Prognostic significance of lymphovascular infiltration in overall survival of gastric cancer patients after surgery with curative intent
Liangliang Wu ,Yuexiang Liang ,Chen Zhang,Xiaona Wang,Xuewei Ding,Chongbiao Huang,Han Liang
1Department of Gastric Cancer,Tianjin Medical University Cancer Institute and Hospital,National Clinical Research Center of Cancer,Key Laboratory of Cancer Prevention and Therapy,Tianjin 300060,China;2Department of Gastrointestinal Oncology,the First Affiliated Hospital of Hainan Medical University,Haikou 570102,China;3Nutritional Department,Tianjin Beichen Hospital,Tianjin 300000,China;4Senior Ward,Tianjin Medical University Cancer Institute and Hospital,National Clinical Research Center of Cancer,Key Laboratory of Cancer Prevention and Therapy,Tianjin 300060,China
Abstract Objective:Lymphovascular infiltration(LVI)is frequently detected in gastric cancer(GC)specimens.Studies have revealed that GC patients with LVI have a poorer prognosis than those without LVI.Methods:In total,1,007 patients with curatively resected GC at Department of Gastric Cancer,Tianjin Medical University Cancer Institute and Hospital were retrospectively enrolled.The patients were categorized into two groups based on the LVI status:a positive group(PG;presence of LVI)and a negative group(NG;absence of LVI).The clinicopathological factors corrected with LVI and prognostic variables were analyzed.Additionally,a pathological lymphovascular-node(lvN)classification system was proposed to evaluate the superiority of its prognostic prediction of GC patients compared with that of the eighth edition of the N staging system.Results:Two hundred twenty-four patients(22.2%)had LVI.The depth of invasion and lymph node metastasis were independently associated with the presence of LVI.GC patients with LVI demonstrated a significantly lower overall survival(OS)rate than those without LVI(42.8% vs.68.9%,respectively;P<0.001).In multivariate analysis,LVI was identified as an independent prognostic factor for GC patients(hazard ratio:1.370;95% confidence interval:1.094-1.717;P=0.006).Using strata analysis,significant prognostic differences between the groups were only observed in patients at stage I-IIIa or N0-2.The lvN classification was found to be more appropriate to predict the OS of GC patients after curative surgery than the pN staging system.The-2 log-likelihood of lvN classification(4,746.922)was smaller than the value of pN(4,765.196),and the difference was statistically significant(χ2=18.434,P<0.001).Conclusions:The presence of LVI influences the OS of GC patients at stage I-IIIa or N0-2.LVI should be incorporated into the pN staging system to enhance the accuracy of the prognostic prediction of GC patients.
Keywords:Gastric carcinoma;lymphovascular infiltration;LVI;prognosis;risk factors
Introduction
A standard therapeutic strategy for gastric cancer(GC)by stage has been established in Japanese GC treatment guidelines.Radical gastrectomy with D2 lymph node dissection has become increasingly regarded as the standard surgical procedure for potentially curable T2-T4 tumors and cT1N+tumors(1).Endoscopic submucosal dissection(ESD)is also indicated as a standard treatment for differentiated adenocarcinoma without ulcerative findings,in which the depth of invasion is clinically diagnosed as T1a and the diameter is≤2 cm(1).Perioperative chemotherapy and chemoradiotherapy have been affirmed to further improve overall survival(OS)of advanced GC patients(2-4).However,even after curative surgery plus adjuvant therapy,the long-term outcome of GC remains poor.The main reason is that most patients have lymph node metastasis or micrometastasis at diagnosis.Lymphovascular infiltration(LVI),which is also referred to as blood vessel and lymphatic invasion,was reported to be a useful indicator of lymph node metastasis or distant metastasis(5,6).In Japanese GC treatment guidelines,the presence of LVI in endoscopically resected specimens is regarded as non-curative resection because of high incidence of lymph node metastasis,and gastrectomy with lymph node dissection should be performed subsequently as a remedy(1).The presence of LVI has been shown to be associated with a higher recurrence rate and poorer prognosis in several malignancies,including colorectal cancer,breast cancer,and non-small cell lung cancer(7-11).In hepatocellular carcinoma,LVI is included in the Barcelona Clinic Liver Cancer(BCLC)staging system,and the presence of LVI in the portal vein is classified as stage C(12).Regarding GC,LVI was frequently detected in the resected specimens,especially in advanced disease.However,its clinical significance has been rarely evaluated.In this study,we retrospectively analyzed the outcomes of 1,007 GC patients who underwent surgery with curative intent.We aimed to evaluate the potential impact of LVI on long-term outcomes of GC patients after curative surgery and test the superiority of lvN classification for prognostic prediction in GC compared with N stage in the eighth edition of TNM staging system for GC.
