Astrocytes in the cerebral cortex play a role in the spontaneous motor recovery following experimental striatal hemorrhage
Intracerebral hemorrhage (ICH) is a stroke subtype caused by spontaneous rupture of small vessels and bleeding into the brain parenchyma, resulting in cell death and sensorimotor deficits. Despite the greater prevalence of the ischemic form of stroke (87%), ICH has the highest mortality rate of all stroke subtypes. The striatum is the most affected structure in hemorrhagic stroke (35–70%), followed by cerebral cortex (15–30%), brain stem and cerebellum (5–10%); patients suffering striatal and/or cortical ICH bear persistent sensorimotor disabilities. Although chronic sensorimotor impairment is established, a considerable amount of patients experience some degree of spontaneous recovery during thefirst six months after stroke (Qureshi et al., 2009), and the neurobiological basis of this process is not understood.
Spontaneous motor recovery is also one of the hallmarks of experimental stroke, and cellular mechanisms of plasticity appear to involve coordinated neuronal changes such as regulation of growth factors,increase in protein synthesis and reorganization of the cortical maps(Adkins et al., 2006). There is also evidence that astrocytes may play a role in this complex phenomenon (Hayakawa et al., 2010; Neves et al., 2017). Both experimental ischemic and hemorrhagic stroke in rodents induces similar changes in astrocyte morphology. However, the known differences as regards to the pathophysiology of ischemic and hemorrhagic stroke influencing lesion recovery, mainly attributed to the brain plasticity and the activation of remote brain areas (Mestriner et al., 2015), indicate that glial mechanisms triggered by either form of stroke need further investigation.
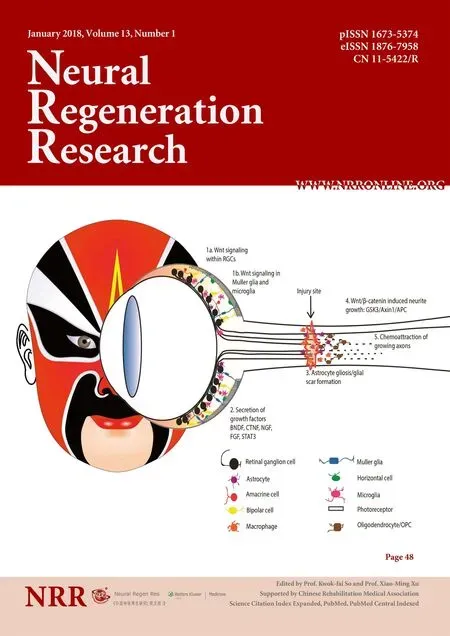
The remodeling of the injured brain parenchyma after ICH is a graded and multi-stage process involving a wide range of molecules and morphological changes. It is a defensive process to adapt the brain microenvironment in response to injury. Reactive astrocytes surround and isolate the damaged tissue generating a “yin/yang-like”effect (Burda and Sofroniew, 2014): on the one hand, isolation of the damaged tissue is protective to minimize the injury size, to restrict inflammation, to stimulate the blood-brain barrier repair and to counteract edema; all these may influence blood flow and thus contribute to functional reestablishment of the remaining tissue. On the other hand, exacerbated astrocyte reactivity may activate molecular mechanisms leading to glial scar formation that can disrupt axonal sprouting and circuits rewiring (Burda and Sofroniew, 2014).
Glial-related changes after ICH have been mainly investigated in the perilesional tissue, however the functional connections between the striatum and the cerebral cortex suggest that spontaneous recovery after ICH might encompass injury response in both structures(Hamzei et al., 2012; Neves et al., 2017). Interestingly, it was recently shown that intrastriatal hemorrhage causes similar increase of GFAP-positive cell and expression, up to seven days post-event, in both the damaged striatum and the ipsilateral cerebral cortex (Neves et al., 2017). The development of reactive gliosis, characterized by the increased GFAP, as well as the activation of cortical plasticity,may explain the highest degree of motor recovery after hemorrhagic stroke as compared to ischemic ones (Mestriner et al., 2015).
