Lesson Seventy-four An atypical presentation of a typical arrhythmia
●心電學英語
Lesson Seventy-four An atypical presentation of a typical arrhythmia
A 44-year-old man with a long history of a narrow complex tachycardia and prior left lateral accessory pathway(LL-AP) ablation wasbroughtto the electrophysiology laboratory for a redo supraventricular tachycardia(SVT)ablation procedure.Catheters were positioned within the coronary sinus(CS)and right ventricular apex(RVa).The case was performed with the guidance of a 3D mapping system.A long RP tachycardia with a cycle length of 320 ms was easily induced with ventricular extrastimulus.Earliest atrial activation was present in the proximal(9,10)CS electrodes with a ventricular to atrial(VA)time of 140 ms.Ventricular overdrive pacing was consistent with a V-A-V response with a post pacing interval minus tachycardia cycle length(PPI-TCL)of 175 ms,and stimulus to atrial(SA)activity during pacing minus VA activity during tachycardia time of 120 ms(Fig.1A).A premature ventricular complex (PVC) introduced around the time of His-refractoriness did not change the timing of the subsequent atrial activation(Fig.1B).In sinus rhythm,dualatrioventricularnode(AVN)physiology was present and Para-Hisian pacing resulted in a VA time that was 52 ms shorter with His capture than with loss of capture(Fig.2A).What is the possible mechanism of the tachycardia according to these findings?
The differential diagnosis of long RP tachycardia with"concentric"activation is atypical atrioventricular nodal reentrant tachycardia(AVNRT),atrioventricular reentrant tachycardia(AVRT)using a septal pathway as the retrograde limb or atrial tachycardia.The results of ventricular entrainment as well as His-refractory PVC and Para-Hisian pacing excluded atrial tachycardia and were supportive of atypical AVNRT rather than AVRT utilizing septal pathway.Slow pathway modification was therefore performed on the right septum as well as on the left septum and CS ostium.Accelerated junctional rhythm was frequently observed during radiofrequency ablation;however,the tachycardia remained inducible; Was this due to inadequate ablation or a misdiagnosis?
With subsequent tachycardia induction,SVT with a left bundle branch block(LBBB)was present.The TCL and VA time were longer during LBBB compared to the absence of LBBB(Fig.2B),which supported the presence of AVRT utilizing a left-sided AP.Mapping the earliest retrograde atrial activity during SVT was consistent with conduction across an LL-AP.This conduction occurred in the region where the previous LL-AP ablation was performed.As apparent in our local activation time map(Fig.3A),delayed activation of the adjacent mitral annular region was present(purple and blue areas)between the distal pair of the CS electrodes and the atrial pathway insertion,which we hypothesized was due to the presence of mitral isthmus conduction block from the prior ablation procedure.The presence of mitral isthmus block was demonstrated during tachycardia and in sinus rhythm.A single ablation lesion at the site with earliest atrial activation during SVT(Fig.3B)terminated the tachycardia within 4 seconds and rendered it noninducible at 30 minutes of wait time.The patient had no recurrence of arrhythmia 1 year postprocedure.
Commentary
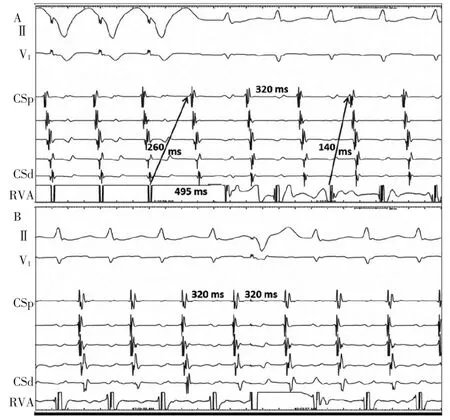
Figure 1 A:RVa overdrive pacing with tachycardia entrainment.The atrial activation in the CS occurs from the proximal to distal electrodes.Upon cessation of RVa pacing a V-A-V response is noted.PPI-TCL=175 ms and SA-VA=120 ms.B:His-refractory PVC introduced during tachycardia.There is no change in atrial activation timing.CS= coronary sinus;PPI=postpacing interval;PVC=premature ventricular complex;RVa=right ventricular apex;SA= stimulus to atrial;TCL=tachycardia cycle length;VA=ventricular to atrial.
