Phalloplasty following penectomy for penile cancer
Wai Gin Lee *,A.Nim Christopher ,David J.Ralph
a University College London Hospital,London,United Kingdom
b St Peter’s Andrology,London,United Kingdom
KEYWORDS Humans;Male;Myocutaneous flap or transplantation;Penis or surgery;Phalloplasty;Reconstructive surgical procedures;Retrospective study;Surgical flap;Thigh or surgery;Treatment outcome;Urethra or surgery
Abstract Objective: Penile reconstruction or phalloplasty following penectomy can be offered where the functional penile length is inadequate for a man to void while standing or to have sexual intercourse.Phalloplasty is usually staged due to the complex surgical techniques required.This narrative review describes the technical concepts and summarises the contemporary outcomes following phalloplasty in this challenging cohort.Methods: A retrospective review of the English literature was performed between January 1946 till November 2021.The data were synthesised and complemented by the expert opinion of the authors with 20 years of experience in this field.The flaps are ideally designed with an integrated urethra or alternatively,a further free flap urethroplasty can be offered.Phalloplasty is further complicated following penectomy by scarring from the previous surgery and the potential loss of structures that would normally be present at the recipient site.Results: There are limited published data with a total of 19 men recorded in the literature.Only the radial artery forearm free flap and anterolateral thigh flap have been described in this cohort of patients.Functional outcomes including standing micturition,sensation in the neophallus,and the ability to orgasm are good.Overall quality of life and satisfaction was also good despite the high risk for long-term complications of the neophallus and donor site.Conclusion: Phalloplasty following penectomy requires microsurgical transfer of a free flap or a pedicled flap to reconstruct a neophallus.An erectile device is inserted at a later stage to facilitate sexual intercourse,if desired.Surgical scarring from penectomy and the potential loss of vasculature that would normally be present at the recipient site may further complicate reconstruction.Surgical and functional outcomes are acceptable based on the limited published experience to date.
1.Introduction
Penile reconstruction or phalloplasty is typically reserved for situations when all other options for reconstruction have failed or are inappropriate.For penile cancer,this situation arises following total penectomy or organ-sparing surgery where the functional penile length is inadequate for the man to void while standing or to have sexual intercourse.
Phalloplasty was first pioneered by Bogoraz N in 1936[1]using a tube pedicled abdominal graft and transplanted cartilage implant as a phallic stiffener.This first patient had suffered traumatic penile amputation but a subsequent case series of 16 men that included some men following penectomy for penile cancer was published in 1939 [2].
Penile reconstruction is complex and requires an understanding of the relevant anatomy and surgical techniques including microsurgical skills.Men should be referred to tertiary centres with the necessary expertise but even then,experience remains limited.Only one out of 316 men in a large study reporting the outcomes of phalloplasty had penile cancer [3].The aim of this narrative review is to briefly describe the technical concepts and surgical considerations for phalloplasty in this challenging cohort and to summarise,for the first time,contemporary experience and outcomes following phalloplasty.
2.Materials (patients) and methods
A MEDLINE (January 1946-November 2021) and Embase(January 1974-November 2021) library search (OVID Technologies Inc,New York,NY,USA) of the English language literature was performed to evaluate the current literature on phalloplasty following penectomy for penile cancer.The terms “penile neoplasms” AND “sex reassignment surgery”O(jiān)R“reconstructive surgical procedures”O(jiān)R“surgical flaps”were used as a MeSH subject heading search on the 1st of November 2021.The Emtree subject headings used were“penis cancer” AND “plastic surgery” OR “free tissue graft”.The terms“penile cancer”AND“phalloplasty”were used as truncated keyword searches.
Only articles pertaining to phalloplasty following partial,total or radical penectomy for penile cancer were summarised.Emphasis was placed on articles describing techniques for phalloplasty in this cohort but seminal articles that illustrate important technical considerations pertinent to the present cohort of patients were also included.The published data were supplemented by expert opinion from the authors’ cumulative experience of over 20 years in this field.
