Morphological and functional changes in the macular area in diabetic macular edema after a single intravitreal injection of aflibercept
Chuan-He Zhang, Bin Gong, Chao Huang, Xiang-Wen Shu, Tian-Yu Chen, Xuan Chen,Chang-Long Wu, Yu Wang
1Shenzhen Aier Eye Hospital, Aier Eye Hospital, Jinan University, Shenzhen 518031, Guangdong Province, China
2Department of Ophthalmology, Jinan Second People’s Hospital, Jinan 250001, Shandong Province, China
3Medical Department, Wuxi Second People’s Hospital, Wuxi 214001, Jiangsu Province, China
Abstract
● KEYWORDS: aflibercept; best corrected visual acuity;diabetic macular edema; foveal retinal thickness; mean light sensitivity
INTRODUCTION
Diabetic macular edema (DME) is usually defined as retinal thickening within the two optic disk diameters of the central fovea close to macula; it belongs to the category of diabetic retinopathy (DR) and is one of the leading causes of blindness in patients with diabetes[1‐2]. Diabetic patients with elevated blood glucose lead to retinal microvascular damage, and finally lead to retinal ischemia and hypoxia and activate the inflammatory pathway by releasing a variety of cytokines such as vascular endothelial growth factor (VEGF),interleukin 6 and so on[3]. In DME, the loss and dysfunction of capillary pericytes lead to the destruction of the inner blood‐retinal barrier, resulting in intra‐retinal leakage of fluid, protein and lipids[4]. These changes lead to the progressive thickening of the retina and the painless decrease of vision. Although reversible in early stages, longstanding macular edema can lead to ischemia and atrophy of the retinal photoreceptors and retinal epithelium. If the lesion involves the macular fovea, it may lead to permanent vision loss[5‐6].
As a traditional treatment of DME, laser therapy can effectively reduce edema, but it has a weak effect on the recovery of visual function[7]. Several studies have found that VEGF plays a key role in the development of DME. The activation of VEGF can increase retinal vascular permeability,leading to vascular leakage and neovascularization. At present,the intravitreal injection of anti‐VEGF drugs has become the first‐line treatment for DME. Aflibercept, as a fusion protein anti‐VEGF drug, can bind to not only VEGF‐A but also placental growth factor; also, it can improve the function of blood‐retinal barrier and reduce macular edema[8‐9]. In this study, optical coherence tomography angiography (OCTA)and MP‐3 microperimetry were used to analyze the structural characteristics and functional changes of the macular area in patients with DME after a single injection of anti‐VEGF drugs,and to explore their clinical significance.
SUBJECTS AND METHODS
Ethical ApprovalThis prospective study was performed from March to July 2021 at Jinan Second People’s Hospital and approved by the Ethics Committee of Jinan Second People’s Hospital (No.20201203). The study abided by the Declaration of Helsinki, and all patients signed informed consents.
SubjectsThe inclusion criteria were as follows: 1) Adult patients with type 2 diabetes, blood pressure less than 150/90 mm Hg, fasting blood glucose <8.0 mmol/L, and blood glucose <10.0 mmol/L; 2) Patients with untreated DME, or patients who had not received intravitreal injection therapy and pan retinal photocoagulation therapy within 6mo before this treatment; 3) Optical coherence tomography (OCT)examination confirming macular edema and central retinal thickness (CRT) ≥250 μm; 4) No hemorrhage, proliferation,traction retinal detachment, and other vitreous surgery indications.
The exclusion criteria were as follows: 1) History of ocular trauma and other fundus diseases; 2) Severe cataract affecting the fundus examination; 3) Patients with DME who had received intravitreal or peribulbar injection of glucocorticoids;4) Patients with thromboembolism and coagulation dysfunction, currently taking anticoagulant drugs (except aspirin) or having other serious systemic diseases; 5) Pregnant or lactating women.
Treatment MethodAll patients received levofloxacin eye drops four times a day for the first 3d of treatment. Intravitreal injections were performed in the operating room. The conjunctival sac was disinfected with 5 g/L povidone‐iodine solution and washed with normal saline 90s thereafter. The needle was inserted vertically at the pars plana 4 mm posterior to the limbus, and 2 mg/0.05 mL of aflibercept was injected.The needle insertion site was compressed with a cotton swab,and the intraocular pressure (IOP) was monitored 15min later. The conjunctival sac was coated with tobramycin and dexamethasone.