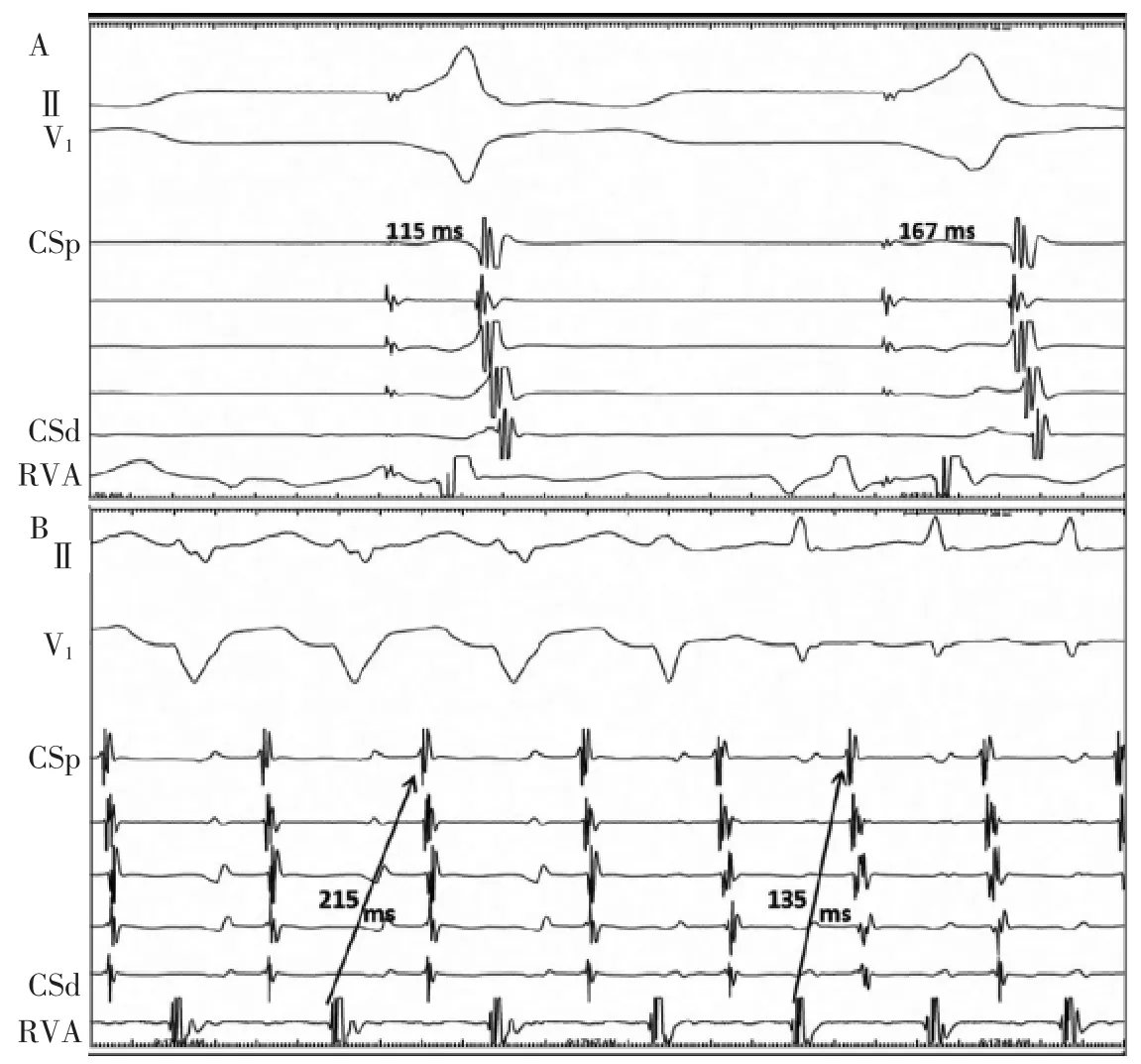
Figure 2 A:Pacing in the His region.The QRS of the first beat is narrow due to His capture whereas RV capture only is present in the second beat as evident by widening of the QRS.The VA time was 52 ms longer with His loss of capture suggesting the absence of a septal AP.B:The tachycardia cycle length and VA time are longer with LBBB compared to a narrow QRS consistent with a positive Coumel's sign1.Please note that the minor change in coronary sinus(CS)activation observed in Panels(A)and(B)are related to movement of the CS catheter during the procedure.AP= accessory pathway;LBBB=left bundle branch block;RV=right ventricular;VA=ventricular to atrial.
This case highlights the diagnostic challenge that occurs in case of recurrence of LL-AP in the setting ofmitral annular block.Recurrence of LLAP conduction after a successful ablation has been reported to be as low as 2%-5%.Rarely,conduction across an LL-AP can occur with reversal of the activation sequence on the CS electrodes.The most commonly accepted mechanism to explain this phenomenon is the presence of left intraatrial block,which can inadvertently be created during LL-AP ablation.This block is similar to a block that can intentionally be created between the lateral mitral annulus and a left inferior pulmonary vein when targeting atrial fibrillation or mitral annular flutter.In the largest published series of patients undergoing LL-AP ablation,approximately 7%had conduction block in this region prior to successful ablation of the AP.When block is created,the activation within the left atrium can change and appears earliest in the proximal CS electrodes during SVT or RVa pacing.A"double potential"can be recorded on the CS catheter as it crosses the block line.Unfortunately in our case we could not"bracket"the block line due to a venous valve. An alternative possible mechanism to explain the reversal of the activation on the CS electrodes is disconnection between the left atrium and the distal portion of the CS musculature during ablation at the LL-AP region.This,however,can only occur in specific conditions in which the only discrete musculature connections between the CS and left atrium are at the distal CS(which have been disconnected)and the proximal electrodes.
