Stents for malignant ureteral obstruction
Kristina Pavlovic,Dirk Lange,Ben H.Chew
Department of Urologic Sciences,The Stone Centre at Vancouver General Hospital,University of British Columbia,Vancouver,Canada
Stents for malignant ureteral obstruction
Kristina Pavlovic,Dirk Lange,Ben H.Chew*
Department of Urologic Sciences,The Stone Centre at Vancouver General Hospital,University of British Columbia,Vancouver,Canada
Malignant ureteral
Malignant ureteral obstruction can result in renal dysfunction or urosepsis and can limit the physician’s ability to treat the underlying cancer.There are multiple methods to deal with ureteral obstruction including regular polymeric double J stents(DJS),tandem DJS, nephrostomy tubes,and then more specialized products such as solid metal stents(e.g.,Resonance Stent,Cook Medical)and polyurethane stents reinforced with nickel-titanium(e.g., UVENTA stents,TaeWoong Medical).In patients who require long-term stenting,a nephrostomy tube could be transformed subcutaneously into an extra-anatomic stent that is then inserted into the bladder subcutaneously.We outline the most recent developments published since 2012 and report on identifiable risk factors that predict for failure of urinary drainage.These failures are typically a sign of cancer progression and the natural history of the disease rather than the individual type of drainage device.Factors that were identified to predict drainage failure included low serum albumin,bilateral hydronephrosis,elevated C-reactive protein, and the presence of pleural effusion.Head-to-head studies show that metal stents are superior to polymeric DJS in terms of maintaining patency.Discussions with the patient should take into consideration the frequency that exchanges will be needed,the need for externalized hardware(with nephrostomy tubes),or severe urinary symptoms in the case of internal DJS.This review will highlight the current state of diversions in the setting of malignant ureteral obstruction.
?2016 Editorial Office of Asian Journal of Urology.Production and hosting by Elsevier B.V.Ltd. This is an open access article under the CC BY-NC-ND license(http://creativecommons.org/ licenses/by-nc-nd/4.0/).
1.Introduction
Obstruction of the ureter can be commonly caused by advanced urological or non-urological malignant lymphadenopathy or by direct extension of the process. Ureteral stenting can bypass the obstruction in order to provide relief and prolong survival.Determining the cause and level of obstruction is important to determine theappropriate technique for urinary diversion.Those with malignant ureteral obstruction(MUO)have a median survival rate of 3.7-15.3 months[1].If untreated,ureteral obstruction can lead to renal failure and even death.Current management options include various types of stents, both metal and silicone,as well as nephrostomy tubes and extra-anatomic stents.However,it is often difficult to know which option would be most beneficial for the patient and their potential short life expectancy.As we continue to search for new ways to improve our techniques,we look at minimizing stent related symptoms,ease of the procedure, effect on quality of life(QoL),decreasing cost,and achieving high success rates. Recent research has addressed these issues and are the main highlights of this review article.
2.Methods
A PubMed review of publications in the English language was performed using the terms“metallic stents”,“tandem stents”,“extra-anatomic stents”,“nephrostomy tubes”, and“double J stents”published from 2012 to 2016.The majority of studies reviewed looked at MUO however studies investigating other etiologies were also included if they were deemed relevant to the topic.
3.Double J stents(DJS)
The most commonly used stent type is the standard DJS,named for its J-shaped curled ends.Manufactured from polyurethane,silicone,or various polymers,DJS are changed frequently at approximately 3-6 month intervals,as they are prone to encrustation,obstruction, migration,and fracture[2].Furthermore,one of the main problems associated with DJS is encrustation of stone formation on the surface of the stent[2]. Polymeric stents have shown to be inferior in long-term drainage when compared to metal stents in the setting of MUO[2,3].
4.Metallic stents
Metallic stents have become a feasible choice in the long-term management of MUO.Different types of metallic stents exist including the non-expandable coiled metallic Resonance stent(Cook Medical,Bloomington, IN,USA),the thermo-expandable metal alloy Memokath 051 stent(PNN Medical,Glostrup,Denmark),and the self-expandable covered metallic UVENTA stent (Taewoong Medical,Gojeong-ro,Wolgot-myeon,Gimposi,Gyeonggi-do,South Korea).