The most recent or complete study was included if patients appeared to be represented in multiple studies,as identified by author names,institution,year of publication,sample demographics and/or outcomes.
3.Goals of surgery
Phalloplasty aims to construct a neophallus following penectomy using a local or distant tissue flap.Distant flaps are transferred as a free flap using microsurgical techniques whereas pedicled flaps are transferred while maintaining their own blood supply.Currently,the most common flap used is the radial forearm free (RFF) flap.Other alternatives include the anterolateral thigh (ALT) flap,musculocutaneous latissimus dorsi(MLD)flap,and abdominal flap as summarised in Table 1 [4].
The ideal neophallus should be aesthetically pleasing and sensate (to both erogenous and tactile stimulus) while allowing voiding while standing and sexual intercourse.The ideal technique should achieve these goals in a single operation with minimal donor site morbidity.Disappointingly,no current technique satisfies all the above requirements [4].
4.Overview of surgical technique
Penile reconstruction is generally performed over 2 to 3 stages depending on the centre[5].The first stage involves creation of a neophallus with integrated urethra followed by microvascular transfer to the recipient site.Two surgical teams are usually required for a phalloplasty-one team raises the flap while the other prepares the recipient site.A glans is then fashioned at the same time or at a second stage (glansplasty).An erectile device can be inserted at least 3 months following the previous operation.
Table 2 summarises all the published papers describing contemporary free or pedicled flap phalloplasty following penectomy for penile cancer [6-10].There are only a single case series and several case reports published(between 1999 and 2014) with a total of 19 patients described.It is encouraging to note that all papers described free or pedicled flap phalloplasty with integrated urethra (the current preferred technique for phalloplasty).
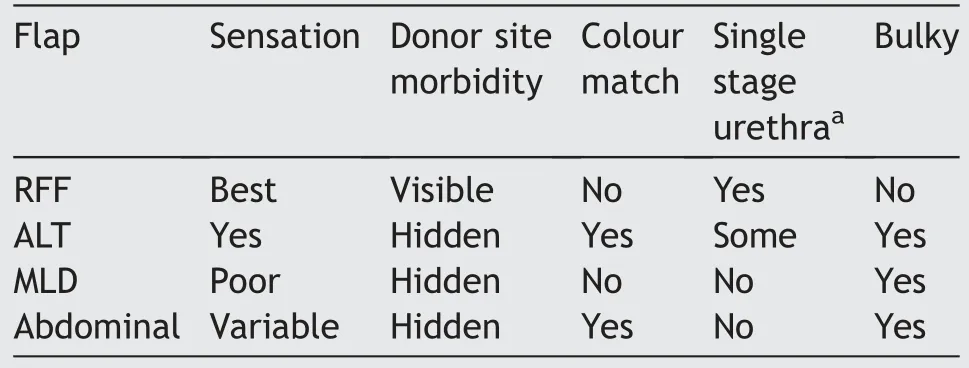
Table 1 Comparison of functional and aesthetic outcomes of commonly used flaps for phalloplasty.
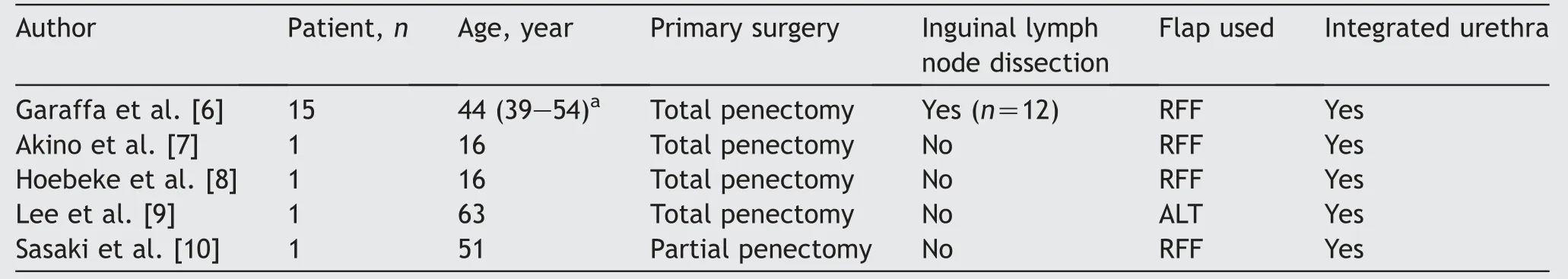
Table 2 Summary of papers reporting phalloplasty following penile cancer treatment.
