Techniques to resect the distal ureter in robotic/laparoscopic nephroureterectomy
Weil R.Li,Benjmin R.Lee
aDepartment of Urology,Tulane University School of Medicine,New Orleans,LA,USA
bDivision of Urology,University of Arizona College of Medicine,Tucson,AZ,USA
Techniques to resect the distal ureter in robotic/laparoscopic nephroureterectomy
Weil R.Laia,Benjamin R.Leeb,*
aDepartment of Urology,Tulane University School of Medicine,New Orleans,LA,USA
bDivision of Urology,University of Arizona College of Medicine,Tucson,AZ,USA
Transitional cell
carcinoma;
Robotic
nephroureterectomy;
Laparoscopy;
Robotic surgical
procedures;
Ureteral neoplasms
Treatment of clinically-organ confined high grade urothelial carcinoma of the upper tract has historically comprised open nephroureterectomy,with the distal ureter and bladder cuff mobilized through a separate open pelvic incision.To decrease morbidity,urologists have increasingly adopted laparoscopy and robotics in performing nephroureterectomy.In many published series of laparoscopic nephroureterectomy,the distal ureter and bladder cuff are detached from the bladder endoscopically by a variation of the“pluck”technique,with the resulting bladder defect left to heal by prolonged indwelling urethral catheter drainage.While the distal ureter and bladder cuff can be excised laparoscopically,it does require advanced laparoscopic skills.With the wrist articulation and stereoscopic vision in robotic surgery,robotic nephroureterectomy(RNU)and bladder cuff excision can be performed in antegrade fashion to mimic the open technique together with the ability to intracorporeally close the bladder defect in a watertight,mucosa to mucosa fashion after excising the bladder cuff.In this review,we discuss the published minimally invasive techniques in resecting the distal ureter and bladder cuff during laparoscopic and RNU.
?2016 Editorial Office of Asian Journal of Urology.Production and hosting by Elsevier B.V.Ltd. This is an open access article under the CC BY-NC-ND license(http://creativecommons.org/ licenses/by-nc-nd/4.0/).
1.Introduction
Upper tract urothelial carcinoma(UTUC)is an uncommon type of cancer.It comprises 5%-10%of malignancies arising from the kidney[1].Similar to bladder cancer,UTUC has a high propensity for recurrence and progression.Prognosis is based on grade and stage.For clinically-organ confined disease,the standard of care for surgical management has been radical nephroureterectomy with excision of bladder cuff.Prior to the wide use of laparoscopy in urologicsurgery,open nephroureterectomy(ONU)was commonly done with either one extended flank/abdominal incision or with two separate incisions(i.e.,one for the nephrectomy and the other one for the distal ureterectomy).The bladder cuff was either excised by an extravesical or an intravesical approach.
In 1991,Clayman et al.[2]published their initial experience with laparoscopic nephroureterectomy (LNU). Compared to ONU,LNU has been shown to have decreased post-operative pain,decreased blood loss,and decreased recovery time[3].In comparative studies,LNU also offered similar oncologic outcomes[3].
While the nephrectomy part of the case is relatively straightforward,the management of the distal ureter and the bladder cuff has been a source of controversy for at least the past two decades.This is,in part,due to the advanced laparoscopic skills required to mobilize the distal ureter to the level of the bladder and reconstruct the bladder defect with laparoscopic suturing after excising the bladder cuff.Many of the earlier LNU literature advocate endoscopic management of the distal ureter,especially as it pertains to the intramural ureter and the ureteral orifice. This is otherwise known as the“pluck”technique.
With the introduction of robot-assisted laparoscopic surgery,the learning curve to performing distal ureterectomy and bladder cuff excision has been mitigated with the increased magnification,3-dimension vision,and 7 degrees of freedom offered by the da Vinci Surgical System (Intuitive Surgical,Sunnyvale,CA,USA).The more recent robotic literature on nephroureterectomy describe extravesical techniques in performing dissection of the distal ureter with concomitant bladder cuff excision,as one would perform in replicating the open approach.In this review,we discuss the different published techniques in the management of the distal ureter during nephroureterectomy and present the pros and cons of each technique.
