Efficacy of custom-made soft keratoconus lenses on corneal aberrations and photic phenomena in patients with keratoconus: a corneal topography imaging based study
Aysegul Penbe, Hatice Selen Kanar, Aysu Karatay Arsan, Sevda Aydn Kurna
1Department of Ophthalmology, Kartal Dr. Lutfi Kirdar Training and Research Hospital, Health Science University,Semsi Denizer Caddesi, E‐5, Kartal Istanbul 34890, Turkey
2Department of Ophthalmology, Fatih Sultan Mehmet Training and Research Hospital, Health Science University, E‐5,Icerenkoy 34752, Istanbul, Turkey
Abstract
● KEYWORDS: corneal aberrations; custom-made soft keratoconus lenses; higher-order aberrations; keratoconus;lower-order aberrations; pupillography
INTRODUCTION
Keratoconus (KC) is a bilateral, asymmetric corneal ectasia characterized by progressive corneal thinning and decreased biomechanical strength of the cornea on a multifactorial etiological basis[1]. For a perfect visual rehabilitation in patients with KC, it is necessary to treat higher‐order aberrations (HOAs) that cannot be eliminated by routine treatments[2].
In patients with mild KC, spectacles or traditional soft contact lenses (CLs) might correct myopia and regular astigmatism[3].However, elevated levels of both lower and HOAs in KC make it difficult to achieve better visual performance with traditional soft CLs or spectacles in moderate and advanced cases[4]. As the disease progress, rigid gas permeable (RGP)CLs become the “gold standard” method of non‐surgical visual rehabilitation as RGP CLs masks the aberrations by forming a regular and smooth optical surface[5]. However, several studies showed that residual HOAs persist even with RGP CLs on‐eye, which are typically attributed to the posterior corneal surface[6‐7]. In recent years, the custom‐made soft keratoconus lenses (CSKLs) have been proposed as a practical and comfortable solution for correcting ocular HOAs in eyes with irregular corneas[8‐10].
HydroCone or Toris K lenses are specially designed soft silicone hydrogel toric lenses for KC, with front toric surface and spherical back optic zones. The higher oxygen permeability and modulus of rigidity of these silicone hydrogel CLs make them more suitable for KC corrections than conventional soft CLs[11‐12]. The custom‐made soft toric lenses may offer better visual performance with a good ocular comfort level by covering the anterior corneal irregularities and correcting the anterior corneal surface HOAs[13].It is known that pupil diameter affects ocular aberrations which in turn affects the luminance and sharpness of the retinal image[14]. In KC patients, the retinal image becomes brighter with increasing pupil dilation; on the other hand, wavefront aberrations tend to increase, leading to a deterioration in visual quality[15]. For specially designed and custom‐made soft toric lenses, pupil diameter should also be evaluated when treating ocular aberrations.
In this study, we aim to evaluate the efficiency of Toris K CSKLs in the visual rehabilitation of eyes with KC by investigating corneal aberrations in different optical zones and subjective photic phenomena at different pupil diameters.
SUBJECTS AND METHODS
Ethical ApprovalThe study protocol adhered to the tenets of the Declaration of Helsinki for clinical research and was approved by the Ethical Committee of Kartal Dr. Lutfu Kirdar Training and Research Hospital (No.514‐192‐38). Written informed consent was obtained from all of the patients after explaining the purpose and possible consequences of the study.
Patient RecruitmentPatients with KC, who were not satisfied with their vision and were fitted with soft Toris K CSKLs,were enrolled in the study between October 2019 and February 2020. All participants had undergone corneal collagen cross‐linking (CCXL) surgery at least 24mo ago. KC was classified into 4 severity levels according to the criteria of the ABCD grading system, based on corneal parameters determined with the Sirius topography device (CSO, Firenze, Italy).Participants in stages 1, 2, and 3 were included in the study,except for stage 4, because the degree of irregular astigmatism in stage 4 is so high that sufficient visual improvement cannot be achieved with soft KC lenses[16].
All participants underwent a standardized ophthalmic examination, including refraction measurements as spherical,cylindrical and spherical equivalent (SE) in diopters, high‐contrast uncorrected visual acuity (UCVA), high‐contrast best spectacle‐corrected visual acuity (BSCVA), and contact lens‐corrected visual acuity (CLCVA) in decimal values with Snellen at 5 meters using a Topcon ACP‐8 chart projector(Topcon Corporation, Tokyo, Japan). The UCVA, BSCVA, andCLCVA were transformed to the logarithm of the minimum angle of resolution (logMAR) for statistical analyzes.