4.1.Integrated urethra
Urethral reconstruction for phalloplasty was historically achieved by prelamination (grafted tissue tubed over a catheter and buried in a subcutaneous tunnel) or by skin tube urethra where both long edges are incised,undermined,and tubularised [11].These were sometimes performed over several stages.The advent of free flap phalloplasty by Chang and Hwang [12] allowed the urethra to be integrated in the flap design for the first time.The“tube-within-a-tube” design results in a well-vascularisedskin tube urethra that is made in a single stage within the neophallus.This technique reduced the rate of urethral complications within the neophallus from 75% to 43% in a large series of transgender patients [13].
4.2.RFF flap
The RFF flap is based on the radial artery while venous outflow is via the cephalic and basilic veins [6].The radial artery is anastomosed to the inferior epigastric artery via a groin incision while the veins are anastomosed to branches of the ipsilateral saphenous vein.A “tube-within-a-tube”urethra is integrated in the flap design and an anastomotic urethroplasty to the native urethra is typically performed with a covering suprapubic catheter and urethral stent.Tactile and erogenous sensation in almost 90%of patients is achieved by neurorrhaphy between the lateral antebrachial cutaneous nerves of the forearm with the dorsal penile nerves [6].
4.3.ALT flap
Alternatively,an ALT flap may be preferred for a more easily hidden donor site and greater flexibility in the length of the neophallus.The flap is supplied by perforators originating from the descending branch of the lateral circumflex femoral artery with sensation from the lateral femoral cutaneous nerve in up to 60% of men [9].
The ALT flap is a pedicled flap and does not require microvascular anastomosis thereby reducing the risk of arterial complications.Free flap microvascular transfer may be required if the vascular pedicle is not long enough(10% of cases).
In contrast to the RFF flap,the ALT flap is best suited for men with little subcutaneous fat because the distribution of fat is thicker around the thigh.The neophallus and integrated urethra can’t be tubularised if there is too much subcutaneous fat.If this is the case,the ALT flap can be combined with a less bulky free flap urethroplasty from another donor site either at the same time or a later date.
4.4.MLD flap
The MLD flap is well-described for transmasculine gender affirmation surgery [14,15].The flap results in a well-proportioned neophallus with the benefit of a relatively aesthetic donor site that can be better hidden than the RFF flap.The disadvantage is that the flap is poorly sensate [16] because it is supplied by the thoracodorsal neurovascular bundle.The urethra cannot be integrated into the flap design and therefore,has a poorer underlying blood supply.It has not been described for penile reconstruction following penectomy for penile cancer.
4.5.Abdominal flap
The abdominal flap(also known as suprapubic or pubic flap)is a pedicled flap raised from the lower anterior abdominal wall based on branches of the superficial epigastric artery.Venous drainage is via cutaneous veins and the superficial external pudendal vessels found at the base of the flap[17].The flap can be pre-expanded prior to phalloplasty to minimise the donor site scarring [18].
It is not a technically challenging flap but has limited tactile sensation (proximal phallus only) and no erogenous sensation.It may not be possible following penectomy if a pelvic lymph node dissection was performed.The flap must be combined with a free flap urethroplasty if the man wishes to void while standing.It has not been described for penile reconstruction following penectomy.