2.Endoscopic management of the ureter
2.1.Variations of the“pluck”technique
In 1952,McDonald et al.[4]described their technique of endoscopic resection of the ureteral orifice into the perivesical fat.After freeing the ureter endoscopically,the nephroureterectomy was performed through a single flank incision.The ureter was placed on gentle traction to pull it away from the bladder(hence the term “pluck”).The bladder defect was not closed.This technique was not widely adopted in open cases,as there was concern of increased locoregional tumor recurrence with spillage of tumor cells from an unclamped ureter into the perivesical space during endoscopic resection of the ureter[5]. Although the bladder defect was not closed,there were no significant complications rates reported.
One main oncologic advantage of the pluck technique is the ability to minimize risk of continued drainage of cancer cells from a patent ureter during and after endoscopic resection.Many different options for ureteral occlusion have been developed,especially in the studies presenting results of LNU and hand-assisted LNU.These variations include suture ligation,fulguration of the ureteral lumen, occluding the ureteral lumen with a balloon,occluding the ureteral lumen with fibrin,or placement of a clip on the proximal ureter to prevent distal migration of UTUC cells.
In 1999,Gill et al.[6]published their technique of ligating the ureter transvesically with an ENDOLOOP ligature(Ethicon,Sommerville,NJ,USA).In this technique, two needlescopic ports were placed percutaneously into the bladder under cystoscopic guidance.The ENDOLOOP was placed through the port on the same side as the target ureteral ori fice.A ureteral catheter was advanced through the ENDOLOOP and the ureteral ori fice.With a Collins knife through the resectoscope,the bladder cuff,intramural ureter,and extravesical ureter(3-4 cm)were circumferentially mobilized to the extravesical fat. After removing the ureteral catheter,the ENDOLOOP was tied down around the ureter to occlude the lumen.The ureteral ori fice was also fulgurated.After completion of the endoscopic procedure,the authors repositioned the patient in flank position for retroperitoneal LNU.The bene fit to this approach is ligation of the distal segment to prevent tumor spillage.Contemporary trends have moved towards placement of clip on the ureter via peritoneal approach to prevent distal tumor migration.
Agarwal et al.[7]also described a technique in occluding the ureter with the ENDOLOOP.In their method, which was done transurethrally,the authors mobilized the ureteral orifice with the Collins knife without detaching the ureter or exposing the perivesical fat prior to ligation of the ureteral stump with the ENDOLOOP.After the stump was ligated,they then further mobilized the ureter more proximally to the perivesical fat to detach the ureter from the bladder.
Wong and Leveillee[8]described a hand-assisted LNU approach in which they first proceed with nephrectomy. Prior to dissecting out the kidney,the ureter was clipped. The main advantage of this approach is that the kidney is able to be mobilized and hilum controlled with a larger working space,and then after the kidney was mobilized, the ureter was mobilized to the intramural hiatus.With the laparoscopist maintaining tension on the ureter,the cystoscopist excised the bladder and intramural ureter with a Collins knife.The main disadvantage to this approach is that a second monitor and camera are required to resect the distal ureter from below while the pneumoperitoneum is maintained.The bladder defect was not closed.A nonhand-assisted LNU approach was similarly described by Tan et al.[9].The benefit to this approach included the direct visualization of perivesical fat upon dissection of the distal ureter,with confirmation that the entire transmural ureter was free,minimizing the chances of local recurrence.
Vardi et al.[10]described a similar hand-assisted LNU approach in which they also clipped the ureter prior to completing the nephrectomy.Instead of using the resectoscope,they used a 5 Fr electrode(on cutting current)through a flexible cystoscope to resect the bladder cuff.