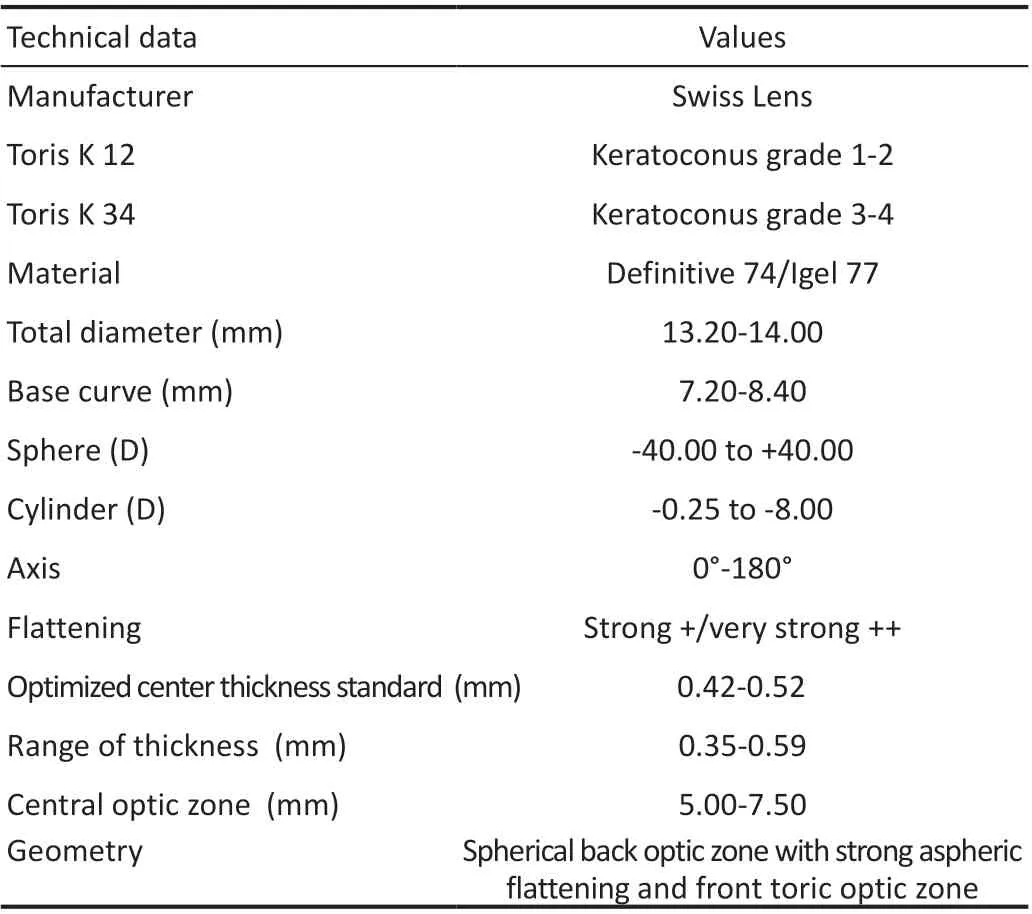
Table 1 The fitting set parameters of Toris K-HydroCone lens
Exclusion criteria included the presence of ocular surgery other than CCXL, history of ocular trauma, ocular disease (e.g.,corneal dystrophies, severe dry eye, active ocular infections,glaucoma, cataracts, retinal and choroidal pathologies),or systemic diseases such as diabetes or hypertension. In addition, participants with extensive corneal scarring due to the inadequate optical effect of soft CLs were also excluded if the cornea was unclear. Participants who had undergone CCXL surgery less than 24mo ago were excluded from the study due to the ongoing corneal remodeling process. History of using CLs or spectacles for refractive correction and time interval between CCXL surgery and contact lens fitting was recorded.
Contact Lens Fitting AssessmentToris K‐HydroCone soft contact lens (SwissLens, Prilly, Switzerland) is a custom‐made silicone hydrogel lens with toric anterior and spherical posterior surfaces that provides good stabilization and comfort thanks to the dynamic stabilization system. The technical parameters of the lens set were described in Table 1.
The first lens was selected as HydroCone 12 if the keratometry>6.8 mm or KC grade 1 or 2, and HydroCone 34 if the keratometry <6.8 or KC grade 3 or 4. Then 0.6 mm was added to the average K value of the auto refractometer to select a trial lens. The first lens was used to validate the base curve and overall diameter. The stabilization marks at 0 and 180 degrees were evaluated to measure the stabilization axis. Subsequently,the lens characteristics of eye movement, rotation, centration,and comfort were observed after 30min of wear. When the optimal fit was achieved, over‐refraction was performed with prescription spectacles. The endpoint of refraction was defined as the maximum “plus” sphero‐cylindrical refraction that allowed the patient to read his threshold letters on the Snellen acuity chart. Once the endpoint of over‐refraction was reached,the vertex distance was recorded in millimeters and converted according to the scheme for the final prescribed lens.
