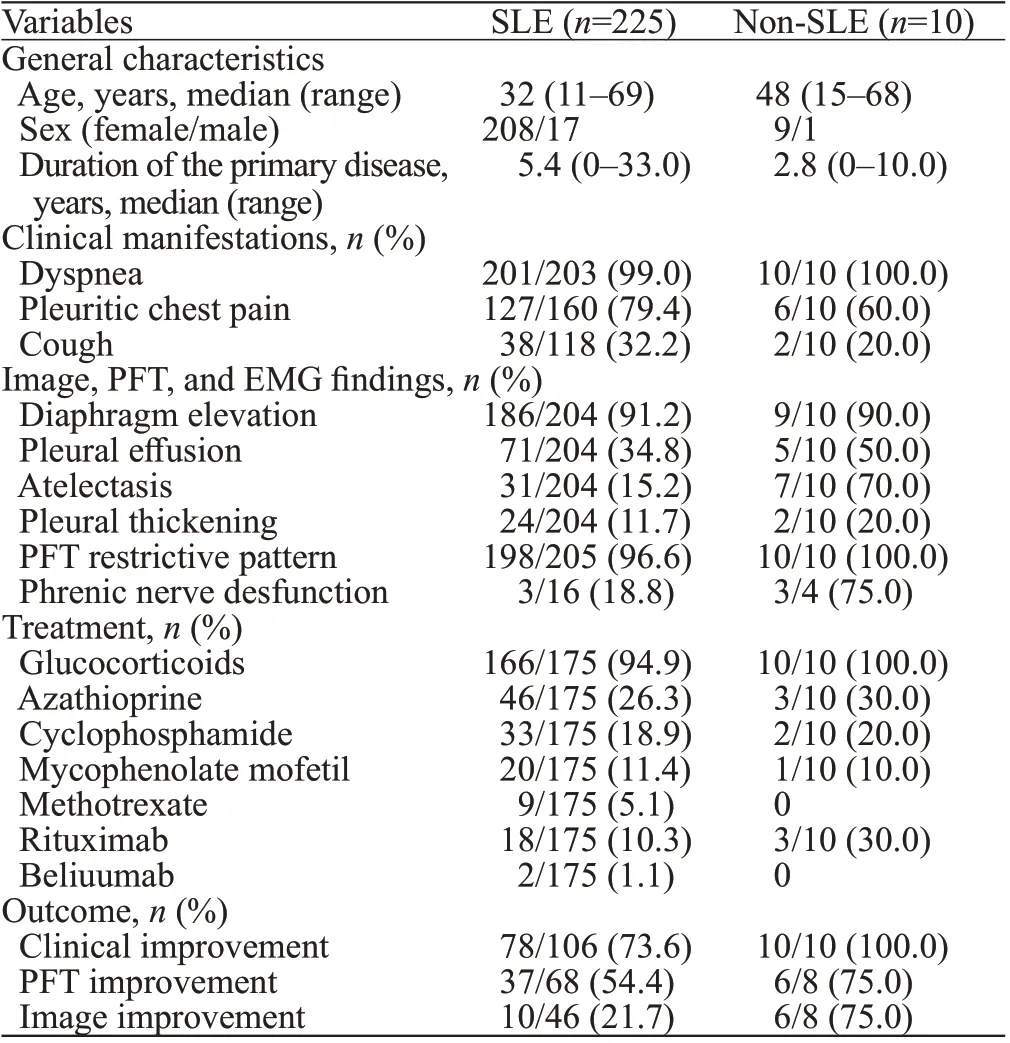
Table 2. Clinical characteristics and outcome of 225 SLE patients and 10 non-SLE patients with shrinking lung syndrome
Diagnosis of SLS relies on the following factors:unexplained dyspnea, reduced lung volume, and restrictive defects on PFTs, without simultaneous interstitial, alveolar,or pulmonary vascular disease. There is no consensus treatment for SLS in the absence of large sample clinical trials. Medium or high doses of glucocorticoids are the first-line treatments to reduce inflammation and regulate immunity. Azathioprine and CYC were the most frequently reported immunosuppressive agents.Rituximab and belimumab were also eff ective in a few severe or refractory cases.Theophylline and beta-agonists were beneficial for some patients to increase diaphragmatic strength and decrease diaphragmatic fatigue. In most reported cases,lung function was improved after timely and active treatment.
CONCLUSIONS
SLS is a rare respiratory manifestation in various autoimmune inflammatory diseases. The main characteristics of SLS are restrictive patterns on PFTs and reduced lung volume on chest imaging. Glucocorticoids and immunosuppressive agents are effective in most patients with CTD-related SLS. Heightened awareness and early identif ication of SLS are important to improve the disease prognosis.
None.
This study was approved by our local ethics committee and performed in accordance with the. We obtained written informed consent from the patients to publish their data.
The authors declare that there is no conf lict of interest.
XCC proposed the study and wrote the paper. All authors contributed to the design and interpretation of the study and to further drafts.
All the supplementary files in this paper are available at http://wjem.com.cn.
 World Journal of Emergency Medicine2022年3期
World Journal of Emergency Medicine2022年3期
- World Journal of Emergency Medicine的其它文章
- Mortality-related electrocardiogram indices in methanol toxicity
- The combination of creatine kinase-myocardial band isoenzyme and point-of-care cardiac troponin/contemporary cardiac troponin for the early diagnosis of acute myocardial infarction
- Increasing angiotensin-converting enzyme (ACE) 2/ACE axes ratio alleviates early pulmonary vascular remodeling in a porcine model of acute pulmonary embolism with cardiac arrest
- Traumatic tension pneumocephalus: A case report
- Blunt myocardial injury and gastrointestinal hemorrhage following Heimlich maneuver: A case report and literature review
- Successful treatment of a patient with diff use alveolar hemorrhage and anti-neutrophil cytoplasmic antibody-associated vasculitis