Test IndicatorsOphthalmological examinations were performed on all patients 1d before and 1mo after surgery,including: 1) IOP was measured using a noncontact tonometer,2) best corrected visual acuity (BCVA) was measured by refraction, and the results were converted into the logarithm of the minimum angle of resolution (logMAR) visual acuity for recording, 3) anterior segment was examined using slit lamp,4) the fundus was observed using a 90 D lens, 4) CRT was measured using OCT, and the foveal avascular zone (FAZ)area, vessel density (SVD) of superficial retinal capillary plexus (SCP), and vessel density (DVD) of deep retinal capillary plexus (DCP) were observed using OCTA, 5) mean light sensitivity (MLS), 2° fixation rate (P1), and 4° fixation rate (P2) of the macular area were observed using an MP‐3 microperimetry.
Optical Coherence Tomography AngiographyOCTA(CIRRUS HD‐OCT, Carl Zeiss Meditec Inc, Dublin, CA,USA) examination was used to perform three transverse and longitudinal cross scans in the macular area in the range of 3×3 mm2using the AngioPlex mode, and the obtained retinal and choroidal blood flow images were stratified using the system built‐in analysis software. The images of the SCP and DCP were converted into 8‐bit grayscale images using Image J software. The FAZ area was measured, SVD and DVD were calculated. All patients were examined by an experienced ophthalmologist.
MicroperimetryThe patients underwent MP‐3 microperimetry (NIDEK Co., Ltd., Aichi, Japan) with the parameters set as follows. In the MP1 Macula‐10deg mode,retinal light sensitivity within 10° (approximately 3 mm) of the macular area and fixation rates at 2° and 4° were measured.The number of stimulation points was 40, arranged in inner,middle, and outer concentric circles, with a diameter of 2°and 8 points for the inner circle, 6° and 16 points for the middle circle, and 10° and 16 points for the outer circle. The background cursor was white light with a luminance of 31.4 apostilbs, and the stimulus cursor was Goldmann III, white,with a duration of 200ms. The maximum stimulus source luminance was 1000 apostilbs, the fixation target was red,cross, and 1° in size, and the light sensitivity threshold ranged from 0 to 34 dB. For examination in the dark room, mydriasis was not required, and if the pupil was small (<3.3 mm), it could be dilated and the untested eye needed to be shielded.The 2° fixation rate represents the ratio of fixation points in the circle with the fovea as the center and 2° as the diameter to all fixation points, represented by P1. The 4° fixation rate represents the ratio of fixation points in the circle with the fovea as the center and 4° as the diameter to all fixation points, represented by P2. MLS, P1 and P2 are all recorded for analysis.
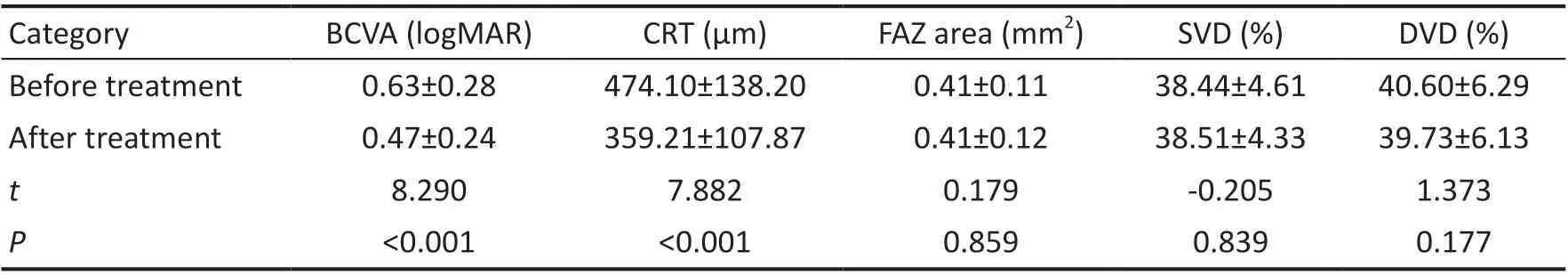
Table 1 Changes of BCVA, CRT, FAZ area, SVD and DVD mean±SD
Statistical AnalysisAll data were analyzed using SPSS 26.0 statistical software. The normal test and homogeneity test of variance were performed for all parameters. Data that met the normal distribution were expressed as mean±standard deviation (SD), and the paired samplet‐test was performed on preoperative and postoperative 1‐month data. Data that did not meet the normal distribution (P1, P2) were expressed as median (interquartile range; IQR) and subjected to the Wilcoxon signed rank‐sum test. Pearson correlation analysis was used for analyzing the correlation between the factors, and Spearman correlation analysis was used for data that did not meet the bivariate normal distribution. Considering inclusion of both eyes from some patients, we apply the generalized estimate equation (GEE) model to compensate for inter‐eye correlation of bilateral cases. Scatterplots were drawn using the R language. The difference was considered statistically significant whenP<0.05.