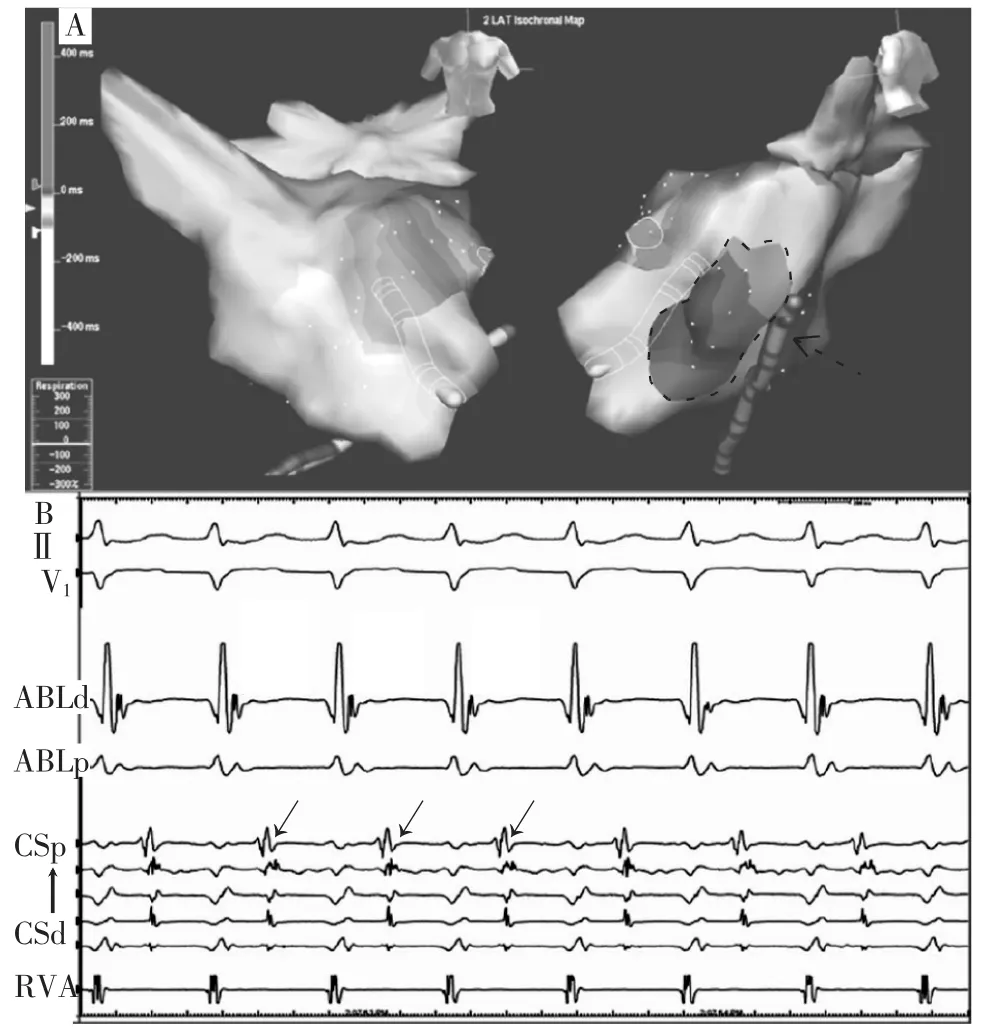
Figure 3 A:Local activation time map of retrograde atrial activity during tachycardia.Earliest activation(white)occurs at two o'clock on the mitral annulus.Delayed conduction or conduction block is apparent on the local activation timing map as illustrated by later atrial activity(dashed arrow and dotted line area)adjacent to the earliest atrial activity(white color).B:Local electrogram recordings at the site with earliest atrial activity(arrows point to the local atrial recordings).Ablation at this site eliminated the tachycardia within 4 seconds.
To avoid the confusion that can occur in this setting,a few points should be kept in mind.First, conduction across recurrent LL-AP should always be entertained even in the absence of eccentric retrograde atrial conduction with RVa pacing and SVT when prior ablation has been performed in this region.Second,the PPI upon cessation of SVT entrainment from the RV,the response to His-synchronous PVC2,and para-Hisian pacing maneuvers are fundamentally related to the AP's conduction properties,distance from the AVN,as well as the distance of the pacing site from the circuit during tachycardia.Although the presence of a septal AP, which is close to the AVN,may be ruled out with the results of these maneuvers,an LL-AP may not be with these maneuvers3.This is less of an issue in the presence of eccentric VA conduction,which is not the case when concomitant mitral annular block is present. Operators must keep this point in mind when testing for success after an initial LL-AP ablation to ensure inadvertent mitral annular block is not misinterpreted as successful AP elimination. Noteworthy is the significance of positive Coumel's sign in this case. Although other findings did not rule out LL-AP presence,this sign was diagnostic.
In conclusion,negative findings on electrophysiology studies may not necessarily be reassuring,whereas positive findings can be diagnostic.Mapping the earliest retrograde atrial activation during SVT may allow an operatorto simultaneously demonstrate both the insertion site of the AP and location of block.