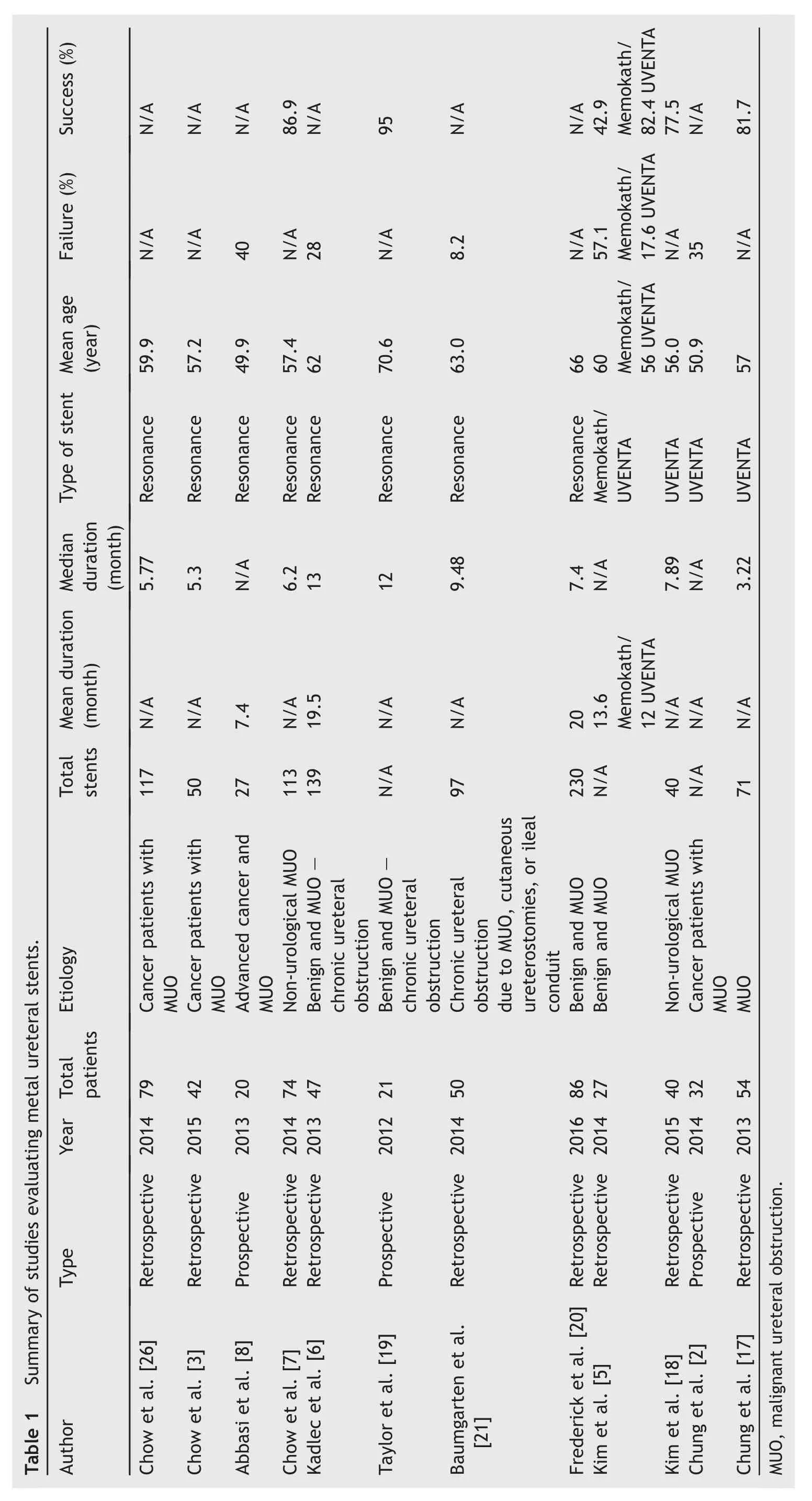
The Resonance stent is a nickel-cobalt-chromiummolybdenum alloy DJS[2](Fig.1).This stent does not have a lumen like the Memokath 051 and UVENTA stents; therefore,insertion of the stent is done through the lumen of a 10 Fr ureteric catheter under fluoroscopic guidance[4]. Outcomes from studies utilizing metal stents are shown in Table 1.

Figure 1 Resonance metallic ureteral stent(permission for use granted by Cook Medical,Bloomington,IN,USA).
The Memokath 051 stent is composed from a nickeltitanium alloy that forms a tight spiral structure[5](Fig.2). Regulating the temperature of the stent during insertion and removal is important for proper use of this stent[4]. Expertise is required to place the Memokath 051 stent,as insertion can be complicated and technically challenging[2]. Its coiled structure prevents urothelial ingrowth,preserves peristalsis,and reduces the risk of secondary ischemic damage to the ureteric wall[5].
Two layers of a self-expandable nickel-titanium alloy mesh covering a polytetrafluoroethylene (PTFE)layer combine to make the UVENTA stent(Fig.3).The outer mesh containing a nickel-titanium skeleton holds the stent against the ureteral urothelium preventing stent migration [5].The inner PTFE and mesh layers prevent tissue ingrowth and maintain patency by strengthening the overall radial force of the stent.