In Zou et al.[11],the authors instilled carbon dioxide gas into the bladder to establish a pneumovesicum.They excised a bladder cuff around the ureteral orifice with a Collins knife and mobilized the ureter to the perivesical fat. They then placed a 10 mm suprapubic trocar into thebladder so that Hem-o-lok clips(Teleflex,Morrisville,NC, USA)could be placed through the port to occlude the ureter.The authors claimed that compared to saline irrigation, carbon dioxide insufflation of the bladder provided better visualization(particularly when there is bleeding from instrumentation)and minimized risk of cancer cell spillage.
In Cormio et al.[12],the lumen of the distal ureter was occluded with the balloon of the 5 Fr Fogarty occlusion catheter.The bladder cuff was the excised around the catheter.The proximal ureter was then clipped during nephroureterectomy.The catheter balloon was palpated during dissection of the distal ureter.The catheter was clamped and cut distally to maintain balloon inflation.
In Mueller et al.[13],the lumen of the distal ureter was occluded with injection of 5 mL of Tisseel through an 8 Fr olive-tipped ureteral catheter.Prior to dissecting out the ureteral orifice with the Collins knife,the ureteral occlusion was confirmed with the injection of intravenous indigo carmine.
In Geavlete et al.[14],an Olympus bipolar“button”type electrode was used to vaporize tissue around the ureteral orifice until the perivesical fat was exposed.Prior to detaching the distal ureter from the bladder,the ureteral orifice was coagulated to close its lumen.
In Guo et al.[15],the authors excised the ureteral orifice and bladder cuff with Thulium laser.After mobilizing the ureteral stump to the perivesical fat,they vaporized the mucosa of the ureteral orifice with the laser fiber to seal the ureteral lumen closed.
2.2.Ureteral stripping/intussusception of the distal ureter
An alternative endoscopic method to the“pluck”technique was ureteral intussusception.In 1953,McDonald[16]presented the initial technique for ureteral intussusception and transurethral ureteral stripping of the distal ureter. Ureteral intussusception typically involved retrograde endoscopic insertion of a ureteral catheter into the ureter. A nephrectomy was then performed,during which the proximal ureter was ligated prior to dividing the ureter at that level.The distal part of the divided ureter was then tied to the pre-placed ureteral catheter.After mobilizing the ureter as distally as possible(i.e.,below the common iliac vasculature),the catheter was placed on gentle traction to intussuscept the ureter into the bladder.The ureteral orifice and intramural ureter were then dissected out transurethrally with a resectoscope.Like the “pluck”technique,the resulting bladder defect was not closed and allowed to heal with Foley catheter drainage.The advantage of the intussusception technique is that it ensures complete removal of the distal ureter and bladder cuff.
The success of the intussusception technique varies depending on the series presented in literature.This technique is typically limited to tumors involving the renal pelvis(i.e.,not the ureter).Clayman et al.[17]demonstrated technical success in 18 patients,with no local recurrence of tumor in 14 patients having follow-up data for at least 5 years.In contrast,in a more contemporary case series of 32 patients,the ureteral stripping failed intraoperatively for six patients(18.7%)[18].Those patients required a separate incision to extract the distal ureter and bladder cuff.The failure rate of intussusception has been reported as high as 26.3%in Matsushita et al.’s study[19].It is not clear why the local recurrence rate after intussusception is higher,perhaps because cells are shed during the extraction technique.
3.Laparoscopic excision of distal ureter and cuff
In comparison to the“pluck”and ureteral stripping techniques,laparoscopic excision of the distal ureter and bladder cuff is technically more difficult to perform.It, however,allows intracorporeal closure of the bladder defect to minimize spillage of urine(and potential cancer cells)into the perivesical space.
In 1995,McDougall et al.[20]presented their initial case series of 10 patients undergoing LNU.In their initial practice,they placed a ureteral balloon into the distal ureter, and incised the ureteral orifice and the entire intramural ureter over the balloon.After exchanging the ureteral balloon for an occlusion balloon catheter,inflated in the renal pelvis and placed on traction at the ureteropelvic junction,the ureteral orifice and intramural ureter were fulgurated.After repositioning the patient for LNU,the ureter was mobilized laparoscopically to the ureterovesical junction.After removing the occlusion catheter from the ureter,the surgeon fired the laparoscopic titanium stapler on the bladder wall just distal to the ureterovesical junction.The laparoscopic nephrectomy was then performed.