The cerebral cortex is a highly specialized and plastic brain structure that contributes to post-injury recovery through changes in its excitability (Adkins et al., 2006). For instance, a previous study has suggested that the partial spontaneous recovery of ICH patients is probably due to their cerebral cortex integrity (Kelly et al., 2003), as well as to new structural and functional circuits that can be formed through cortical remapping after lesion. Since the brain is heavily interconnected, there are many alternate pathways to be used; indeed,brain imaging studies after stroke support that the best recovery is reached whenever closely related circuits are re-engaged in sensorimotor activities affected by the injury (Adkins et al., 2006). In the same way, motor areas of the cerebral cortex exert influence on the dorsolateral striatum, as it is demonstrated that motor skill training engage both structures in a highly interdependent way (Hamzei et al., 2012).Moreover, synchronous neuronal activity was shown to induce a signal for post-infarct axonal sprouting initiated at the intact contralateral cortical hemisphere that benefits the peri-damaged cortex after focal ischemic stroke in rodents (Carmichael and Chesselet, 2002).Additionally, the loss of cortical input to the dorsolateral striatum on the lesion side induces axonal sprouting at the contralateral corticostriatal input in rats, and the sprouting or overactivity of the contralateral projections contribute to the changes in gene expression in the striatum following cortical injury (Napieralski et al., 1996). Taken together, these studies indicate that lesions to striatum or to cerebral cortex may elicit responses in both structures in a functional-related way, and that glial cells may participate in plastic mechanisms involved in spontaneous motor recovery.
T he increase of cortical GFAP expression due to astrocyte hyperplasia and hypertrophy participate on the mechanisms of brain repair after striatal ICH (Neves et al., 2017). Astrocytes secrete synaptogenic molecules that are thought to contribute to the remodeling of neural circuits and to be beneficial for functional recovery after stroke. Following brain injury, reactive astrocytes might revert to an immature functional state but still expressing molecules that induce synapse remodeling. They show changes in morphology that might directly influence the adaptive responses of neighboring neurons in the peri-damaged tissue. Astrocytes and neurons operate in a synergic way, by which astrocytes can regulate the synaptic microenvironment in response to increased neuronal activity (Burda and Sofroniew,2014). They prevent the progression of glutamate excitotoxicity and cellular death through the process of removing the excess of extracellular glutamateviaglutamate transporters present in astrocyte plasma membrane.
Reactive astrocytes also increase axonal remodeling of corticospinal tract and facilitate the promotion of neurite extension and growth,and remyelination (Liu et al., 2014). Upregulation and secretion of many neurotrophic factors during the development of reactive astrogliosis promote the survival of neurons, oligodendrocytes, and neural precursor cells, as well as induce the migration of oligodendrocytes precursors cells into the lesion site favoring proper remyelination(Liu et al., 2014). In agreement, pharmacologic attenuation of astrocyte reactivity by the use of fluorocitrate, a citric acid cycle inhibitor,impaired behavioral/functional recovery in rodents, possibly due to the decrease of high-mobility group box 1 protein-positive astrocytes,a biomarker of reactive astrogliosis and neurovascular remodeling(Hayakawa et al., 2010). Therefore, reactive astrocytes may contribute to the modulation of brain plasticity and recovery after ICH. Considering the above discussed interplay between cerebral cortex and striatum after ICH, it is possible to suggest that astrocyte activity might reveal the existence of a neurochemical “cortico-striatal” unit.
Conversely, the establishment of the glial scar has negative effects on neural repair, as seen in various conditions such as head trauma,stroke, multiple sclerosis and others brain injuries. Glial scar tissue has been shown to release a variety of inhibitory molecules that prevent axon regeneration, as myelin inhibitory molecules, chondroitin sulfate proteoglycans, ephrins and semaphorins. After the injury,reactive astrocytes release great amounts of these mediators leading to their extensive deposition in the scar extracellular matrix (Burda and Sofroniew, 2014). Reactive astrogliosis can also increase lesion size through the production of pro-inflammatory molecules, by increasing the oxidative stress and reducing beneficial effects of neurotrophic factors that promote brain plasticity and recovery. Indeed, for many years, the reactive astrocyte was thought to be anti-regenerative when responding to a brain injury (Burda and Sofroniew, 2014).