Kim et al.[5]were the first to publish a study comparing the UVENTA and Memokath 051 stents in 27 patients.Both types of stents demonstrated similar minor complications when used for both benign and MUO.However,the clinical success rate(defined as improved renal function and no obstruction on intravenous urography,computed tomography,or diuretic renography)of the UVENTA stent was significantly higher than the Memokath 051 stent(82.4%vs. 42.9%,respectively;p=0.031).The difference with success rate further increased when comparing just malignant obstruction (92% UVENTA vs. 33% Memokath 051; p=0.022).Failures in the Memokath 051 group included tumor progression,and stent migration.Failures in the UVENTA group included stent migration and mucosal hyperplasia causing luminal obstruction.Migration of the Memokath 051 was the biggest reason for differences between the two stents-all other failure reasons were equal between the two groups.Shortcomings of this study include the fact that these patients were retrospectively analyzed, the short-term follow-up,and the small sample size.The Memokath 051 and UVENTA had mean indwelling times of 13.6 months(range,7-21 months)and 12 months(range, 9-16 months),respectively.The small sample size precludes the authors from definitively identifying which factors predicted long-term success.
?

Figure 2 Memokath 051 ureteral stent(permission for use granted by PNN Medical,Glostrup,Denmark).
Kadlec et al.[6]performed a retrospective study on 47 patients with chronic ureteral obstruction and examined their results over a 5-year follow-up period.They found the median stenting duration for benign and malignant obstruction to be 22 months and 7 months,respectively (p=0.106).The mean stenting duration was 8 months for the Resonance stent before they were exchanged.The most common reason for early exchange was stent-related urinary tract infection(UTI).The majority(57%)of the patients were stented for MUO.They had 28%failure rate, with majority of these stents failing relatively soon after placement with a mean follow-up of 20 months.The authors did not find any pre-stent factor that was significantly associated with failure.Unlike previous studies,they found no difference between the results of patients requiring the metal stent for malignant or benign ureteral obstructions.
Chow et al.[7]reported similar results for their 74 patients who received the metallic Resonance stent for nonurological malignant diseases and MUO.The median functional duration was 6.2 months.Their success rate of insertion was 86.9%of which 91.2%achieved patency of the urinary system.Risk factors for stent failure were obstructions in the abdominal ureter(irregular thickening of the ureteral wall with abnormal enhancement and infiltration)and lymphatic metastasis around the ureter (p=0.0279 and 0.0398,respectively).Non-urological cancers have a lower risk of stent failure than urological cancers.No major complications were reported however minor complications such as UTIs,gross hematuria,dysuria, flank pain,urinary frequency,and stent migration, occurred.The Resonance stent was inserted in these patients only after they failed a regular polymeric DJS.The authors hypothesize,this delayed time to obtaining the Resonance may have resulted in cancer progression and a more dif ficult patient population in which to stent.Another study demonstrated similar positive results of the Resonance stent in patients with advanced cancer and MUO with a mean time to failure of 7.4 months[8].
These studies cannot be directly compared due to different patient populations,sample sizes,and etiologies, but a common trend is that metallic stents remain patent for a longer dwell time,thus eliminating the need for more frequent changes.Metal stents are also well tolerated with minimal lower urinary tract symptoms.Although the purchase price of each metal stent may be more costly than a regularpolymeric stent,itmay resultin overallcostsavingsif the number of visits to the operating room can be reduced.
Figure 3 UVENTA ureteral stent(permission for use granted by TaeWoong Medical Co.Ltd.,Gojeong-ro,Wolgot-myeon, Gimpo-si,Gyeonggi-do,South Korea).
5.Tandem stents
Inserting tandem ureteral stents,also known as twin ureteral stents,can be considered an alternative to the single DJS.In addition to an extra lumen,the side-by-side stents are thought to increase drainage as the second stent creates additional space between the two stents and the ureteral wall even if there is external compression.
Two studies have shown the effectiveness of tandem stents in patients with MUO.The first was a retrospective analysis of 187 cases in 66 patients,the largest experience with tandem ureteral stents to date[9].Tandem stents were inserted for both MUO and benign ureteral obstruction. The mean stent duration in these patients was 4.8 months. No complications were identified in their cohort and stent irritation occurred in 12 of the patients.Their results suggested tandem stent placement was highly successful in both benign and MUO.Patients with MUO had an approximated survival of 1 year,with the likelihood of mortality and shorter overall survival increasing with stent failures:71%of patients with MUO and previous stent failure died at a median 66 days,whereas 40%of patients with MUO and without stent failure died at a median 433 days.Stent failure was a prognostic factor for mortality and likely a sign of cancer progression in those patients.
The second study prospectively performed 22 tandem ureteral stent insertions in 15 patients with MUO[10].They also found that patients with failing tandem ureteral stents had a shorter life expectancy than those with functioning tandem stents(median life expectancy of 45.6 days vs. 162.5 days,respectively;p<0.05).Overall,they determined tandem stents can be an effective method of managing MUO in patients where a single DJS had previously failed[10].In both these studies,the patient mortality was almost certainly due to progression of the cancer,which resulted in failure of the stents to drain.