After fitting the prescribed lens, a biomicroscopic evaluation was performed with a slit lamp to ensure that the manufactured lens was well positioned in terms of lens centration (horizontal and vertical), movement (with the push‐up test, in the primary position, upon up‐gaze, and with a horizontal lag), and toric marker alignment. In all cases, the ideal rotation of the lens was equal to or less than 5°.
Finally, each patient received detailed information on lens cleaning, wetting, and disinfection with standard soft lens solutions. Participants received detailed information on possible adverse events and details on emergency communication.
Corneal Curvature, Wavefront, and Pupillography AnalysisAll participants were examined at baseline and 4wk after the prescription lens was manufactured. Corneal measurements were performed by the same experienced operator in the scotopic environment using Sirius topography (CSO Inc.,Firenze, Italy), which uses a combination of a 3D Scheimpflug camera and a Placido disk[17]. Measurements of corneal curvature with apical zone keratometry (Kapex), and flat keratometry (SimK1) and steep keratometry (SimK2) scores,anterior and posterior corneal curvature and the thinnest corneal thickness were obtained from a pupil area of 3 mm.HOAs were obtained by converting the corneal elevation profiles to wavefront data using Zernike polynomials (Zernike 3‐7). The posterior corneal wavefront measurements are not affected by contact lens fitting, only the anterior corneal aberrations coefficients were evaluated. The anterior corneal lower‐order corneal aberrations (LOAs), HOAs, spherical,coma, trefoil, quadrifoil, spherical, and residual aberrations,and optical path difference (OPD) coefficients in root mean square (RMS) values were recorded. The point spread function(PSF) images were analyzed using the Sirius wavefront analysis system, which provides the image of a point‐like object including the effects of all aberrations in an optical system[18].
All corneal wavefront aberration parameters were measured and compared before and after fitting the Toris K lens,which was manufactured in 6.5 mm. Wavefront analyzes were evaluated in two different selected pupil/optical zones;the central 4.5 mm and the peripheral 7 mm, which were outside the optical zone of the contact lens. To investigate the distribution characteristics of the aberrations from the center to the peripheral zones with CSKLs, the corneal wavefront parameters were also compared between the two optical zones.Pupil size was assessed under mesopic conditions using a specific anterior segment camera‐based pupillography modefrom Sirius topography[19]. Those who had a pupil size less than 6 mm were evaluated in subgroup 1, while the other participants with a pupil size greater than/equal to 6 mm were evaluated in subgroup 2.
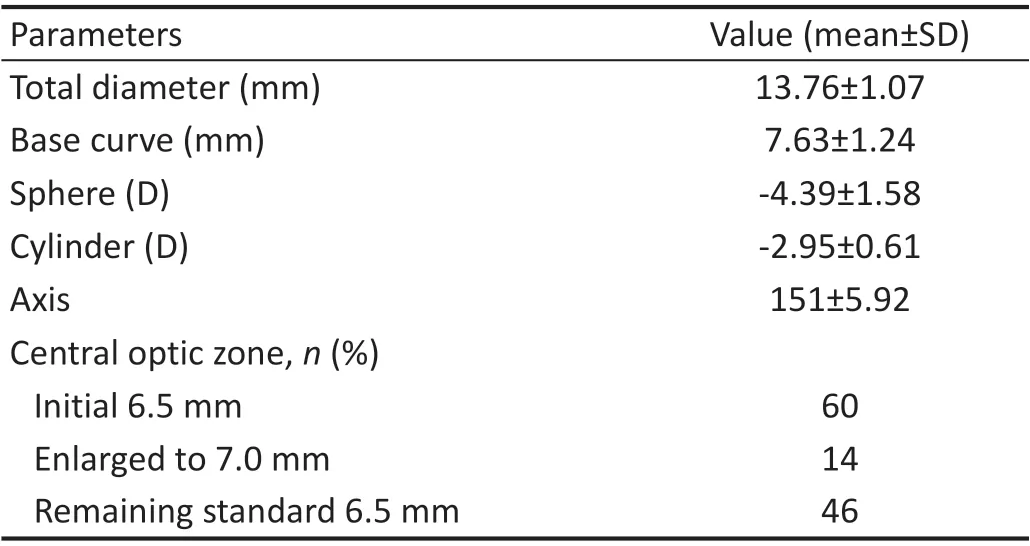
Table 2 The parameters of the Toris K lenses fitted
The presence of subjective photic phenomena such as halo,flare, flash, or glare was investigated using a modified questionnaire based on one published by Arnold[20]. In cases where any type of photic phenomena was reported with moderate or severe values, the CLs were recorded, and the optical zone was increased from a standard value of 6.50 to 7.00 mm. After wearing the new CSKL with an enlarged optical zone, the decrease in photic phenomena was rechecked.Statistical Analysis Statistical analysis was performed using the SPSS software version 21 (SPSS Inc., Chicago, IL, USA).Data distribution was tested using the Kolmogorov‐Smirnov test. A paired samplet‐test was performed to compare the difference in the means “before” and “after” fitting the lens.The significance level of theP‐value was accepted as 0.05(P≤0.05).