In an update of that case series,Shalhav et al.[3] compared the results of 25 and 17 patients who underwent LNU and ONU,respectively,with similar oncologic outcomes(i.e.,intravesical recurrence,cancer specific survival).In another retrospective case series comparing 12 patients who underwent LNU with extravesical stapling and ONU with transvesical distal ureterectomy,the positive margin rate and the rates of local/bladder recurrence were not statistically different[21].However,in a series of handassisted LNU with different methods of distal ureteral management,two out of seven patients(29%)who underwent the laparoscopic stapling technique had positive surgical margin involving the distal ureter[22].
Tsivian et al.[23]described the use of the 10 mm LigaSure(Medtronic,Minneapolis,MN,USA)to incise the bladder cuff.Similar to the stapling technique,the ureter was also mobilized to the ureterovesical junction.After clearing a 1 cm area of bladder adventitia around the ureterovesical junction,the bladder cuff was divided with the LigaSure extravesically.The authors reported no positive margins and confirmed absence of ipsilateral ureteral orifice on subsequent surveillance cystoscopy.In the mean follow-up of 11.6 months,there was no local recurrence, and the two bladder recurrences were away from the bladder cuff scar.
Lambert et al.[24]also reported their experience with the use of LigaSure in dividing the bladder cuff.Of the 22 patients who underwent either LNU or hand-assisted LNU, four required intracorporeal suturing to reinforce areas of bladder leakage.One patient had a remnant ureteral orifice noted on subsequent surveillance cystoscopy.This seriesalso reported no positive surgical margins and no recurrences at the bladder cuff scar site.
Cho et al.[25]described their technique of using a bulldog clamp on the bladder cuff prior to dividing the cuff to minimize intraoperative urine extravasation from the bladder.During LNU,the authors dissected the distal ureter past the intramural ureter to expose the bladder mucosa. This cuff of mucosa was then clamped with a laparoscopic bulldog clamp.Prior to dividing the cuff proximal to the bulldog clamp,the distal ureter was additionally clamped with a Hem-o-lok clip.After suturing the mucosa in running fashion,the clamp was removed,and the second layer was sutured in interrupted fashion.
Liu et al.[26]reported a modification of the bulldog clamp technique.They used a custom-made laparoscopic bulldog clamp with a curved tip and stronger closing force. They also used a barbed suture to close the bladder in two layers,with the clamp removed after completing the first layer.None of the 31 patients had positive surgical margin. The ureteral orifice was surgically absent on surveillance cystoscopy.There was no local or bladder recurrence noted in the mean follow-up of 10.5 months.
4.Robotic excision of distal ureter and cuff
In the earlier,published case series of robotic nephroureterectomy(RNU),a combination of laparoscopy for the nephrectomy portion of the case and robotics for the distal ureterectomy and bladder cuff excision was performed. The patients were also often repositioned to lithotomy position for the distal ureterectomy portion of the case. With the exception of Nanigian et al.[27],most of the RNU case series mobilize the distal ureter extravesically.
At our institution,we prefer to perform the nephrectomy part of the case laparoscopically(to decrease the overall surgical time)and subsequently mobilize the proximal ureter.During nephrectomy,the ureter is identified and clipped at the level of the proximal ureter.If the UTUC involves the ureter,additional clips are placed distal to the level of the ureteral tumor.The advantage of this approach is the relative quick portion of the nephrectomy,on the order of 65-90 min.