6.Nephrostomy tube
Percutaneous nephrostomy(PCN)tube insertion is a minimally invasive procedure that can be performed under local anesthesia by interventional radiologists or urologists. Complications that can occur during this procedure arebleeding,bowel transgression,sepsis,and pleural complications[11].It is an effective way of relieving ureteric obstruction and pain.However,the external drainage tube and bag can be burdensome,restrict physical activity,and negatively impact the patient’s QoL.Complaints regarding PCN include impaired body image,social dysfunction,and compromised sleep(especially with bilateral PCN)[12]. Minor complications resulting from the PCN tube include pain,dislodgment,blockage,infection,and frequent tube changes in addition to the routine 3-month changes[13].
Monsky et al.[13]prospectively evaluated the effect placement of PCN tube(Boston Scientific,Natick,MA,USA), an internal DJS(Boston Scientific),or an internal-external nephroureteral stent(Boston Scientific)for MUO had on QoL in 46 patients.Patients were not randomized to a specific intervention.A previously validated QoL survey,which included questions from a published survey specific to nephrostomy and nephroureteral stents,was taken at 7,30, and 90 days after placement.A common validated health index,to assess physical,social,functional,and emotional well-being was also included.The results indicated no significant difference in QoL between the three interventions.
Urinary symptoms and pain,including dysuria and urinary frequency,in those receiving DJS were significantly higherat 30 and 90 days that those with nephrostomies(p=0.0035 and p=0.0189,respectively),but not at 7 days after placement.Greatest use of pain medications at 30 and 90 days was seen in the DJS group(p=0.0189).DJS related procedures also required significantly longer fluoroscopy time(p=0.0054).There was no significant difference in UTIs and use of antibiotics between the groups(p>0.05). Routine changes were scheduled at 3-month intervals; however,due to a greater rate of complications,patients with nephrostomy tubes required more additional changes than DJS and internal-external nephroureteral stent (p=0.051).A total of 83%of nephrostomy tubes,36%of nephroureteralstents,and 16%of DJS were changed because of complications.Patients should be counseled regarding these symptoms when making a decision regarding the type of diversion they will receive.
Alawneh et al.[12]also updated and validated a prognostic model developed by Ishioka et al.[14]which predicts the overall survival in cancer patients after receiving PCN. PCN was performed in 211 patients with MUO.Statistically significant factors that predicted shorter survival after PCN included type of malignancy,presence of metastasis to any site,presence of pleural effusion,bilateral hydronephrosis, and low serum albumin<3.5 mg/dL.Patients were further categorized into fourrisk groups depending on the numberof these factors were present.Those with 0,1,2,and 3 risk factors had a median survival of 17.64,7.7,2.20,and 1.72 months,respectively(p<0.0001).The median survival rate forallpatientswas5.05 monthsand 87%ofthe patientsin the study were deceased by the end of the observation period illustrating the severity of the effects of the malignancies ratherthan the type ofurinary diversion patientsunderwent.
Azuma et al.’s retrospective study[15]also looked at factors that predicted poor prognosis for advanced cancer patients with MUO.A multivariate analysis compiled from 214 patients,found that low albumin,low sodium,and high C-reactive protein in the serum before PCN were associated with poor prognosis(p<0.0001).Three or more clinical events related to malignant dissemination before PCN was also another indicator of poor prognosis(p<0.0001).Degree of hydronephrosis was not an indicator in this study, but was shown to be an indicator in other studies described above[12].When divided into three risk groups,the median survival in the favorable(0 or 1 risk factor),intermediate(2 risk factors),and poor(3 or 4 risk factors)risk factor groups was 12.0,6.0,and 2.8 months,respectively(p<0.0001). The median overall survival was 6.4 months.The authors suggest examining these levels to ensure the patient is appropriately informed before making a decision on whether to have a PCN placed.
7.Extra-anatomic stent(EAS)
An EAS is an internal prosthetic replacement of the ureter,which allows urine drainage by bypassing the obstruction.It involves a PCN that is then tunneled subcutaneously along the abdomen and then inserted into the antero-superior portion of the bladder via cystotomy.None of the tubing is externalized and is all subcutaneous.This is a viable long-term option for patients who are too frail to undergo reconstruction surgery or do not want to do so[16].The primary candidates were those where previous stents or nephrostomy had failed.EAS is also used in transplanted kidneys and ileal conduits.
The normalpractice for Kimulietal.[16]wasto utilize two types of stents.The first was a short-term 8.5 Fr 65 cm EAS with side holes ateitherend.Ifthe patientsurvived and had a good prognosis afterthe use offirststent,a longer-term 29 Fr detour EAS would be used at the exchange.This second procedure has the potential of being a permanent solution, but requires open cystostomy,which is more invasive. Therefore,it is generally only considered the primary option for those with a longer life expectancy.Contraindications included uncorrected coagulopathies,tumor invasion along the stent,and active malignancy either arising or invading the bladder.Stent placement near a tumor is not advised as tumor seeding along the stent may occur.Both stent blockage and storage bladder symptoms were rare.Other complications include encrustation,infection,obstruction, or skin problems.One case presented with skin erosion,and two others had local tumor progression with bladder fistulae resulting in the removal of the stent.