RESULTS
Sixty eyes of 42 KC patients (26 men and 16 women) with a mean age of 21±4.35 (range: 18‐47)y were examined. The mean time interval between CCXL surgery and soft contact lens fitting was 38.2±18.31 (range: 24‐178)mo. According to the ABCD KC grading system, the 26 eyes were in stage 1, 23 eyes were in stage 2, and the remaining 11 eyes were in stage 3. The mean values of the fitted CSKL parameters are shown in Table 2.
Forty‐five (75%) eyes in the study group had no history of contact lens wear, while 17 (28.3%) eyes had been using spectacles and 28 (46.7%) eyes had no history of vision correction instruments. The 15 (25%) eyes of the participants had tried at least one type of CLs and had stopped using the lenses due to various complaints. Eleven (18.3%) of them had experience with RGP lenses and suffered from discomfort and/or excessive mobility on the ocular surface, while 4 (6.7%)eyes had worn hybrid lenses but also complained of redness and difficulty in removing the lenses at the end of the day.

Figure 1 An example of corneal wavefront changes with Toris K lens in 4.50 mm selected optical zone A: The maps of OPD, HOAs, and Zernike expansions before Toris K lens fitting; B: The maps of OPD, HOAs, and Zernike expansions after Toris K lens fitting; C: The maps of astigmatism,coma, spherical and residual aberrations before Toris K lens fitting; D: The maps of astigmatism, coma, spherical and residual aberrations after Toris K lens fitting. Most of the aberration scores were decreased after contact lens fitting in 4.5 mm optical zone. HOAs: High order aberrations;OPD: Optic path difference; RMS: Root mean square.
Refraction and Visual Acuity ChangesBefore CSKL fitting, the mean high‐contrast UCVA was 0.71±0.23 (range:1.2‐0.5) logMAR and the mean high‐contrast BSCVA was 0.54±0.18 (range: 1.0‐0.4) logMAR. With CSKLs, all eyes achieved significant recovery of visual acuity. After CSKL fitting, the mean CLCVA was 0.21±0.11 (range: 0.5‐0.0)logMAR (P<0.0001). Eighteen (42.8%) eyes achieved a CLCVA of 0.10 logMAR or less and 37 (88.1%) eyes achieved a CLCVA of ≤0.30 logMAR. However, only 5 patients remained below 20/40, but they had at least 4 lines of improvement. The initial mean SE, manifest cylindric and spheric diopters, Kapex, SimK1 and SimK2 scores with anterior and posterior curvature in 3 mm diameter on Sirius corneal topography were significantly decreased after CSKL fitting. Table 3 shows the changes in refractive and topographic parameters before and after CSKL fitting. Except for posterior corneal curvature values, all corneal curvature and refraction values decreased significantly after CSKL fitting.
Corneal Wavefront Aberrations ResultsAccording to the 7th‐order Zernike expansion scale, all mean corneal aberration coefficients, including LOAs (1stto 2ndorder)and HOAs RMS (3rdto 7thorder) in the central optical zone of 4.5 mm were significantly reduced after CSKL fitting(P=0.000; Figure 1, Table 4) The mean values for LOAs,trefoil, and quatrefoil RMS were also significantly reduced in the peripheral optical zone of 7.00 mm after CSKL fitting.(P=0.000; Figure 2, Table 4) The mean coma RMS values in 7.00 mm were also reduced after CSKL fitting, but the difference was not statistically significant (P=0.676). On the other hand, the mean values of HOA, OPD, spherical aberrations, and the residual coefficients of RMS showed a statistically significant increase in the optical zones of 7.00 mm. The mean PSF Strehl ratio score increased significantly in both the 4.5 and 7 mm optical zones after CSKL fitting (Table 4, Figure 3).