The balance between the positive and the negative effects of reactive astrogliosis are possibly dependent on the time window, the local environment and the extent of brain lesion after stroke (Burda and Sofroniew, 2014). In thefirst recovery phase, acute/subacute, following ICH astrocytes are able to recruit and stimulate inflammatory and immune cells and to initiate debris removal; the major increase of inflammatory cytokines might be involved in the process of cellular death. This is a very critical point, since microglia may drive the functioning of reactive astrocytes; for instance, acute proinflammatory factors such as interleukin-1, interleukin-6, and tumor necrosis factor-alpha are closely related with microglia activation and the further enhancement of reactive astrogliosis. However, as from the second recovery phase on (subacute/chronic), astrocytes contribute to tissue repair and remodeling through cellular proliferation, migration,tissue regeneration and long-lasting tissue stabilization. It is postulated that, during this later stage, neural stem cells give rise to neural progenitors that migrate to the injury sites in cortex or striatum to form the cells of perilesional area, so contributing to tissue repair and remodeling (Burda and Sofroniew, 2014).
Although reactive astrogliosis shows controversial effects, it seems clear that astrocytes play a key role during brain remodeling after injury. The promotion of synaptic plasticity underlying functional recovery is affected by the release of gliotransmitters that may modify synaptic networks to the plastic mode during states of rehabilitative training in the cerebral cortex of lesioned animals (Hirase et al.,2014). In fact, cortical astrocytes may act as gliovascular units regulating neuronalfiring threshold through synchronized glial signaling,coordinating neuronal production, network insertion, phenotype and functional activity (Hirase et al., 2014). Thus, we can hypothesize that astrocyte reactivity in cerebral cortex might be important to the extent of sensorimotor recovery after ICH. It seems likely that reactive astrogliosis observed in the cerebral cortex after ICH may, in fact, influence the primary lesion environment and act synergistically with the striatum in an attempt to reorganize and repair the injured area, working as a “cortico-striatal unit”. The increased activation of secondary areas, as the sensorimotor cortex, connected to the injured zones, as striatum, can strength the synaptic microenvironment contributing to spontaneous motor recovery (Hamzei et al., 2012). Considering that available evidence comes from experimental studies, it is now important to conduct human studies aiming to support the existence of a functional role of cortical astrocytes in the suggested “cortico-striatal unit” scenario. Whether proved, this working hypothesis will contribute to move forward thefield of neurorehabilitation after stroke.
Conclusions:The complexity of reactive astrocytosis and its dual,positive and negative, effects in the perilesional neural tissue after brain injury points to its importance on brain homeostasis. Interestingly, a recent investigation from our research group shows that astrocytes in cerebral cortex and striatum are closely and similarly affected after intrastriatal hemorrhage, and suggests that cortical changes are related to spontaneous motor recovery. The working hypothesis here discussed is that there is a “cortico-striatal unit” in terms of astrocyte reactivity, which might be important for brain plasticity and remodeling.
Future directions:Experimental interventions to selectively block cortical reactive astrocytosis in the subacute/chronic phase of ICH would prove the validity of presented hypothesis. An ideal astrocyte management in the “cortico-striatal unit” may combine different mechanisms of initiation and progression of astrocyte reactivity encompassing other players in another important “unit”,the neurovascular.
Juliana Dalibor Neves*, Régis Gemerasca Mestriner,Carlos Alexandre Netto
Graduate Program of Physiology, Institute of Basic Health Sciences,
Universidade Federal do Rio Grande do Sul, Porto Alegre, RS,Brazil (Neves JD, Netto CA)
Department of Biochemistry, Institute of Basic Health Science,Universidade Federal do Rio Grande do Sul, Porto Alegre, RS,Brazil (Neves JD, Netto CA)
Neurorehabilitation and Neural Repair Research Group, Pontifícia Universidade Católica do Rio Grande do Sul, Porto Alegre, RS,Brazil (Mestriner RG)
*Correspondence to:Juliana Dalibor Neves, Ph.D.,julianadn@gmail.com.
orcid:0000-0001-8035-755X (Juliana Dalibor Neves)
Plagiarism check:Checked twice by iThenticate.