With experience in over 100 patients at their institution, Kimuli et al.[16]determined that EAS offers a minimally invasive way to provide a temporary or permanent solution for internal urinary drainage.EAS was determined to be an alternative to a long-term nephrostomy tube,with the tubes being routinely changed at 12 months.
8.Metallic stents vs.plastic double J stents
When comparing the Resonance metallic ureteral stent to a regular polymeric stent in patients with MUO,Chow et al. [3]demonstrated a mean increase in functional duration of 4 months using the Resonance stent(p<0.0001).In this retrospective study,42 patients who had previously failed polymeric stents had their stent replaced with the Resonance stent.The degree of hydronephrosis was measuredboth prior to the placement of the polymeric stents and prior to the placement of the Resonance stent.Hydronephrosis and serum creatinine subsided or remained the same in 90%of these patients.Stent duration was not affected by severe hydronephrosis,suggesting the Resonance stent was more effective in relieving severe obstruction.No major complications were reported and no stents were exchanged due to non-tolerability.A few patients had minor complications that were similar to those seen with the polymeric stents.These included dysuria, fever,urinary frequency,flank pain,and hematuria.Preoperative serum creatinine<2 mg/dL,age≥60 years, gender,method of insertion(antegrade vs.retrograde), previous technical failure,genitourinary(GU)cancer, previous and ongoing radiotherapy,severe hydronephrosis, and occurrence of UTI were analyzed to determine if they were associated with good stent outcomes.Radiotherapy, GU cancer,and UTI were not associated with reduction of stent duration.Pre-operative serum creatinine<2 mg/dL was determined to be the only significant indicator of good stent outcome.Where prior polymeric stents failed,the Resonance stent presented an effective and safe method of relieving MUO[3].
Chung et al.[2]compared the UVENTA stent to the standard polymeric DJS[2].Data were prospectively collected from 32 patients with the UVENTA stent inserted and compared to data retrospectively collected from 56 patients with DJS.Both stents were placed for MUOs caused by various cancers.Minor complications included mild pain, hematuria,and UTIs in both groups.Stent migration only occurred in one UVENTA patient.Primary patency was defined as the time between the initial insertion of the stent and secondary procedure to ensure there was urinary drainage.Assisted primary patency was defined as the time between the initial insertion and repeat PCN.They found that the primary patency of the UVENTA stent was better than the assisted patency of DJS(p=0.012).In terms of patency and technical success,the UVENTA stent was determined to be superior to DJS.This study was not a randomized control study,but an effective method of urinary decompression similar to a previous study showing that the UVENTA stent was safe and effective in palliative treatment of MUO[17].
In a retrospective study of 40 patients,Kim et al.[18] established that long-term indwelling of DJS affected the subsequent UVENTA stent failure rate through their multivariate analysis of potential risk factors(p=0.037).They suggested this might be due to the anatomical,histological, and functional changes that are induced with long-term DJS.Other risk factors such as age,serum creatinine level at the time of stent placement,and history of previous radiation therapy were not statistically significant risk factors of UVENTA stent failure.
Standard polymer DJS are unable to provide the longterm drainage seen with metal stents[2-4].Therefore, unlike metal stents,polymeric or silicone stents are changed regularly at 3-6 month intervals,necessitating a minimum of two to four exchanges per year[19].This has a substantial effect on the annual cost for caring for these patients.Polymer stents are also prone to recurrent stenosis as a result of compression from advanced malignancy, retroperitoneal metastases,or encrustation.Metal stents are able to resist lumen occlusion from extrinsic compression,allowing for the longer indwelling times.
According to a prospective study of 21 Resonance stent and 15 polymer stented patients,the mean charges for a single polymer stent and metal stent change are US$6072.75 and US$9469.50,respectively[19].The prices include hospital charges related to stent cost and surgery, including anesthesia,fluoroscopy,pharmaceuticals,and surgeon charges.Annually,the price range for a polymer stent change was estimated to be between US$18,218.25-US$36,436.50.The cost depends on the number of exchanges that occur within a year,with the lower end at three exchanges and the upper end at six exchanges annually.A significant financial reduction by 48%-74%occurs when compared to the annual price of a metal stent.This cost analysis excluded patients with a life expectancy of less than 6 months.The median duration of the Resonance stent was 12 months(range,2-32 months). With the exception of one patient,the resonance stent was tolerated well and no removals or shortening of the indwelling period were required.Overall,success rate of this cohort was 95%.There is a significant financial benefit to having a metal stent able to last 12 months without the risk of encrustation or failure from extrinsic compression [19].