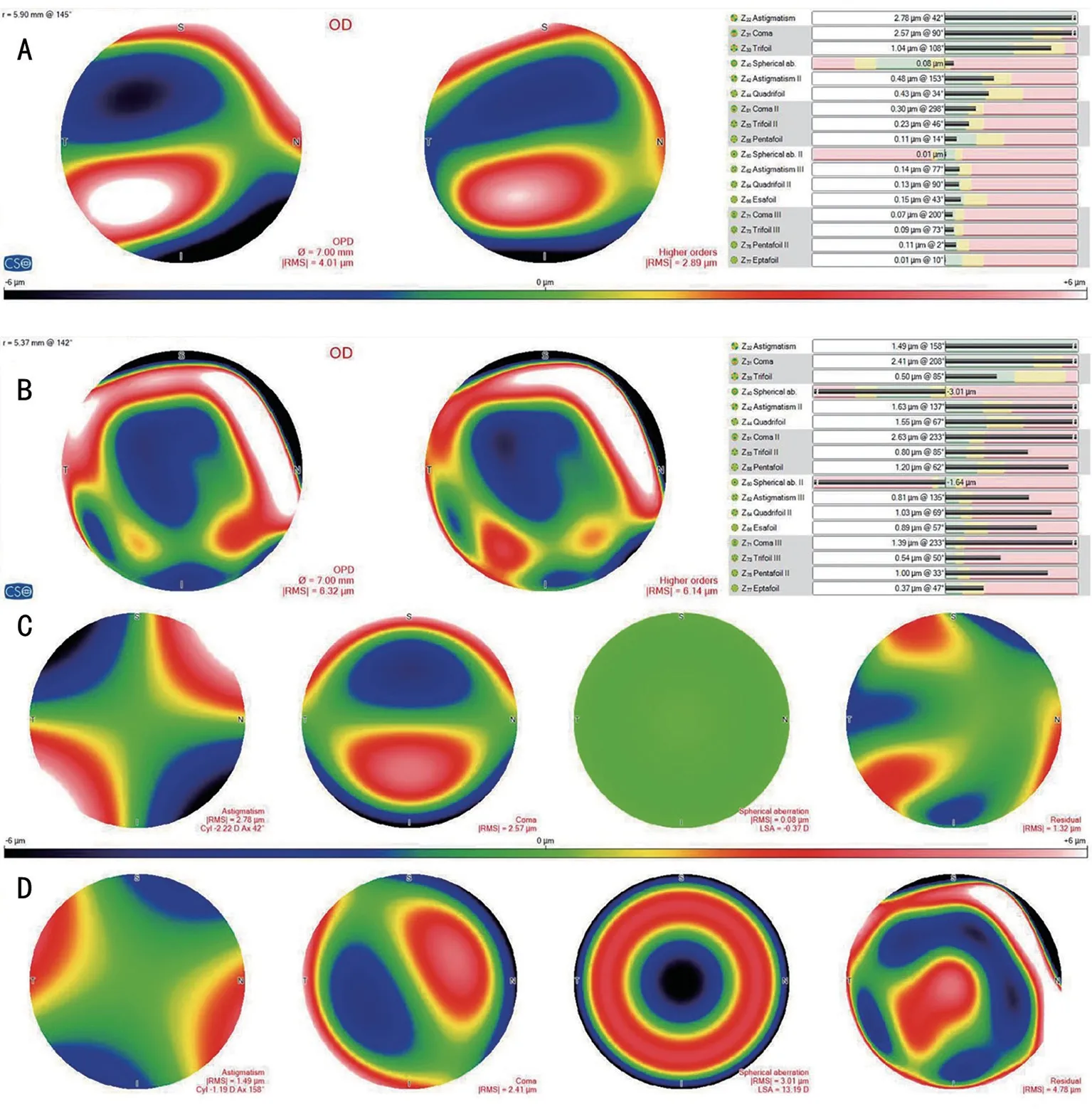
Figure 2 An example of corneal wavefront changes displays with Toris K lens in 7.00 mm selected optical zone A: The maps of OPD, HOAs,and Zernike expansions before Toris K lens fitting; B: The maps of OPD, HOAs, and Zernike expansions after Toris K lens fitting; C: The maps of astigmatism, coma, spherical and residual aberrations before Toris K lens fitting; D: The maps of astigmatism, coma, spherical and residual aberrations after Toris K lens fitting. Most of the aberration scores were elevated after contact lens fitting in 7 mm optical zone. HOAs: High order aberrations; OPD: Optic path difference; RMS: Root mean square.