Peer review:Externally peer reviewed.
Open access statement:This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under identical terms.
Open peer review report:
Reviewer: Ilias Kazanis, University of Cambridge, UK.
Comments to authors: The review submitted by Neve et al. touches upon an interesting and novel aspect of the biology of regeneration: the role of astrocytes in the remodeling of the perilesional tissue after stroke. The focus on the corticostriatal remodeling nicely highlights their recent experimental work.
Adkins DL, Boychuk J, Remple MS, Kleim JA (2006) Motor training induces experience-specific patterns of plasticity across motor cortex and spinal cord. J Appl Physiol (1985) 101:1776-1782.
Burda JE, Sofroniew MV (2014) Reactive gliosis and the multicellular response to CNS damage and disease. Neuron 81:229-248.
Carmichael ST, Chesselet MF (2002) Synchronous neuronal activity is a signal for axonal sprouting after cortical lesions in the adult. J Neurosci 22:6062-6070.
Hamzei F, Glauche V, Schwarzwald R, May A (2012) Dynamic gray matter changes within cortex and striatum after short motor skill training are associated with their increased functional interaction. Neuroimage 59:3364-3372.
Hayakawa K, Nakano T, Irie K, Higuchi S, Fujioka M, Orito K, Iwasaki K,Jin G, Lo EH, Mishima K, Fujiwara M (2010) Inhibition of reactive astrocytes with fluorocitrate retards neurovascular remodeling and recovery after focal cerebral ischemia in mice. J Cereb Blood Flow Metab 30:871-882.
Hirase H, Iwai Y, Takata N, Shinohara Y, Mishima T (2014) Volume transmission signalling via astrocytes. Philos Trans R Soc Lond B Biol Sci 369:20130604.
Kelly PJ, Furie KL, Shafqat S, Rallis N, Chang Y, Stein J (2003) Functional recovery following rehabilitation after hemorrhagic and ischemic stroke.Arch Phys Med Rehabil 84:968-972.
Liu Z, Li Y, Cui Y, Roberts C, Lu M, Wilhelmsson U, Pekny M, Chopp M(2014) Beneficial effects of gfap/vimentin reactive astrocytes for axonal remodeling and motor behavioral recovery in mice after stroke. Glia 62:2022-2033.
Mestriner RG, Saur L, Bagatini PB, Baptista PP, Vaz SP, Ferreira K, Machado SA, Xavier LL, Netto CA (2015) Astrocyte morphology after ischemic and hemorrhagic experimental stroke has no influence on the different recovery patterns. Behav Brain Res 278:257-261.
Napieralski JA, Butler AK, Chesselet MF (1996) Anatomical and functional evidence for lesion-specific sprouting of corticostriatal input in the adult rat. J Comp Neurol 373:484-497.
Neves JD, Aristimunha D, Vizuete AF, Nicola F, Vanzella C, Petenuzzo L,Mestriner RG, Sanches EF, Gon?alves CA, Netto CA (2017) Glial-associated changes in the cerebral cortex after collagenase-induced intracerebral hemorrhage in the rat striatum. Brain Res Bull 134:55-62.
Qureshi AI, Mendelow AD, Hanley DF (2009) Intracerebral haemorrhage.Lancet 373:1632-1644.
 中國(guó)神經(jīng)再生研究(英文版)2018年1期
中國(guó)神經(jīng)再生研究(英文版)2018年1期
- 中國(guó)神經(jīng)再生研究(英文版)的其它文章
- Neural Regeneration Research: Information for Authors
- Injury of the Papez circuit in a patient with traumatic spinal cord injury and concomitant mild traumatic brain injury
- Critical role of SDF-1/CXCR4 signaling pathway in stem cell homing in the deafened rat cochlea after acoustic trauma
- Low-frequency pulsed electromagneticfield pretreated bone marrow-derived mesenchymal stem cells promote the regeneration of crush-injured rat mental nerve
- PTEN knockdown with the Y444F mutant AAV2 vector promotes axonal regeneration in the adult optic nerve
- Neuroprotective mechanisms of rutin for spinal cord injury through anti-oxidation and anti-inflammation and inhibition of p38 mitogen activated protein kinase pathway