For the distal ureterectomy part of the case,the robot (da Vinci Si)is docked in a three-robotic arm configuration with the patient remaining in lateral decubitus position. While placing the ureter on traction,the ureter is mobilized to the detrusor hiatus to expose the intramural ureter.A stay suture(e.g.,2-0 polyglactin on SH needle)is placed into the detrusor muscle above the ureter(Fig.1),prior to dividing the bladder cuff to improve visualization and exposure,as the bladder defect will often retract into the bladder once the ureter is disconnected.The detrusorrhaphy is performed in two layers with multifilament absorbable suture.The bladder is then irrigated to confirm a watertight closure via a 22-Fr Foley catheter.The specimen is extracted through a midline incision.A cystogram is performed in clinic 1 week postoperatively prior to removal of the Foley catheter.
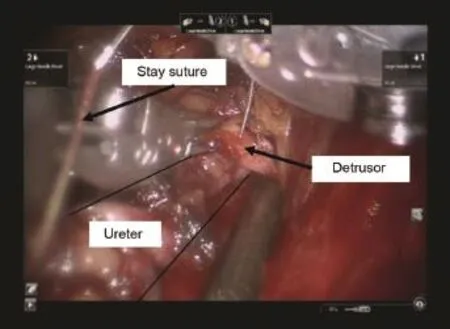
Figure 1 Distal ureterectomy during robotic nephroureterectomy:placement of stay suture into bladder prior to bladder cuff excision.
In Nanigian et al.[27],the authors placed a ureteral stent to identify the ureter,followed by laparoscopic nephrectomy.After positioning patient in Trendelenburg position,the robot was docked to the patient.A transverse incision was made through the posterior margin of the bladder dome for the intravesical approach.After placing a suture through the ureteral orifice and stent for traction, the ureteral orifice and distal ureter were mobilized circumferentially with the stent in place.The ureteral orifice defect was closed intravesically.The bladder dome incision was closed separately.The specimen was extracted through a Gibson incision.None of the 10 patients had positive margins.
Similar to Nanigian et al.[27],Hu et al.[28]also performed the nephrectomy laparoscopically and the distal ureterectomy robotically.The authors,however,do not place a ureteral stent as they dissected out the distal ureter and bladder cuff extravesically.They also extracted the specimen through a midline incision.
Park et al.[29]described one of the first published case series to perform both the nephrectomy and the distal ureterectomy robotically.In the first six patients of their series,the patient was repositioned,and the robotic was re-docked when switching over from nephrectomy to distal ureterectomy part of the case.An 8 mm robotic trocar was inserted into a 12 mm trocar for a hybrid trocar configuration.For the subsequent five patients,they kept the patient in flank position throughout the case without redocking the robot.For all the patients in the series,they reassigned the instrument arms to a different set of trocars for the distal ureterectomy part of the case.
Hemal et al.[30]used a four-robotic arm approach to perform RNU on 15 patients without repositioning the patient or re-docking the robot.No hybrid trocars were used.Like Park et al.[29],the robot arms were physically reassigned different ports when switching from nephrectomy to ureterectomy configuration.Prior to excising the bladder cuff,stay sutures were placed around the ureterovesical junction to avoid bladder wall retraction after the bladder cuff was excised.In their approach,the ureteral orifice can be visually confirmed before fully excising the bladder cuff.
Lee et al.[31]also reported a four-robotic arm approach in RNU without repositioning the patient or re-docking therobot.With the exception of the assistant port,the ports were placed along a“modified paramedian line”(which is an imaginary line that extends from the mid-axillary line at the level of the costal margin to the insertion of the rectus muscle at the pubic symphysis).Prior to mobilizing the colon and identification of the ureter,the authors left the robotic third arm undocked to minimize arm collision.The instrument arms remained physically assigned to the same ports throughout the case.
Patel et al.[32]described their experience with a fourrobotic arm approach on the da Vinci Xi robotic platform.In comparison to their previous work which was done on the S and Si platforms[30],the authors noted that the robotic ports can be placed linearly along the pararectus line,with the line shifted medial or lateral depending on the patient’s body habitus.They also noted that in certain scenarios,the camera could be moved to a different port without the need to reposition the arms to the trocars.