RESULTS
General InformationTotally 28 patients (42 eyes) diagnosed with DME, including 16 men (24 eyes) and 12 women (18 eyes), aged 29‐75y (56.50±11.07y) were enrolled.
Best Corrected Visual Acuity and Central Retinal ThicknessAfter treatment, BCVA improved from 0.63±0.28 to 0.47±0.24 logMAR (P<0.001). CRT decreased from 474.10±138.20 to 359.21±107.87 μm (P<0.001; Table 1).
Foveal Avascular Zone Area, Vessel Density of Superficial and Deep Retinal Capillary PlexusAfter treatment, the FAZ area, SVD, and DVD was not significantly changed (P>0.05;Table 1).
Retinal Mean Light Sensitivity and Fixation RateThe MLS after treatment was 22.16±4.20 dB, which was significantly higher than that before treatment (19.63±4.23 dB,P<0.001).No significant change was found in P1 (P=0.086) however significant change was observed in P2 after treatment (P=0.007;Table 2). The OCT, OCTA, and microperimetry of DME patients before and after treatment are shown in Figure 1.
Correlation Analysis of FactorsThe results of the correlation analysis of factors before and after treatment showed that pretreatment BCVA (logMAR) was positively correlated with the CRT (r=0.493,P=0.001), and negatively correlated withMLS (r=‐0.690,P<0.001), P1 (r=‐0.388,P=0.011), and P2(r=‐0.492,P=0.001), and was not correlated with FAZ area(r=0.262,P=0.094), SVD (r=0.121,P=0.446), and DVD(r=‐0.050,P=0.753). The CRT was negatively correlated with MLS (r=‐0.318,P=0.040), and had no correlation with FAZ area (r=0.275,P=0.078), SVD (r=0.261,P=0.095), DVD(r=0.097,P=0.540), P1 (r=‐0.298,P=0.055), and P2(r=‐0.195,P=0.215). The MLS was positively correlated with P1 (r=0.444,P=0.003) and P2 (r=0.513,P=0.001) and had no correlation with FAZ area (r=‐0.223,P=0.155), SVD (r=0.158,P=0.316), and DVD (r=0.246,P=0.116; Figures 2 and 3).