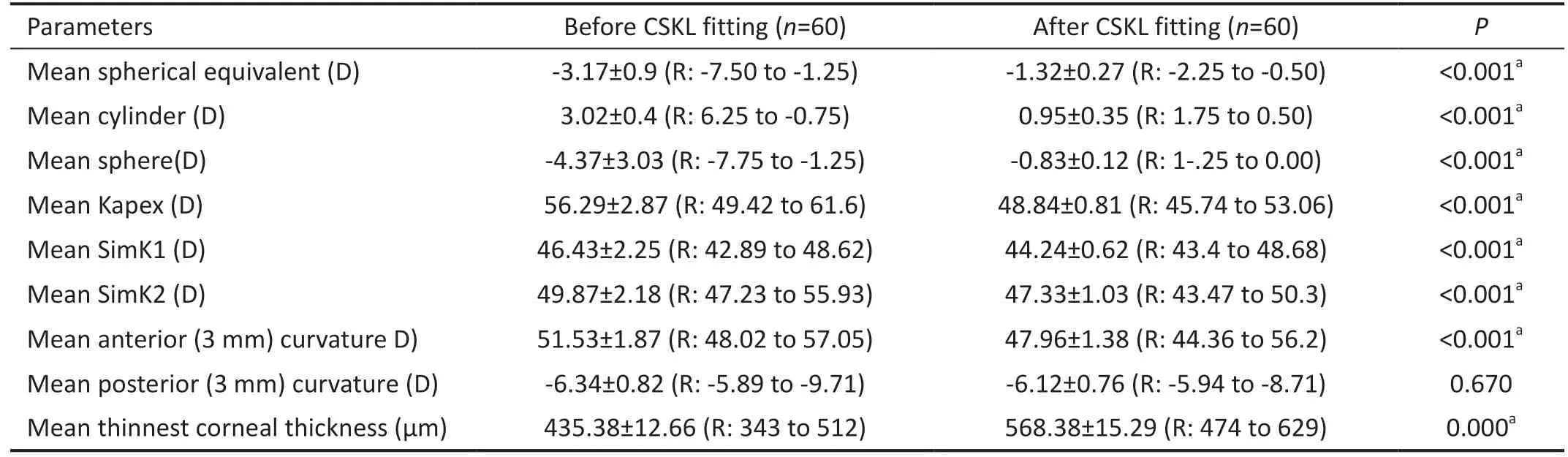
Table 3 The refractive and corneal curvature changes after CSKL fitting mean±SD
Comparison of wavefront analyzes of the central 4.5 mm and peripheral 7.00 mm corneal zones in patients with KC while wearing CSKL showed that all low and high order Zernike scale parameters were significantly increased in the 7.00 optical zone compared to the 4.5 mm zone (P<0.0001).
Pupillography Based Photic Phenomenon Subgroup AnalyzesThe mean mesopic pupil size of the study group was 4.59±1.06 mm (range: 3.61‐7.38 mm). In 35 (83.3%) patients,the pupil diameter was less than 6 mm (subgroup 1), and in theremaining 7 (16.7%) patients, a pupil size of 6 mm or more was measured (subgroup 2). The rate of subjective photic phenomena was significantly higher in subgroup 2 (6/85.7%)than in subgroup 1 (8/22.85%,P=0.000). In all 14 patients who reported photic phenomena, the optical zone of the lenses was widened to 7.00 mm and re‐prescribed. In addition to the decrease in photic phenomena to 20.00% (n=7) from 22.85%(n=8) in subgroup 1, there was a significant decrease in visual complaints in all 6 patients in subgroup 2.
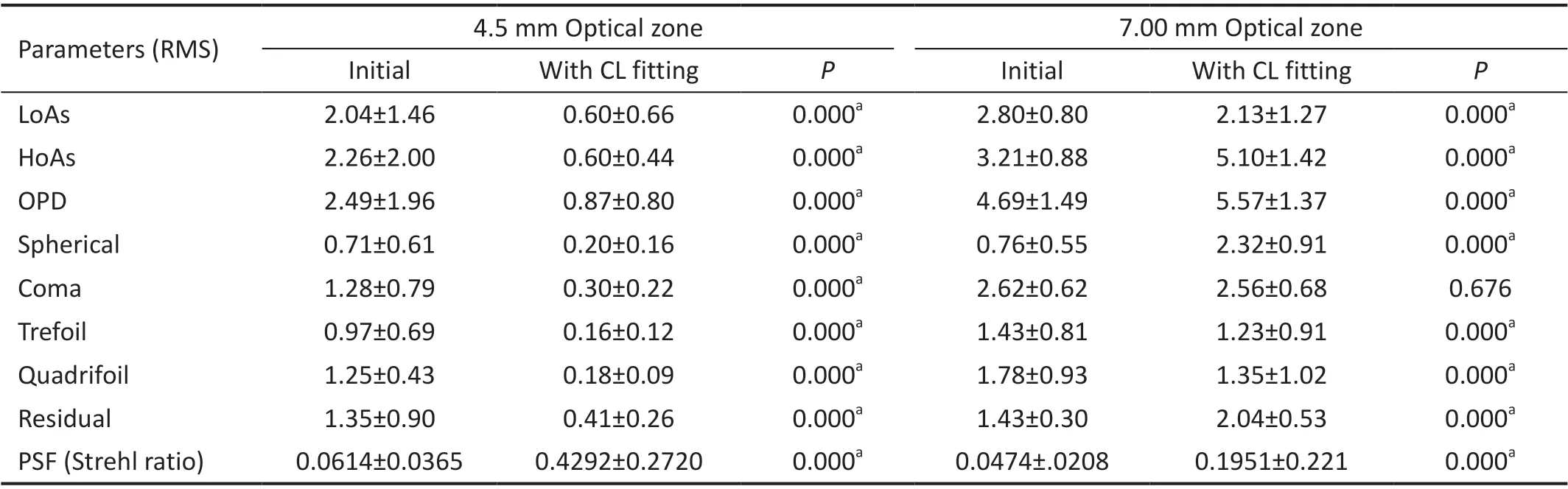
Table 4 The comparison of corneal wavefront coefficients before and after CSKL fitting mean±SD
DISCUSSION
In this study, we investigated the visual and aberrometric changes in the central and peripheral corneal optical zones after CSKL fitting in patients with KC. Our results suggest that CSKL fitting improved visual acuity in the majority of our study population by controlling HOAs in the central optical zones. Several studies have shown that soft CLs can be beneficial in correcting HOAs in severely aberrated eyes and provide visual benefits over their use in normal eyes[8,21‐22]. To our knowledge, this is the first study to investigate the role of pupil size on the occurrence of photic discomfort rates with CSKL in KC patients.