5.Discussion
Open surgery,whether done extravesically or transvesically,has historically been the gold standard in the management of distal ureter and the bladder cuff.Given the low incidence of UTUC,there has been no randomized controlled trial to date to prospectively show superiority of one minimally invasive technique over others in their oncologic outcomes(e.g.,intravesical recurrence,local recurrence,cancer specific survival).Originally designed to reduce surgical incision morbidity,the“pluck”technique has been described in many variations in the earlier laparoscopic nephroureterectomy studies. With the increased utilization of robotic surgery,many authors have gone back to replicating the extravesical technique during RNU.
The advantage of the“pluck”technique is in its technical simplicity.Urologists are already trained in performing transurethral resection of bladder tumors with the resectoscope and can use similar instruments to mobilize the bladder cuff and the distal ureter.The risk of iatrogenic injury to the contralateral ureteral orifice is minimal with this approach.If the nephrectomy is performed before the distal ureterectomy,there is an oncologic advantage such that one can preemptively place a clip on the proximal ureter to decrease the risk of distal migration of UTUC prior to endoscopic resection of the distal ureter.
The disadvantage of the “pluck” technique is the potentially higher risk of locoregional recurrence of urothelial carcinoma at the site of the distal ureterectomy. Most variations of the“pluck”technique use saline for cystoscopic irrigation.As the bladder defect is not closed for this technique,the irrigation fluid can extravasate into the perivesical space and seed this area with cancer cells that have migrated either distally from the ureter or proximally from the bladder.Intravesical chemotherapy cannot be administered immediately after surgery to reduce the risk of intravesical recurrence of urothelial carcinoma.In addition,many publications report the need to use two different positions during surgery(i.e.,dorsal lithotomy for the endoscopic resection of the distal ureter and bladder cuff;modified lateral decubitus position for the nephrectomy).
While rarely used,the intussusception technique gives one the ability to ensure complete removal of bladder cuff under direct vision.It requires division of the proximal ureter during the nephrectomy portion of the case.It is associated with a high intraoperative failure rate,requiring a separate incision to remove the distal ureter and bladder cuff.It is also contraindicated in the presence of ureteral tumors.
The advantage of laparoscopic/robotic excision of the distal ureter is the ability to replicate the open approach in maintaining an intact ureter during nephroureterectomy. The bladder defect is closed in this approach,which leads to a shorter duration of urethral catheterization and provides the option to administer intravesical chemotherapy in the immediate postoperative period.As most authors excise the bladder cuff extravesically,this approach does run the risk of injuring the contralateral ureteral orifice. There is also the risk of incompletely mobilizing the bladder mucosa,which can lead to a higher risk of intravesical recurrence.
With the pure laparoscopic approach,more advanced skills are needed to isolate the ureter down to the detrusor hiatus and to suture the bladder defect closed.The learning curve in laparoscopy can be mitigated with the robotic approach,especially with the ease of suturing with the robot.
For institutions with access to the robot and with staff trained to use the robot,we recommend using the robot at least for the distal ureterectomy and bladder cuff excision. For the urologists who are facile with laparoscopy but do not have access to the robot,we recommend performing LNU with antegrade management of the distal ureter and bladder cuff(and suture closure of bladder defect)to maintain an oncologically safe approach as with open surgery.For the urologists who are not comfortable performing laparoscopic distal ureterectomy and bladder cuff excision, we advise early clipping of the ureter during laparoscopic nephrectomy or sealing the ureteral lumen during the endoscopic portion of the“pluck”technique to minimize downstream seeding of potential cancer cells into the perivesical space and the surrounding operative field.
Conflicts of interest
The authors declare no conflicts of interest.
[1]Siegel RL,Miller KD,Jemal A.Cancer statistics,2016.CA Cancer J Clin 2016;66:7-30.
[2]Clayman RV,Kavoussi LR,Figenshau RS,Chandhoke PS, Albala DM.Laparoscopic nephroureterectomy:initial clinical case report.J Laparoendosc Surg 1991;1:343-9.