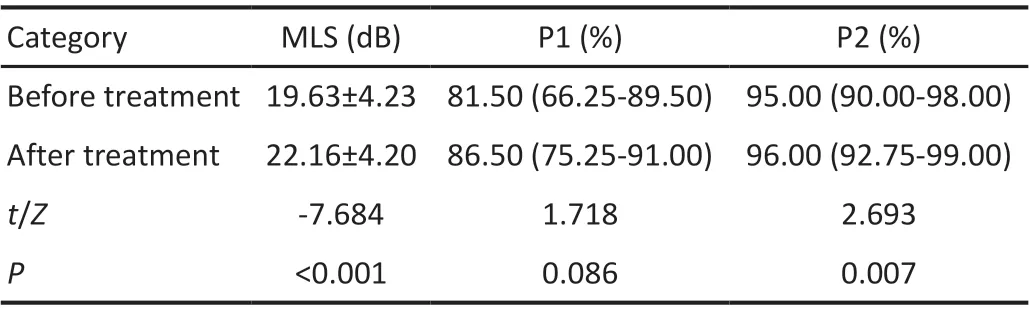
Table 2 Changes of MLS, P1 and P2 mean±SD or M (IQR)
Post‐treatment BCVA was positively correlated with the CRT (r=0.505,P=0.001), negatively correlated with MLS (r=‐0.597,P<0.001), P1 (r=‐0.341,P=0.027), and P2(r=‐0.371,P=0.016), and had no correlation with FAZ area(r=0.227,P=0.148), SVD (r=0.034,P=0.829), and DVD(r=‐0.079,P=0.621). The CRT was negatively correlated with the MLS (r=‐0.455,P=0.002) and had no correlation with FAZ area (r=0.170,P=0.283), SVD (r=‐0.013,P=0.937), DVD(r=‐0.032,P=0.839), P1 (r=‐0.256,P=0.102), and P2 (r=‐0.183,P=0.247). MSL had no correlation with FAZ area (r=‐0.153,P=0.333), SVD (r=0.303,P=0.051), DVD (r=0.261,P=0.095),P1 (r=0.209,P=0.185), and P2 (r=0.204,P=0.194).The GEE model was performed with the MLS before and after treatment as the dependent variable and with all factors correlated with the MLS as the independent variables. BCVA was found to be an independent factor affecting the MLS (Table 3).
DISCUSSION
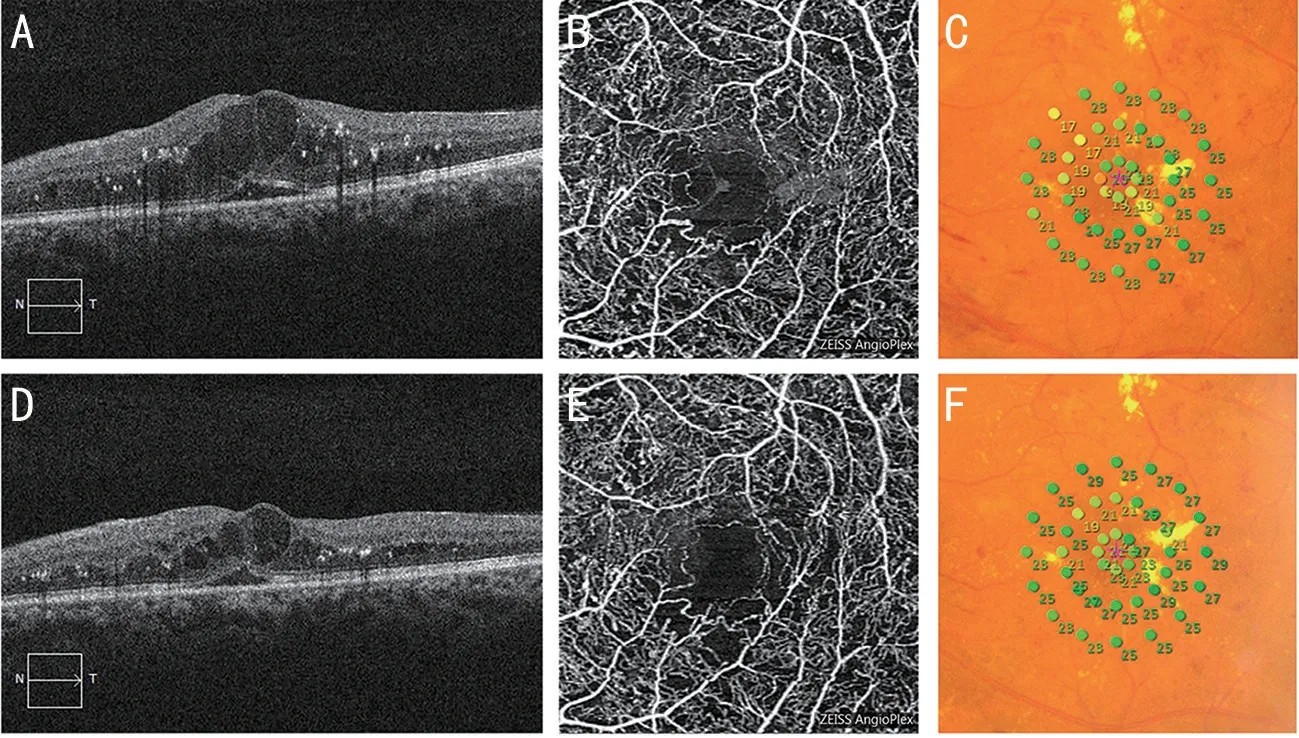
Figure 1 Examination results of the left eye of a patient with DME (male, 48 years old) before and after treatment A: OCT image before treatment showed cystoid edema in the macular; B: OCTA image before treatment, which revealing the destruction of the superficial capillary layer arch ring and nonperfused areas; C: 10° microperimetry results before treatment, which showed a regional decrease in retinal light sensitivity, with an MLS of 22.6 dB; D: OCT image after treatment, which revealing that macular edema was reduced; E: OCTA image after treatment, which revealing that the superficial capillary layer was not significantly changed; F: 10° microperimetry results after treatment,revealing that the local retinal light sensitivity was improved, with an MLS of 24.5 dB; DME: Diabetic macular edema; OCT: Optical coherence tomography; OCTA: Optical coherence tomography angiography; MLS: Mean light sensitivity.