Similarly,Frederick et al.[20]calculated an overall 48% annual cost reduction compared to regular polymeric stent changes.Eighty-six patients had either malignant or benign ureteral obstruction and underwent unilateral or bilateral metalstent placement.The annualcost ofunilateralpolymer placement at 3 and 6 months was determined to be US$16,933.45 and US$8171.00,respectively.Annual cost for metalstents based on mean indwelling duration of7.4 months was US$7859.43.Operating room,anesthesia,medications, fluoroscopy,and stent costs were included.Intangible costs, such as loss of work and productivity were not included in the analyses,butshould be considered as a societalcost.With the inclusion of average loss of wages in their calculation,Baumgarten et al.[21]calculated an even greater cost reduction of up to 59.5%annually with the use ofthe Resonance stentwhen compared to DJS.Theircohortof50 patientshad a failure rate of 8.2%and median stent life of 288.4 days.
Wijayarathna et al.[22]analyzed data on 82 patients who underwent retrograde ureteric stenting for ureteric obstruction related to malignant lesions.They determined elevated serum creatinine over 3 mg/dL and CT evidence of tumor recurrence in the pelvis(p=0.004 and p=0.026,respectively)were indicators of poor outcome.Even if stenting was successful,these patients had a short life expectancy.
9.Nephrostomy tube vs.double J stent
A prospective study by Garg et al.[23]compared the nephrostomy tube and DJS in open pyeloplasty for ureteropelvic junction obstruction hydronephrosis of 40 children ages 2 months to 12 years.Although this study did not study MUO,we wanted to illustrate a head-to-head study of PCN vs.DJS.Minor complications seen in DJS for this study included UTI,increased urinary frequency,distal protrusion into posterior urethra,and dysuria.Other complications that can result from a DJS are mild to moderate flank pain,mechanical irritation of the bladder trigone,urinary urgency,bladder spasm,hematuria,mild pelvic discomfort, urinary urgency,encrustation,pyelonephritis,and incontinence.One major complication that occurred for the DJS group was proximal migration with urinoma formation. Stent migration into the urethra past the external sphincter can result in incontinence.
The authors noted that the optimal stent length could avoid several post-operative problems secondary to migration and bladder irritation.The formula proposed to determine length was:
Length of DJS(cm)=Length of retained ureter(cm)-2
Minor complications seen in the PCN group include tube blockage,urinary leakage a few days after tube removal,persistent urine leak after tube removal,and increased urinary frequency.Breakage of the tube during removal in one patient was the only major complication with the PCN group.Drainage function in both groups showed similar improvement.Those with nephrostomy tubes had a longer hospital stay(3-25 days for DJS group vs.10-16 days for PCN group;p=0.001);however,they incurred an overall lower cost as DJS require removal under anesthesia,resulting in an overall higher mean cost.Patients with nephrostomy tubes preferred to have the tubes removed before discharge due to travel cost and fear of dislodgement.
Song et al.[24]performed a retrospective study reviewing 87 patients bilaterally stented for malignant bilateral ureteral obstruction.If internal stenting failed, the patient was converted to PCN.Twelve of the patients had PCN conversion.Of these,eight had early PCN conversion(<1 year after initial stent)and four had late PCN conversion(after the patient progressed into chronic kidney disease stage 4 or 5)or no conversion.Although a relatively small population was used,they determined that PCN conversion prior to the patient progressing to chronic kidney disease stage 4 or 5,caused a better renal function outcome,than those who had late PCN conversion (p=0.061).This was especially important in patients over the age of 55 years,with diabetes,or poor baseline renal function.Other studies however suggest that PCN placement does not prolong survival for patients with advanced cancer[25].Cancer status was the most causative factor related to stent failure in this study[24].
10.Nephrostomy tube vs.extra anatomic stent
Palliative urinary diversions can be done by either PCN or EAS.The difference is that the nephrostomy tube drains through an external bag,whereas an EAS is internal.PCN tubes are placed in situations where EAS and other procedures have failed.For the insertion of an EAS,a new or existing nephrostomy tract can be used.Therefore,these two interventions can be done in sequence.Patients are usually discharged the day of surgery or the following day.The EAS procedure is not without its faults and it can be time-consuming,and cumbersome for the patient. Stent implantation can also be challenging.Kimuli et al. [16]followed 27 patients for 12 months and noticed an improvement in the mean QoL from 3.4±1.4 preoperatively to 7.6±1.0 postoperatively.
Nephrostomy tubes are changed regularly at 3 months, which is significantly shorter than the 12 months an EAS can stay indwelling.The mean duration for an EAS was 7.5 months(range of 3-18 months)[16].Due to the external method of drainage in PCN the QoL of the patient is compromised.Therefore,PCN is not ideal for long-term treatment and consideration should be given for changing to an EAS.