In patients with KC, CSKLs have been reported to provide good visual acuity under laboratory conditions with high contrast sensitivity consistent with habitual RGP corrections[23].Gumus and Kahraman[21]reported a mean increase in visual acuity of 4.5 lines (range 1‐9 lines) with Toris K lenses.The results of the current study show that the logMAR achieved with Toris K CSKLs was quite satisfactory with an improvement of at least 3 lines in patients with KC.Furthermore, there were notable reductions in spherical,cylindrical, and keratometric values (SimK1, SimK2, Kapex)when measured with the CSKLs. In contrast, as expected,there were no significant differences in posterior corneal keratometry values. The clinical performance of KeraSoft?IC(Bausch &Lomb, Filcon V3 material), the other commonly manufactured soft CLs for irregular corneas, was found to be effective in the high contrast visual acuity values, similar to the results of Toris K[24].
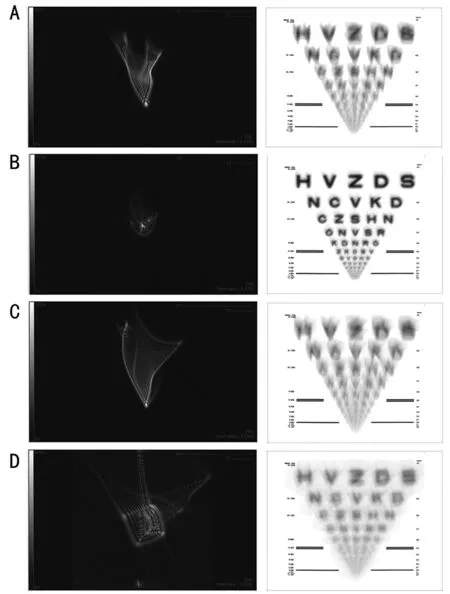
Figure 3 An example of a PSF and display of the vision scale displays with Toris K lens in 7.00 mm selected optical zone A: Before Toris K lens fitting in 4.5 mm optical zone; B: After Toris K lens fitting in 4.5 mm optical zone; C: Before Toris K lens fitting in 7.00 mm optical zone; D: After Toris K lens fitting in 7 mm optical zone. The improvement in PSF scores after CL fittingwas more significant in central 4.5 mm optical zone. PSF: Point spread function.
Wavefront aberrations produced by the cornea are a good indicator of visual quality in normal and keratoconic eyes and for early detection of KC[25]. Although topographic systems cannot measure the wavefront directly, they can estimate corneal aberrations from corneal steepening in ectatic areas that result in a deviation of rays projected onto the retina and a deformed wavefront[26].
In eyes with KC, the increase in anterior HOA, especially in coma, is caused by the irregular steepening and protrusion of the anterior corneal surface, which can be detected with high reliability by camera‐based Scheimpflug topography systems[27]. However, even with RGP lenses, residual HOAs remain on the eye, typically attributed to the posterior corneal surface[7]. Fitting a CSKL to correct LOAs (defocus sphere and astigmatism) has been shown to be very effective in reducing HOAs in eyes with KC, suggesting that soft CLs may additionally mask HOAs by maintaining a uniform anterior surface depending on their thickness. Therefore, in recent years, technology has been introduced to control both LOAs and HOAs with a custom wavefront‐controlled soft contact lens modality. In the study by Marsacket al[23]the full wavefront customized hydrogel lenses, which aim to neutralize all corneal aberrations, were compared to the habitual RGP CLs and they found that the novel wavefront hydrogel lenses were comparable to the RGP CLs in both measurements.However, a comparison of the visual benefits of the wavefront customized hydrogel lenses with the other (non‐wavefront guided) CSKLs such as Toris K has not yet been investigated.Our study showed that the variation in corneal wavefront analyzes depended on the size of the selected optical zone diameters. The central optical zone of 4.5 mm selected for corneal wavefront analysis is the diameter closest to the mean pupil size of the study group (4.59 mm) and is therefore considered clinically more important for visual quality,corresponding to the larger alternatives. All anterior corneal wavefront values showed improvement in the central area of 4.5 mm along with a significant visual recovery in our patients,despite increased peripheral aberrations at 7.00 mm.