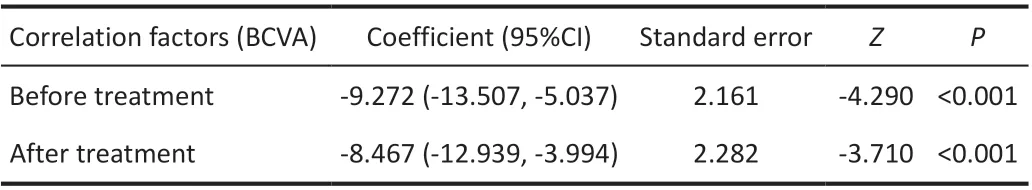
Table 3 Analysis of GEE of BCVA and MLS before and after treatment in patients with DME
DME is a form of DR and a major cause of central vision loss in patients with DR. Although DME is one of the major complications of diabetes, its pathogenesis is not fully understood. The hyperglycemic state promotes the activation of multiple interrelated pathways, leading to the formation of reactive oxygen species and an increase in local concentration beyond the antioxidant capacity. Free radicals, advanced glycation end products, inflammatory processes, or VEGF can cause disruption of the blood‐retinal barrier, ultimately leading to vascular leakage and retinal thickening in patients with DME[6,10]. According to the European Society of Retina Specialists guidelines, anti‐VEGF agents are generally recommended as the first‐line treatment for DME, while aflibercept[11]is preferred for patients with baseline visual acuity less than 69 letters. In this study, changes in macular structure and retinal function were evaluated with OCTA and MP‐3 microperimetry after treatment with aflibercept injection in patients with DME, confirming that anti‐VEGF therapy could effectively reduce foveal thickness and improve retinal light sensitivity and visual acuity.
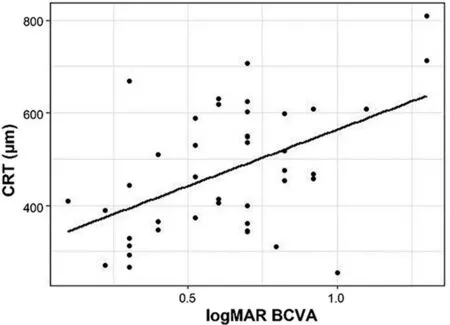
Figure 2 Scatterplot of correlation analysis between pretreatment BCVA and CRT BCVA: Best corrected visual acuity; logMAR: Logarithm of the minimum angle of resolution; CRT: Central retinal thickness.
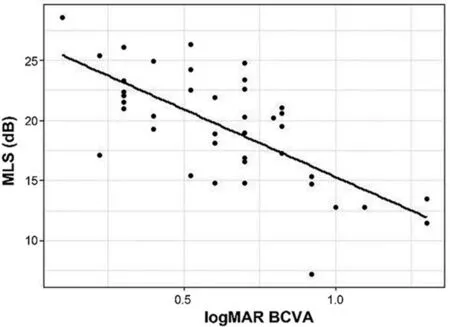
Figure 3 Scatterplot of correlation analysis between pretreatment BCVA and MLS BCVA: Best corrected visual acuity; logMAR:Logarithm of the minimum angle of resolution; MLS: Mean light sensitivity.
