Gait deterioration due to neural degeneration of the corticoreticular pathway: a case report
IMAGING IN NEURAL REGENERATION
Gait deterioration due to neural degeneration of the corticoreticular pathway: a case report
The corticoreticular pathway (CRP) mainly mediates proximal and axial muscles and therefore it is an important neural tract for walking (Miyai et al., 2002; Matsuyama et al., 2004; Mendoza and Foundas, 2007). Diffusion tensor tractography (DTT), derived from diffusion tensor imaging (DTI), enables reconstruction of the CRP three-dimensionally and several studies have reported on the association between the CRP and gait recovery (Yeo et al., 2012a, 2013; Jang et al., 2013, 2015; Jang and Seo, 2014; Kwon and Jang, 2014). However, to the best of our knowledge, there has been no report on degeneration of the CRP. In the current study, we reported on a patient with intracerebral hemorrhages (ICHs) in both hemispheres, presenting with gait deterioration due to neural degeneration of the CRP as shown on DTT images.
A 64-year-old male presented with gait deterioration which started 2 months ago. He had a history of spontaneous ICHs in both putamens (the right ICH: 19 years ago, and the left ICH: 11 years ago). The patient’s motor weakness was measured using Medical Research Council (MRC) scale (Council, 1976). His walking ability was assessed using Functional Ambulatory Category (FAC) (Cunha et al., 2002).
Before the onset of gait deterioration, his motor function had recovered to a subnormal state in the right extremities and a nearly normal state in the left extremities; therefore, he was able to walk independently, even on stairs (FAC: 4). Since about 2 months ago, his gait function had begun to deteriorate and aggravated progressively with time. Two months after the onset of gait disturbance, he could not walk independently, even on floors (FAC: 1.5). He presented with weakness of proximal joints along with more severe weakness in the right extremities compared with the left side (MRC scale, shoulder abductor: 4—/4, elbow flexor: 4/4+, finger extensor: 4/4+, hip flexor: 4—/4, knee extensor: 4/4+, ankle dorsiflexor: 4/4+) (Council, 1976). Brain MR images taken at 2 months after onset of gait deterioration showed leukomalactic lesions in both subcortical white matter and basal ganglia (Figure 1B).
DTI data were obtained twice (first DTI: 6 years ago and second DTI: 2 months after onset of gait deterioration). Sixty contiguous slices (field of view = 240 × 240 mm2; repetition time = 10,726 ms; echo time = 76 ms; b = 1,000 s/mm2; number of excitations = 1; and thickness = 2.5 mm) were acquired. FACT algorithm was used for fiber tracking. The CRP was reconstructed using fibers passing through two regions of interest (ROIs) on the color map. The first ROI was given at the medullary reticular formation and the second ROI at the midbrain tegmentum. Termination criteria used for fiber tracking were fractional anisotropy (FA) of less than 0.2 and angle of less than 60°.
On the first DTT scan performed 6 years ago, the integrities of the CRPs in both hemispheres were preserved from the cerebral cortex to the medulla. By contrast, on the second DTT taken at 2 months after onset of gait deterioration, both CRPsshowed discontinuation at the corona radiata level compared with the first DTT (Figure 1C).
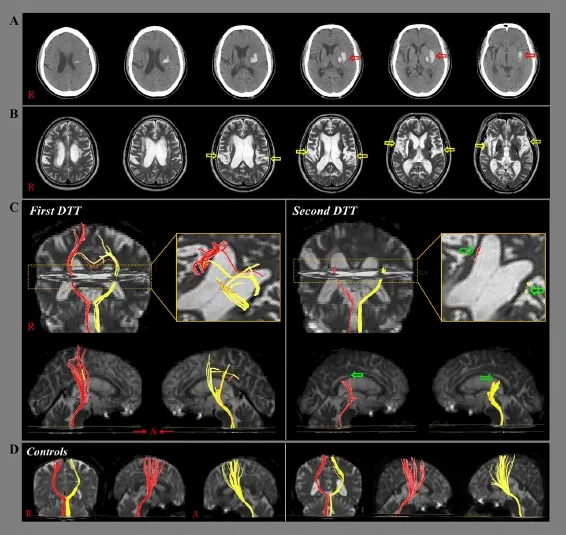
Figure 1 Brain CT and MR images and results of diffusion tensor tractography (DTT) in a 64-yearold male patient with gait deterioration.