[3]Shalhav AL,Dunn MD,Portis AJ,Elbahnasy AM,McDougall EM, Clayman RV.Laparoscopic nephroureterectomy for upper tract transitional cell cancer:the Washington University experience.J Urol 2000;163:1100-4.
[4]McDonald HP,Upchurch WE,Sturdevant CE.Nephro-ureterectomy:a new technique.J Urol 1952;67:804-9.
[5]Hetherington JW,Ewing R,Philp NH.Modified nephroureterectomy:a risk of tumour implantation.Br J Urol 1986;58: 368-70.
[6]Gill IS,Soble JJ,Miller SD,Sung GT.A novel technique for management of the en bloc bladder cuff and distal ureter during laparoscopic nephroureterectomy.J Urol 1999;161: 430-4.
[7]Agarwal DK,Khaira HS,Clarke D,Tong R.Modified transurethral technique for the management of distal ureter during laparoscopic assisted nephroureterectomy.Urology 2008;71: 740-3.
[8]Wong C,Leveillee RJ.Hand-assisted laparoscopic nephroureterectomy with cystoscopic en bloc excision of the distal ureter and bladder cuff.J Endourol 2002;16:329-32.discussion 332-3.
[9]Tan BJ,Ost MC,Lee BR.Laparoscopic nephroureterectomy with bladder-cuff resection:techniques and outcomes.J Endourol 2005;19:664-76.
[10]Vardi IY,Stern JA,Gonzalez CM,Kimm SY,Nadler RB.Novel technique for management of distal ureter and en block resection of bladder cuff during hand-assisted laparoscopic nephroureterectomy.Urology 2006;67:89-92.
[11]Zou X,Zhang G,Wang X,Yuan Y,Xiao R,Wu G,et al.A oneport pneumovesicum method in en bloc laparoscopic nephroureterectomy with bladder cuff resection is feasible and safe for upper tract transitional cell carcinoma.BJU Int 2011; 108:1497-500.
[12]Cormio L,Selvaggio O,Di Fino G,Massenio P,Annese P,de la Rosette J,et al.Transurethral distal ureter balloon occlusion and detachment:a simple means of managing the distal ureter during radical nephroureterectomy.J Endourol 2013;27: 139-42.
[13]Mueller TJ,DaJusta DG,Cha DY,Kim IY,Ankem MK.Ureteral fibrin sealant injection of the distal ureter during laparoscopic nephroureterectomy-a novel and simple modi fication of the pluck technique.Urology 2010;75:187-92.
[14]Geavlete P, Multescu R, Geavlete B, Georgescu D, Moldoveanu C.Bipolar plasma vaporization-an innovative intramural ureter detachment method during nephroureterectomy.J Med Life 2012;5:153-6.
[15]Guo G,Yang Y,Dong J,Zhenhong Z,Zhang X.A new 2-micrometer continuous wave laser method for management of the distal ureter in retroperitoneal laparoscopic nephroureterectomy.J Endourol 2015;29:430-4.
[16]McDonald DF.Intussusception ureterectomy:a method of removal of the ureteral stump at time of nephrectomy without an additional incision.Surg Gynecol Obstet 1953;97: 565-8.
[17]Clayman RV,Garske GL,Lange PH.Total nephroureterectomy with ureteral intussusception and transurethral ureteral detachment and pull-through.Urology 1983;21:482-6.
[18]Giovansili B,Peyromaure M,Saighi D,Dayma T,Zerbib M, Debre B.Stripping technique for endoscopic management of distal ureter during nephroureterectomy:experience of 32 procedures.Urology 2004;64:448-52.discussion 452.
[19]Matsushita Y,Owari Y,Nozawa T,Katoh T,Obara W,Isurugi K, et al.Transurethral removal of the ureter by the intussusception method in the treatment of renal pelvic and ureteral tumors.Hinyokika Kiyo 2000;46:241-5.