OCT is a noninvasive test that can provide morphological information of the retina, especially the macular area, and is the most commonly used imaging test for the diagnosis and follow‐up of DME[12]. As a new OCT‐based vascular imaging technique, OCTA can display retinal plexus in layers,quantify microvascular parameters, and correlate them with functional and morphological data[13]. In a recent study, Yuet al[14]retrospectively analyzed the effect of triamcinolone acetonide combined with anti‐VEGF in the treatment of DME and concluded that the combination treatment group was better in terms of improvement in BCVA and CRT. However, the authors did not measure whether it had an effect on macular microvessels and retinal sensitivity. In our study, we examined macular microvessels and retinal sensitivity to obtain a comprehensive knowledge of changes in macular structure and function. AttaAllahet al[15]used OCTA to assess macular blood perfusion in patients with DME alone and moderate‐to‐severe non proliferative DR. The macular vessel density and FAZ area in the DME and diabetic non‐DME groups and healthy controls were compared. It was found that the vessel density in the macular area and FAZ area significantly decreased in the DME group compared with the other two groups, while the FAZ area in the SCP significantly increased. Also, in patients with DME, the eyes with a larger FAZ had poor visual acuity.Hence, it was concluded that the aforementioned OCTA biomarkers could be used to predict the evolution of visual acuity and monitor the treatment response.
In this study, the visual acuity of patients with DME significantly improved after treatment, the CRT also significantly decreased.This result was consistent with the study results of Shimuraet al[16]. However, the limitation was that this was not a controlled study on different types of DME and failed to analyze the changes in the CRT in patients with different types of DME. One month after intravitreal injection of aflibercept,the FAZ area and the vessel density of SCP and DCP did not change significantly compared with those before treatment.Recently, Mirshahiet al[17]investigated the changes in macular microvessels after intravitreal injection of bevacizumab in patients with DME, revealing no significant differences in the FAZ area and vessel density in different retinal capillary layers compared with baseline. Buschet al[18]reported that retinal vessel density was also not significantly changed after intravitreal injection of aflibercept in treating DME. The results of both studies were consistent with the results of this study.
We concluded that although anti‐VEGF therapy could reduce fluid leakage, it might not dredge occluded blood vessels and improve macular perfusion. However, in this study, the local vascular perfusion of some patients after anti‐VEGF treatment was improved, which might be related to the regression of edema in a short time. When macular edema was severe,the exudated fluids squeezed the retinal vessels, and part of the blood flow signal was obscured, and there was no blood flow signal on OCTA. After the edema subsided, the blood flow signal reappeared. In fact, the perfusion state of macular vessels might not be changed. Mirshahiet al[19]found that macular edema was associated with more non‐perfusion in OCTA compared to dry macula. Therefore, the inability of anti‐VEGF treatments to improve capillary non‐perfusion could be a reason for recurrent DME following intravitreal injection of aflibercept. These results suggested that although the short‐term application of anti‐VEGF drugs in treating DME could reduce macular edema, this might not significantly improve the occlusion of retinal vessels and did not exacerbate the nonperfusion state of macular vessels.