In this study, the gait deterioration in this patient was ascribed to delayed neural degeneration of both CRPs.
The patient began to show gait deterioration 2 months ago, before undergoing the second DTT. The second DTT for the CRP, taken at 2 months after onset of gait deterioration, showed discontinuations at the corona radiata compared with the first DTT (6 years ago), which showed that integrities of both CRPs were intact. This finding was consistent with the characteristics of motor weakness of the patient (more severe weakness of proximal muscles) (Matsuyama et al., 2004; Mendoza and Foundas, 2007; Yeo et al., 2013). Regarding the pathophysiological mechanism of delayed neural degeneration of the CRP in the corona radiata, injury of peri-lesional white matter might occur through a chemical mechanism: a blood clot might release potentially toxic substances which can induce injury to neural tissue, such as free iron, which might release free radicals or inflammatory cytokines (Chua et al., 2009; Yeo et al., 2012b). However, other factors that can deteriorate the gait function such as normal aging or physical deconditioning should be also considered.
Accompanying neural degeneration is often observed after stroke (Yu et al., 2009; Puig et al., 2010). Many studies have reported on Wallerian degeneration that started immediately after neuronal injury in the acute stage of stroke (Yu et al., 2009; Puig et al., 2010). Wallerian degeneration is a process characterized by degeneration of axons and their distal part myelin sheath in the central and peripheral nervous system. However, little is known about delayed neural degeneration in stroke patients. To the best of our knowledge, this is the first study to report on neural degeneration of the CRP although a few previous studies have reported on neural degeneration of the CST in stroke patients (Radlinska et al., 2009; Jang ans Seo, 2016). However, DTI might underestimate the neural fibers due to the fiber-crossing effect (Yamada et al., 2009), which should be considered.
In conclusion, we report on a patient who showed delayed gait deterioration due to neural degeneration of the CRP. We believe that DTT evaluation of the CRP would be helpful to elucidate the mechanism behind delayed gait deterioration in stroke patients.
This work was supported by the National Research Foundation (NRF) of Korea Grant funded by the Korean Government (MSIP), No. 2015R1A2A2A01004073.
Sung Ho Jang, Han Do Lee*
Department of Physical Medicine and Rehabilitation, College of Medicine, Yeungnam University, Namku, Daegu, Republic of Korea
*Correspondence to: Han Do Lee, M.S., lhd890221@hanmail.net.
Accepted: 2015-10-20
orcid: 0000-0002-1668-2187 (Han Do Lee)
Chua CO, Chahboune H, Braun A, Dummula K, Chua CE, Yu J, Ungvari Z, Sherbany AA, Hyder F, Ballabh P (2009) Consequences of intraventricular hemorrhage in a rabbit pup model. Stroke 40:3369-3377.
Council MR (1976) Aids to the Examination of the Peripheral Nervous System. London, HMSO: American printing.
Cunha IT, Lim PA, Henson H, Monga T, Qureshy H, Protas EJ (2002) Performance-based gait tests for acute stroke patients. Am J Phys Med Rehabil 81:848-856.
Jang SH, Seo JP (2014) The distribution of the cortical origin of the corticoreticular pathway in the human brain: a diffusion tensor imaging study. Somatosens Mot Res 31:204-208.
Jang SH, Seo JP (2016) Delayed leg weakness due to peri-lesional neural degeneration in a patient with intracerebral haemorrhage: case report. Acta Neurol Belg 116:91-93.