4.6.Free flap urethroplasty
Individuals who prefer an ALT or abdominal flap with no integrated urethra will require a free flap urethroplasty to void while standing [19].The radial artery urethroplasty was first described for urethral reconstruction in a patient following failed hypospadias repair [20].The flap can be based on either the radial artery or the ulnar artery[21,22],and is raised from the volar aspect of the forearm,which tends to be relatively hairless.The superficial circumflex iliac artery perforator flap has also been described for urethroplasty [23].
4.7.Insertion of erectile device
The decision to insert an erectile device should be made on a case-by-case basis.Penile prostheses have a high rate of complications that may directly compromise the neophallus(e.g.,severe infection leading to loss of neophallus) in some circumstances.Therefore,it should be considered only if specifically requested by the individual.In our experience,most men would normally request an erectile device if they have had penile cancer treatment.
If desired,inserting an erectile device can be challenging given the lack or loss of typical anatomical landmarks.A rear tip extender or malleable penile prosthesis can be placed in the crus of the penis(if preserved)at the time of phalloplasty to help identify the structures during subsequent penile prosthesis insertion.A penoscrotal incision is typically used and dilatation of the cylinder space within the neophallus is performed to size 18 Hegar dilator [24].The device is prepared as routine,but a polyethylene terephthalate (Intergard Silver Dacron?by Getinge,La Ciotat,France) cap is sutured to the cylinder tip to prevent migration within the neophallus (Fig.1).A Dacron?sock may be required following radical penectomy or if the residual corpora cavernosa or crura do not have adequate length to stabilise the cylinders.Proximal fixation of the device or Dacron?sock to the pubic bone would be required in a similar approach to transgender male patients.
The reservoir of the inflatable erectile device can usually be inserted in a similar fashion to a man with a native penis.Common options include the retropubic approach,high sub-muscular approach,or ectopic retroperitoneal approach [25].We recommend an individualised decision because each approach has advantages and disadvantages.An alternative to retropubic placement of the reservoir should be considered if the man has had a previous pelvic lymph node dissection.
Following successful placement,the device is kept partially inflated for a week to allow a capsule to form.Men are asked to refrain from sexual intercourse for at least 6-8 weeks to allow all wounds to fully heal.The median time to resumption of sexual activity was 3 (range 2-6) months [26].
5.Specific technical considerations following penectomy
There is limited published literature on penile reconstruction following surgical treatment for penile cancer.There is a single case series of 15 patients and several case reports as summarised in Table 2.As shown,only the RFF and ALT flaps have been described in this patient cohort.We therefore propose several important considerations when contemplating penile reconstruction following penectomy derived from our cumulative experience.
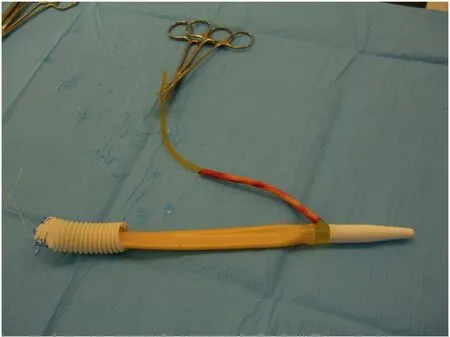
Figure 1 Single cylinder device prepared with Dacron?cap in place.
5.1.Surgical planning
Penile reconstruction in men following partial or total penectomy is further complicated by scarring from previous surgery and the potential loss of structures that would normally be present at the recipient site.Thorough and precise surgical planning is therefore required when considering penile reconstruction in this population similar to the approach in patients with exstrophy-epispadias complex [27].Ideally,the oncological surgeon who performed the penectomy should be consulted or their operation report reviewed.This is not always possible,and it is essential that the reconstructive urologist has the experience to manage unexpected intra-operative findings.