11.Factors predicting stent failure
11.1.Metal stent
Possible risk factors for Resonance stent failure include age,sex,degree of hydronephrosis,treatment for cancer, occurrence of UTI,serum creatinine,and cancer type.Of these,age≥60 years and serum creatinine level≥2 mg/dL were associated with shorter stent duration[26].In this retrospective study,117 Resonance stents where placed in 79 cancer patients with MUO.When age and serum creatinine level were controlled for,lower gastrointestinal(GI) cancer showed a lower risk of stent failure than GU cancer (p=0.0494).Therefore,cancer type may also be a significant indicator.They hypothesized that lower GI cancers reduce the compression on the stent as they have softer texture and composition.Overall,lower GI cancer,younger age,and low serum creatinine levels are good indicators to stent.Stent failure due to high pre-operative serum creatinine may be a result of poor urine production promoting encrustation and thus shortening the stent duration. The median duration of the resonance stent in this study was 5.77 months.Insertion of metal stent was done after the regular polymeric stent failed.This could be the reason for the shorter stent duration seen in this study,as hydronephrosis had already developed and the cancer likely progressed.The authors found that neither severe hydronephrosis nor peritoneal carcinomatosis were associated with stent failure.However,increased level of obstruction was associated with stent failure.Since the Resonance stent in this study was not inserted as soon as hydronephrosis developed,there is a potential selection bias in this cohort.
11.2.Regular polymeric stent
Yu et al.[1]assessed performance status,type of cancer, hydronephrosis grade location of the obstruction,presence of bladder invasion,C-reactive protein,serum albumin,and inflammation-based prognostic score(Glasgow prognostic score,GPS)of the cystoscopic ureteral stent(Endo-sof, Cook Urological,Spencer,IN,USA).They performed a retrospective study including 71 patients with MUO due to nonurological cancers undergoing stent placement.According to their multivariate analysis,preoperative serum creatinine level of>1.2 mg/dL,GPS≥1,and presence of a mid or lower ureteral obstruction(over or below the sacroiliac joint)were associated with shorter stent duration (p=0.044,0.001,and 0.007,respectively).The medianstent survival and overall survival were 5 and 7.7 months, respectively.
12.Conclusion
MUO can be handled by DJS,tandem DJS,PCN tubes,metal ureteral stents,or EAS.The predictors of failure are those of advanced cancer progression.The QoL between modalities is similar and consideration must be given to the frequency of exchange,the cost of exchange procedures,and the difference in urinary symptoms between the different modalities.None of these have been shown to completely extend the life of patients(from cancer),but do preserve renal function in order for them to receive treatment modalities such as chemotherapy or surgery.The modalities available to physicians are varied and depend on access to each modality at each site.
Conflicts of interest
Kristina Pavlovic has none to declare.Dirk Lange is the consultant for Bard Medical,Boston Scientific Corporation, Cook Medical,and Urotech.Ben H.Chew is the consultant for ADVA-Tec,AurisSurigcal,Bard Medical,Boston Scientific Corporation,Cook Medical,Olympus Medical.
[1]Yu SH,Ryu JG,Jeong SH,Hwang EC,Jang WS,Hwang IS,et al. Predicting factors for stent failure-free survival in patients with a malignant ureteral obstruction managed with ureteral stents.Korean J Urol 2013;54:316-21.
[2]Chung HH,Kim MD,Won JY,Won JH,Cho SB,Seo TS,et al. Multicenter experience of the newly designed covered metallic ureteral stent for malignant ureteral occlusion: comparison with double J stent insertion.Cardiovasc Interv Radiol 2013;37:463-70.
[3]Chow PM,Chiang IN,Chen CY,Huang KH,Hsu JS,Wang SM, et al.Malignant ureteral obstruction:functional duration of metallic versus polymeric ureteral stents.PLoS One 2015;10: e0135566.
[4]Kulkarni R.Metallic stents in the management of ureteric strictures.Indian J Urol 2014;30:65-72.
[5]Kim KS,Choi S,Choi YS,Bae WJ,Hong SH,Lee JY,et al. Comparison of efficacy and safety between a segmental thermo-expandable metal alloy spiral stent(Memokath 051) and a self-expandable covered metallic stent(UVENTA)in the management of ureteral obstructions.J Laparoendosc Adv Surg Tech A 2014;24:550-5.
[6]Kadlec AO,Ellimoottil CS,Greco KA,Turk TM.Five-year experience with metallic stents for chronic ureteral obstruction.J Urol 2013;190:937-41.
[7]Chow PM,Hsu JS,Wang SM,Yu HJ,Pu YS,Liu KL.Metallic ureteral stents in malignant ureteral obstruction:short-term results and radiological features predicting stent failure in patients with non-urological malignancies.World J Urol 2014; 32:729-36.
[8]Abbasi A,Wyre HW,Ogan K.Use of full-length metallic stents in malignant ureteral obstruction.J Endourol 2012;27: 640-5.
[9]Elsamra SE, Motato H, Moreira DM, Waingankar N, Friedlander JI,Weiss G,et al.Tandem ureteral stents for the decompression of malignant and benign obstructive uropathy. J Endourol 2013;27:1297-302.
[10]Varnavas M,Bolgeri M,Mukhtar S,Anson K.The role of tandem double-J ureteral stents in the management of malignant ureteral obstruction.J Endourol 2016;30:465-8.
[11]Allen DJ,Longhorn SE,Philp T,Smith RD,Choong S.Percutaneous urinary drainage and ureteric stenting in malignant disease.Clin Oncol R Coll Radiol 2010;22:733-9.