Jang SH, Chang CH, Lee J, Kim CS, Seo JP, Yeo SS (2013) Functional role of the corticoreticular pathway in chronic stroke patients. Stroke 44:1099-1104.
Jang SH, Choi BY, Kim SH, Chang CH, Jung YJ, Yeo SS (2015) Injury of the corticoreticular pathway in subarachnoid haemorrhage after rupture of a cerebral artery aneurysm. J Rehabil Med 47:133-137.
Kwon HG, Jang SH (2014) Delayed gait disturbance due to injury of the corticoreticular pathway in a patient with mild traumatic brain injury. Brain Inj 28:511-514.
Matsuyama K, Mori F, Nakajima K, Drew T, Aoki M, Mori S (2004) Locomotor role of the corticoreticular-reticulospinal-spinal interneuronal system. Prog Bain Res 143:239-249.
Mendoza JE, Foundas AL (2007) Clinical neuroanatomy: a neurobehavioral approach. New York; London: Springer.
Miyai I, Yagura H, Oda I, Konishi I, Eda H, Suzuki T, Kubota K (2002) Premotor cortex is involved in restoration of gait in stroke. Ann Neurol 52:188-194.
Puig J, Pedraza S, Blasco G, Daunis IEJ, Prats A, Prados F, Boada I, Castellanos M, Sanchez-Gonzalez J, Remollo S, Laguillo G, Quiles AM, Gomez E, Serena J (2010) Wallerian degeneration in the corticospinal tract evaluated by diffusion tensor imaging correlates with motor deficit 30 days after middle cerebral artery ischemic stroke. AJNR Am J Neuroradiol 31:1324-1330.
Radlinska BA, Ghinani SA, Lyon P, Jolly D, Soucy JP, Minuk J, Schirrmacher R, Thiel A (2009) Multimodal microglia imaging of fiber tracts in acute subcortical stroke. Ann Neurol 66:825-832.
Yamada K, Sakai K, Akazawa K, Yuen S, Nishimura T (2009) MR tractography: a review of its clinical applications. Magn Reson Med Sci 8:165-174.
Yeo SS, Kim SH, Jang SH (2013) Proximal weakness due to injury of the corticoreticular pathway in a patient with traumatic brain injury. NeuroRehabilitation 32:665-669.
Yeo SS, Chang MC, Kwon YH, Jung YJ, Jang SH (2012a) Corticoreticular pathway in the human brain: diffusion tensor tractography study. Neurosci Lett 508:9-12.
Yeo SS, Choi BY, Chang CH, Kim SH, Jung YJ, Jang SH (2012b) Evidence of corticospinal tract injury at midbrain in patients with subarachnoid hemorrhage. Stroke 43:2239-2241.
Yu C, Zhu C, Zhang Y, Chen H, Qin W, Wang M, Li K (2009) A longitudinal diffusion tensor imaging study on Wallerian degeneration of corticospinal tract after motor pathway stroke. Neuroimage 47:451-458.
10.4103/1673-5374.180759 http://www.nrronline.org/
How to cite this article: Jang SH, Lee HD (2016) Gait deterioration due to neural degeneration of the corticoreticular pathway: a case report. Neural Regen Res 11(4):687-688.
- 中國神經(jīng)再生研究(英文版)的其它文章
- Complement components of nerve regeneration conditioned fluid influence the microenvironment of nerve regeneration
- Electrical stimulation of dog pudendal nerve regulates the excitatory pudendal-to-bladder reflex
- Supplementary motor area deactivation impacts the recovery of hand function from severe peripheral nerve injury
- Combined use of Y-tube conduits with human umbilical cord stem cells for repairing nerve bifurcation defects
- Senegenin inhibits neuronal apoptosis after spinal cord contusion injury
- Human umbilical cord blood-derived stem cells and brain-derived neurotrophic factor protect injured optic nerve: viscoelasticity characterization