Anastomotic variations may be required when structures like the long saphenous vein and dorsal penile nerves are sacrificed during the primary surgery.Alternative venous anastomoses can be performed to the femoral vein,the venae comitantes of the inferior epigastric artery,or the dorsal penile vein,if present.Similarly,neurorrhaphy to the ilio-inguinal nerves or genital branch of the genitofemoral nerve may be required instead.
5.2.Timing of surgery
Timing of surgery is essential.Our centre recommends a minimum of 1-year recurrence-free survival before we consider penile reconstruction.Phalloplasty involves complex reconstruction,and it is not advisable to offer the surgery without an adequate period of follow-up.Single stage total penectomy followed by immediate RFF phalloplasty has been described but the patient subsequently developed nodules suspicious for distant tumour recurrence in the lungs at the time the manuscript was published [8].Delaying reconstruction by a year was successful in another 16-year-old male with no tumour recurrence after 7 years of follow-up [7].He did not suffer any persistent adverse psychological impact due to the delayed approach.
5.3.Perineal urethrostomy
A perineal urethrostomy will need to be reversed and rerouted to the orthotopic position if the man wishes to void while standing.There are several approaches that can be considered depending on the length of residual native urethra.
An indication of the residual urethral length may be found in the previous operative notes and by speaking to the oncological surgeon.In practice,the length of residual native urethra would usually need to be assessed intraoperatively.An adequate length of urethra to reach close to the suprapubic region can sometimes be found even following total penectomy.The length of the integrated urethra could then be adapted to bridge the rest of the gap and allow for anastomotic urethroplasty at the time of phalloplasty (preferred option).
Alternatively,the phallus urethra can be tunnelled to the perineum and spatulated adjacent to the perineal urethrostomy.A staged urethral join-up could then be offered with buccal mucosa graft augmentation urethroplasty.
An alternative approach has been proposed using a modification of the “urethral lengthening” principles used in transgender patients [9].The scrotum is divided along the midline and the defect resurfaced with a split-thickness skin graft.The urethral lengthening is then tubularised after 3 months with buccal mucosa augmentation.This is allowed to stabilise for a further 3 months before proceeding with ALT flap phalloplasty with integrated urethra.
6.Surgical and functional outcomes
There are little published data on phalloplasty following penectomy for penile cancer given the rarity of the condition and complexity of reconstruction using contemporary free or pedicled flap phalloplasty.Much expertise in phalloplasty has been adapted from the field of transmasculine gender affirmation surgery.Only one retrospective study has reported the outcomes of penile reconstruction following penile cancer (n=15) in addition to a handful of case reports [6].Outcomes from these publications are summarised in Table 3.
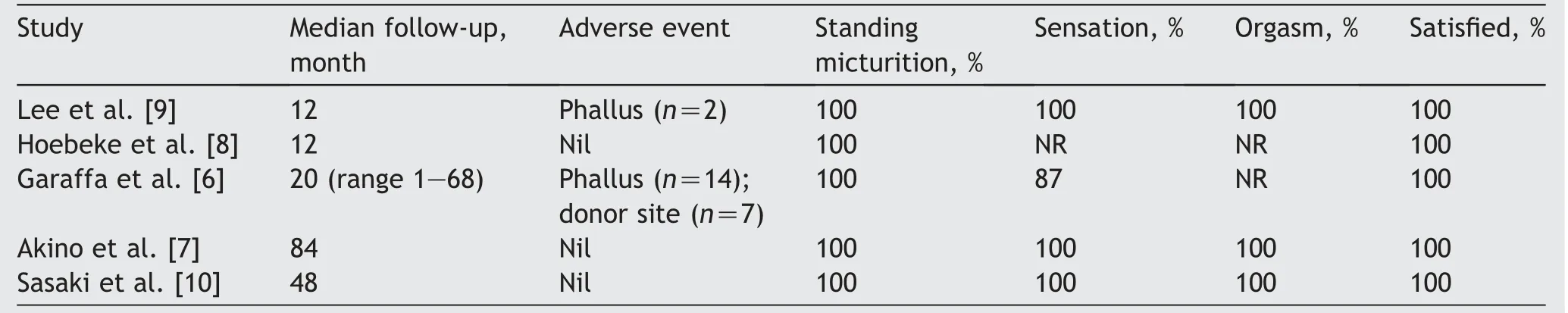
Table 3 Surgical and functional outcomes following phalloplasty for total penectomy.