[20]McDougall EM,Clayman RV,Elashry O.Laparoscopic nephroureterectomy for upper tract transitional cell cancer:the Washington University experience.J Urol 1995;154:975-9. discussion 979-80.
[21]Romero FR,Schaeffer EM,Muntener M,Trock B,Kavoussi LR, Jarrett TW.Oncologic outcomes of extravesical stapling of distal ureter in laparoscopic nephroureterectomy.J Endourol 2007;21:1025-7.
[22]Brown JA,Strup SE,Chenven E,Bagley D,Gomella LG.Handassisted laparoscopic nephroureterectomy:analysis of distal ureterectomy technique,margin status,and surgical outcomes.Urology 2005;66:1192-6.
[23]Tsivian A,Benjamin S,Sidi AA.A sealed laparoscopic nephroureterectomy:a new technique.Eur Urol 2007;52:1015-9.
[24]Lambert EH,Schachter LR,Altamar HO,Tikhonenkov S, Moeckel G,Miller NL,et al.A sealed bladder cuff technique during laparoscopic nephroureterectomy utilizing the Liga-Sure electrosurgical device:laboratory and clinical experience.J Endourol 2010;24:327-32.
[25]Cho HJ,Kim SJ,Yoon BI,Lee JY,Kim SW,Hwang TK,et al.A novel bulldog clamp technique for management of a distal ureter and bladder cuff during laparoscopic nephroureterectomy.J Endourol 2010;24:1719-20.
[26]Liu P,Fang D,Xiong G,Yang K,Zhang L,Yao L,et al.A novel and simple modification for management of distal ureter during laparoscopic nephroureterectomy without patient repositioning:a bulldog clamp technique and description of modified port placement.J Endourol 2016;30:195-200.
[27]Nanigian DK,Smith W,Ellison LM.Robot-assisted laparoscopic nephroureterectomy.J Endourol 2006;20:463-5.discussion 465-6.
[28]Hu JC,Silletti JP,Williams SB.Initial experience with robotassisted minimally-invasive nephroureterectomy.J Endourol 2008;22:699-704.
[29]Park SY,Ham WS,Choi YD,Rha KH.Robot-assisted laparoscopic radical prostatectomy:clinical experience of 200 cases.Korean J Urol 2008;49:215-20.
[30]Hemal AK,Stansel I,Babbar P,Patel M.Robotic-assisted nephroureterectomy and bladder cuff excision without intraoperative repositioning.Urology 2011;78:357-64.
[31]Lee Z,Cadillo-Chavez R,Lee DI,Llukani E,Eun D.The technique of single stage pure robotic nephroureterectomy.J Endourol 2013;27:189-95.
[32]Patel MN,Aboumohamed A,Hemal A.Does transition from the da Vinci Si to Xi robotic platform impact single-docking technique for robot-assisted laparoscopic nephroureterectomy?BJU Int 2015;116:990-4.
Received 2 March 2016;received in revised form 25 April 2016;accepted 26 April 2016 Available online 11 May 2016
*Corresponding author.
E-mail address:brlee@surgery.arizona.edu(B.R.Lee).
Peer review under responsibility of Second Military Medical University.
http://dx.doi.org/10.1016/j.ajur.2016.04.001
2214-3882/?2016 Editorial Office of Asian Journal of Urology.Production and hosting by Elsevier B.V.Ltd.This is an open access article under the CC BY-NC-ND license(http://creativecommons.org/licenses/by-nc-nd/4.0/).
 Asian Journal of Urology2016年3期
Asian Journal of Urology2016年3期
- Asian Journal of Urology的其它文章
- Robot-assisted laparoscopic radical cystectomy with complete intracorporeal urinary diversion
- Current status of laparoscopic and robotassisted nerve-sparing radical cystectomy in male patients
- Stents for malignant ureteral obstruction
- Percutaneous resection of upper tract urothelial cell carcinoma:When,how, and is it safe?
- Thulium laser treatment for bladder cancer
- Narrow band imaging for bladder cancer