Microperimetry is a technique that combines fundus imaging and automated perimetry to achieve anatomical and functional associations[20]. The treatment of DME is usually based on morphological changes. However, patients are more concerned about the improvement in visual function. Central visual acuity provides complete visual function information for diagnosing and treating DME. Compared with visual acuity, retinal sensitivity accurately quantifies the macular visual function status and is one of the best indicators for evaluating visual acuity[21]. The MP‐3 microperimetry provides the precise assessment of macular function and measurement of retinal light sensitivity and fixation stability[22]. The MLS within 10°of the retina was measured in this study because the posterior pole of the retina had the parameters of 1° about 300 μm and 10° about 3 mm, which could be consistent with the OCTA scan range of 3×3 mm2and facilitate comparative studies. On comparing the MLS and the changes in fixation rates at 2° and 4° after and before treatment in patients with DME, the MLS was found to significantly increase after treatment compared with that before treatment, and the results were consistent with the study results of Xuet al[23]. Sugimotoet al[24]treated patients with DME with a monthly intravitreal injection of anti‐VEGF agents and found a significant increase in the mean retinal sensitivity of 24.1±2.8 dB after 3mo compared with the baseline of 21.8±3.1 dB (P=0.006), consistent with the results of this study. In our study, P1 did not change significantly from baseline after treatment, and P2 significantly improved from baseline, with statistically significant results (P=0.007),which was not completely consistent with the study results of Seidenstickeret al[25], which might be related to the number of injections and follow‐up time. We hypothesized that the mean retinal sensitivity and fixation stability, especially P2, could be significantly improved early in patients with DME receiving anti‐VEGF therapy. However, no significant change in P1 was found. This may be due to the fact that the improvement of P1 requires higher fixation stability than that of P2, the improvement of visual function after a single injection of aflibercept is limited, so the fixation stability only changes significantly in P2, but not in P1, which requires more stable fixation. It means that P2 may provide early signs of improvement in fixation stability. Retinal sensitivity and fixation rate can be used as additional parameters in the follow‐up of DME treatment, which can provide us with more information about the changes of visual function in patients with DME.
The correlation analysis of all factors showed that MLS in patients with DME was negatively correlated with BCVA and CRT, consistent with the results of Vujosevicet al[26]and inconsistent with the results of Kimet al[27]. The changes of visual function caused by macular edema could be better reflected by retinal sensitivity. Previous studies showed a significant correlation between the foveal thickness measured using OCT and the BCVA in patients with DME[28‐30], which was consistent with the results of this study. Therefore, we believed that retinal sensitivity and BCVA could be used as important indicators to evaluate macular visual function.In addition, the MLS positively correlated with P1 and P2 before treatment, but the correlation between MLS and P1 and P2 disappeared after treatment. The analysis showed that it might be related to the unstable state of retina caused by the injection of aflibercept in a short time. Longer follow‐up time to observe the changes is necessary. In this study,multiple linear regression analysis was performed for the MLS and its related factors. The results showed that BCVA was an independent factor affecting the MLS. The reasons for some differences between this study and previous studies might be related to the sample size and the degree of macular edema. In addition, it might also be related to the type of microperimetry.Previous studies mostly used MAIA microperimetry or MP‐1 microperimetry, but this study used the latest generation of MP‐3 microperimetry. Different parameters and internal procedures between different instruments might also affect the results. Although we have made an in‐depth discussion on the variables related to OCT, OCTA, and microperimetry,the study of the interaction between these parameters is still quite interesting and challenging, which requires us to increase the number of samples and prolong the follow‐up time to do further study.
OCTA combined with microperimetry revealed that the intravitreal injection of aflibercept in patients with DME could effectively reduce macular edema and improve retinal sensitivity, fixation stability, and visual acuity, while the FAZ area and retinal capillary density might not change significantly over a short time. This study had the following limitations.The sample size was relatively insufficient, DME was not classified, and only macular changes were observed in patients with DME after a single anti‐VEGF treatment. In addition,the level of systematic control of diabetes might influence the efficacy of anti‐VEGF agents. It is still necessary to increase the sample size and add a control group for further study and analysis in the future.
ACKNOWLEDGEMENTS
Conflicts of Interest: Zhang CH, None;Gong B,None;Huang C, None;Shu XW, None;Chen TY, None;Chen X,None;Wu CL, None;Wang Y, None.
 International Journal of Ophthalmology2023年1期
International Journal of Ophthalmology2023年1期
- International Journal of Ophthalmology的其它文章
- Instructions for Authors
- Macular vascularisation changes analysed using OCT angiography after successful rhegmatogenous retinal detachment repair
- Comparison of success rate and intraocular pressure spikes between selective laser trabeculoplasty and micropulse laser trabeculoplasty in African American and Hispanic patients
- Efficacy of custom-made soft keratoconus lenses on corneal aberrations and photic phenomena in patients with keratoconus: a corneal topography imaging based study
- Clinical observation of recombinant human nerve growth factor in the treatment of neurotrophic keratitis
- Destructive effects on endothelial cells of grafts in cytomegalovirus DNA-positive patients after keratoplasty