In this case series,functional and cosmetic outcomes following RFF phalloplasty were excellent after a median(range) follow-up of 20 (1-68) months [6].All men were satisfied with the cosmesis and size of the neophallus(Figs.2 and 3)and 87%of men reported sensation.Five out of six men with a penile prosthesis could engage in sexual intercourse.
Having an erectile device improved the erectile function,orgasmic function,intercourse satisfaction,and overall satisfaction domains of the International Index of Erectile Function questionnaire [28] in men following phalloplasty [26].However,there was no difference in sexual quality of life or overall quality of life after an erectile device was inserted.However,we emphasise that this study primarily included men with exstrophy and congenital micropenis.A more comparable cohort for comparison would be men following penile trauma.Outcomes including quality of life,satisfaction with their health,and acceptance of their bodily appearance are poor in men following penile trauma probably because they previously had a normal penis that they could compare the neophallus with.

Figure 2 The neophallus deflated.

Figure 3 The neophallus inflated.
7.Complications
Long-term complications were common given the complexity of reconstruction in this group of patients [5].Urethral complications (strictures and fistulae) were themost common complication occurring in 47% of men.One man required explant of his penile prosthesis due to infection (14%).Donor site complications were relatively common with incomplete skin graft take (n=2),loss of sensation in the radial fossa (n=2),lymphoedema (n=1),and contracture of the forearm (n=2).
The risk of complications following phalloplasty is dependent not only on the type of tissue flap used but also the underlying anatomy of the recipient site.It is therefore misleading to compare different cohorts of patients following phalloplasty.Urethral complications are the most common and these would increase depending on the presence of a native,well-vascularised,bulbar urethral segment that would allow for anastomotic urethroplasty in addition to other factors like the type of neourethra construction.Systematic reviews comparing complication rates between these two cohorts of patients(transgender or nonbinary patients and patients following penectomy) should be interpreted with caution [29,30].
8.Conclusion
Phalloplasty following penectomy for penile cancer is a challenging endeavour that requires several surgical stages.Both microsurgical free flaps and pedicled flaps should be offered for penile reconstruction,but it is important to individualise the choice depending on the requirements of the patient.An erectile device is usually required for sexual intercourse.Men report good satisfaction and quality of life following phalloplasty despite the significant risk of complications.
Author contributions
Study concept and design: David J.Ralph.
Data acquisition: Wai Gin Lee,A.Nim Christopher.Data analysis: Wai Gin Lee.
Drafting of manuscript: Wai Gin Lee.
Critical revision of the manuscript: Wai Gin Lee,A.Nim Christopher,David J.Ralph.
Conflicts of interest
The authors declare no conflict of interest.
 Asian Journal of Urology2022年4期
Asian Journal of Urology2022年4期
- Asian Journal of Urology的其它文章
- The first Japanese case of intraductal cancer of the prostate with checkpoint kinase 2 mutation
- The relationship between sexually transmitted microorganisms and seminal quality in asymptomatic men
- Validation of Vesical Imaging Reporting and Data System score for the diagnosis of muscle-invasive bladder cancer: A prospective cross-sectional study
- Extramammary Paget’s disease: Updates in the workup and management
- Genitourinary manifestations of Lynch syndrome in the urological practice
- Multidisciplinary management of patients diagnosed with von Hippel-Lindau disease:A practical review of the literature for clinicians