The improvements in anterior corneal aberrations achieved with CSKL fitting were quite remarkable and comparable to previous studies[8,21,24]. At 4.5 mm, all corneal aberrations,including LOAs and HOAs, showed significant reductions.In contrast, when the selected optical zone was enlarged to 7.00 mm, HOAs, especially spherical coefficients, were significantly increased compared to baseline values, although values for other peripheral aberrations such as trefoil and quatrefoil RMS decreased. The circular and regular pattern of the edge of the optic zone in the mid‐periphery of the cornea could lead to an increase in spherical aberrations, but also to a deterioration in the patterns of other peripheral aberrations such as trefoil and quatrefoil, leading to a decrease in RMS values. The LOAs coefficients that depended on the spherical‐cylindrical errors decreased in the 7 mm zone as much as in the 4.5 mm zone. The main reason for these incongruent patterns of change in HOAs during CSKL fitting was that the 7.00 mm selected optical zone was further outside the 6.5 mm boundary of the standard optical zone of the manufactured CSKL.Vertical coma is usually significantly increased in eyes with KC, which depends on the distortion of light waves arriving at the (flatter) superior and (steeper) inferior corneas[28]. Our results showed that the improvements in mean coma with CSKLs in 4.5 mm were quite remarkable (from 1.28 to 0.30 RMS);however, the changes in coma aberration in the optical zone of 7.00 mm were not significant. The keratoconic cone apex distorts incoming light waves by ‘‘rotating’’ them and inducing trefoil (or triangular astigmatic) aberrations[29]. After CSKL fitting procedure, the mean trefoil RMS value of the study group showed significant regression in both 4.5 and 7.00 mm.In this regard, the subjective photic phenomena were reported more frequently in subgroup 2 with pupil diameter greater than 6.00 mm (85.7%) than in subgroup 1 with pupil size less than 6 mm (22.85%). As a solution, it was considered to increase the diameters of the optical zone to reduce the effects of aberrations originating from the optical edge of the present lens, and the optical zone was re‐ordered as 7.00 mm instead of the 6.50 mm standards. With the new manufactured lens, photic complaints were regressed in all 6 patients in subgroup 2.However, there was no obvious change in photic phenomena in 7 of 8 patients in subgroup 1. This is because the pupil size of these patients was already smaller than the original optical size of the CSKL. Our results suggest that the use of the standard 6.5 optical zones in patients with larger pupil diameters causes an extremely high incidence of photic phenomena. Therefore,it is reasonable to include pupillography measurements in the initial Toris K fitting examination for patients with a mesopic pupil larger than 6 mm and to increase the optical zone to 7.00 mm to prevent photic phenomena.
The current study has some limitations. Our sample size is relatively small. We did not assess contrast sensitivity, and the presence of halo and glare was not performed with an objective, device‐based method. In addition, subgroup analyzes of KC stages were not evaluated to avoid review of overdose data in the same study.
In conclusion, the current study demonstrated that the increased LOAs and HOAs in eyes with KC can be rehabilitated with Toris K CSKLs within the limits of the optic zone of the lens.CSKLs provide good visual benefits and should therefore be considered as an alternative to conventional RGP lenses.In addition, patients’ pupil size should be considered when determining the diameter of the Toris K lens optical zone to control the subjective photic phenomenon as it affects ocular aberrations and visual quality.
ACKNOWLEDGEMENTS
Conflicts of Interest: Penbe A, None;Kanar HS, None;Arsan AK, None;Kurna SA, None.
 International Journal of Ophthalmology2023年1期
International Journal of Ophthalmology2023年1期
- International Journal of Ophthalmology的其它文章
- Instructions for Authors
- Morphological and functional changes in the macular area in diabetic macular edema after a single intravitreal injection of aflibercept
- Macular vascularisation changes analysed using OCT angiography after successful rhegmatogenous retinal detachment repair
- Comparison of success rate and intraocular pressure spikes between selective laser trabeculoplasty and micropulse laser trabeculoplasty in African American and Hispanic patients
- Clinical observation of recombinant human nerve growth factor in the treatment of neurotrophic keratitis
- Destructive effects on endothelial cells of grafts in cytomegalovirus DNA-positive patients after keratoplasty