[12]Alawneh A,Tuqan W,Innabi A,Al-Nimer Y,Azzouqah O, Rimawi D,et al.Clinical factors associated with a short survival time after percutaneous nephrostomy for ureteric obstruction in cancer patients:an updated model.J Pain Symptom Manag 2016;51:255-61.
[13]Monsky WL,Molloy C,Jin B,Nolan T,Fernando D,Loh S,et al. Quality-of-life assessment after palliative interventions to manage malignant ureteral obstruction.Cardiovasc Interv Radiol 2013;36:1355-63.
[14]Ishioka J,Kageyama Y,Inoue M,Higashi Y,Kihara K.Prognostic model for predicting survival after palliative urinary diversion for ureteral obstruction:analysis of 140 cases.J Urol 2008; 180:618-21.discussion 21.
[15]Azuma T,Nagase Y,Oshi M.Prognostic marker for patients with malignant ureter obstruction.Clin Genitourin Cancer 2013;11:353-6.
[16]Kimuli M,Sciberras J,Lloyd S.In:Go¨"oz PM,editor.Extraanatomic urinary drainage for urinary obstruction,chronic kidney disease.Rijeka,Croatia:InTech;2012.p.281-96. http://dx.doi.org/10.5772/23049.
[17]Chung KJ,Park BH,Park B,Lee JH,Kim WJ,Baek M,et al. Efficacy and safety of a novel,double-layered,coated,selfexpandable metallic mesh stent(Uventa)in malignant ureteral obstructions.J Endourol 2013;27:930-5.
[18]Kim KH,Cho KS,Ham WS,Hong SJ,Han KS.Early application of permanent metallic mesh stent in substitution for temporary polymeric ureteral stent reduces unnecessary ureteral procedures in patients with malignant ureteral obstruction. Urology 2015;86:459-64.
[19]Taylor ER,Benson AD,Schwartz BF.Cost analysis of metallic ureteral stents with 12 months of follow-up.J Endourol 2012; 26:917-21.
[20]Frederick L,Kadlec AO,Shah A,Ellimoottil CS,Turk TM, Schwartz BF.Cost analysis of metallic stents for chronic ureteral obstruction:a multi-center study.J Urol Clin Pract 2016 [in press].
[21]Baumgarten AS,Hakky TS,Carrion RE,Lockhart JL,Spiess PE. A single-institution experience with metallic ureteral stents:a cost-effective method of managing deficiencies in ureteral drainage.Int Braz J Urol 2014;40:225-31.
[22]Wijayarathna S,Suvendran S,Ishak M,Weligamage A,Epa A, Munasinghe S,et al.Outcome of retrograde ureteric stenting as a urinary drainage procedure in ureteric obstruction related to malignant lesions.Ceylon Med J 2015;59:124-7.
[23]Garg RK,Menon P,Narasimha Rao KL,Arora S,Batra YK. Pyeloplasty for hydronephrosis:issues of double J stent versus nephrostomy tube as drainage technique.J Indian Assoc Pediatr Surg 2015;20:32-6.
[24]Song SH,Pak S,Jeong IG,Kim KS,Park HK,Kim CS,et al. Outcomes of stent-change therapy for bilateral malignancyrelated ureteral obstruction.Int Urol Nephrol 2014;47: 19-24.
[25]Kouba E,Wallen EM,Pruthi RS.Management of ureteral obstruction due to advanced malignancy:optimizing therapeutic and palliative outcomes.J Urol 2008;180:444-50.
[26]Chow PM,Hsu JS,Huang CY,Wang SM,Lee YJ,Huang KH, et al.Metallic ureteral stents in malignant ureteral obstruction:clinical factors predicting stent failure.J Endourol 2014; 28:729-34.
Received 2 March 2016;received in revised form 14 April 2016;accepted 26 April 2016 Available online 13 May 2016
*Corresponding author.
E-mail address:ben.chew@ubc.ca(B.H.Chew).
Peer review under responsibility of Second Military Medical University.
http://dx.doi.org/10.1016/j.ajur.2016.04.002
2214-3882/?2016 Editorial Office of Asian Journal of Urology.Production and hosting by Elsevier B.V.Ltd.This is an open access article under the CC BY-NC-ND license(http://creativecommons.org/licenses/by-nc-nd/4.0/).
obstruction;
Ureteral stent;
Hydronephrosis
 Asian Journal of Urology2016年3期
Asian Journal of Urology2016年3期
- Asian Journal of Urology的其它文章
- Robot-assisted laparoscopic radical cystectomy with complete intracorporeal urinary diversion
- Current status of laparoscopic and robotassisted nerve-sparing radical cystectomy in male patients
- Percutaneous resection of upper tract urothelial cell carcinoma:When,how, and is it safe?
- Techniques to resect the distal ureter in robotic/laparoscopic nephroureterectomy
- Thulium laser treatment for bladder cancer
- Narrow band imaging for bladder cancer