Materials and methods
Patients
The Ethics Committee of Tianjin Medical University Cancer Institute and Hospital has reviewed and approved this study.A total of 1,508 patients with GC who underwent surgical resection at Tianjin Medical University Cancer Institute and Hospital between July 2011 and June 2013 were eligible for this study.The eligibility criteria for this study included the following:1)patients with adenocarcinoma of the stomach;2)patients who underwent gastrectomy with curative intent;3)patients with stage I-IIIc disease;4)patients with no history of gastrectomy or other malignancies;5)patients with no history of neoadjuvant chemotherapy;6)patients who received at least D1+lymph node dissection;7)patients with a total number of dissected lymph nodes greater than 16;8)patients who were completely followed up;and 9)patients who did not die during the initial hospital stay or for 1 month after surgery.After excluding 4 patients with gastric neuroendocrine carcinoma,1 patient with gastric squamous cell carcinoma,20 patients with remnant GC,14 patients with other malignant tumors,38 patients who accepted neoadjuvant chemotherapy,72 patients who received less than D1 lymph node dissection,265 patients with lymph node retrieval less than 16,7 patients who died within 1 month after surgery,53 patients who were lost,and 27 patients with distant metastasis,ultimately,1,007 patients were enrolled in this study.
Evaluation of clinicopathological variables and survival
Clinicopathological variables studied included 12 factors:sex,age at surgery,tumor location,Borrmann type,tumor size,histology,depth of invasion,lymph node metastasis,extranodal tumor deposits,LVI,preoperative carbohydrate antigen(CA)19-9 levels,and carcinoembryonic antigen(CEA)levels.Tumors were staged according to the 8th edition of the Union for International Cancer Control(UICC)TNM classification system,whereas lymphadenectomy and lymph node stations were defined according to the 3rd English edition of the Japanese Classification of Gastric Carcinoma and the 4th English edition of the Japanese Gastric Cancer Treatment Guidelines(13).The tumors were classified into two groups based on histology:differentiated type,including papillary,well or moderately differentiated adenocarcinoma;and undifferentiated type,including poorly differentiated or undifferentiated adenocarcinoma,signet ring cell carcinoma and mucinous carcinoma.
Incorporation of LVI into the eighth edition of UICC pN stage system
According to the prognostic impact of LVI on GC patients with different pN stages,we established a new lymphovascular-node(lvN)classification by incorporating LVI into the eighth edition of the UICC pN staging system.The lvN classification was defined as follows:lvN0,N0 stage without LVI;lvN1,N1 stage without LVI and N0 stage with LVI;lvN2,N2 stage without LVI;lvN3a,N3a stage regardless of LVI and N1-2 stages with LVI;lvN3b,N3b stage regardless of LVI.The differences in prognostic prediction between the eighth edition of the pN staging system and lvN classification system were directly compared.
Follow-up
The patients were followed up by an attending physician and research nurse at Department of Gastric Cancer,Tianjin Medical University Cancer Institute and Hospital.To increase the follow-up rate,methods such as telephone,message,correspondence and outpatient department visits were used together.The patients were followed up with every 3 months for up to 2 years after surgery,then every 6 months for up to 5 more years,and then once every year or until death.A physical examination,laboratory tests(including assessing CEA and CA19-9),and an abdominal ultrasound(US)were performed at each visit,while chest and abdominal computed tomography(CT)and endoscopy were obtained every 6 months or each year.The OS rate was calculated from the day of surgery until the time of death or final follow-up.The median follow-up was 53(range:2-72)months.The date of the final follow-up was July 30,2018.
Statistical analysis
The categorical variables were analyzed using Chi-squared or Fisher’s exact test.Logistic regression analysis was used to identify the independent risk factors for the presence of LVI.The OS curves were calculated using the Kaplan-Meier method based on the length of time between the primary surgical treatment and final follow up or death.The log-rank test was used to assess significant differences between curves.Independent prognostic factors were identified by the Cox proportional hazards regression model.To compare the redefinition of the lvN classification with the eighth edition of the N staging system,the-2 log-likelihood,hazard ratio(HR)value,and 95% confidence interval(95% CI)related to the Cox regression model were used to measure homogeneity and discriminatory ability.The difference in the-2 loglikelihood between lvN classification and the N staging system was compared using analysis of variance,which was accomplished using R software(Version 3.4.3;R Foundation for Statistical Computing,Vienna,Austria).P<0.05(bilateral)was considered statistically significant.Statistical analysis was performed using SPSS 18.0(SPSS Inc.,Chicago,IL,USA).
Results
Clinicopathological features and potential risk factors for presence of LVI
The 1,007 patients included 705 males(70.0%)and 302 females(30.0%).The age ranged from 19 to 86 years old,and the median age was 56 years old.Of the 1,007 GC patients,383 underwent total gastrectomy,and 624 patients received subtotal gastrectomy.Regarding the extent of lymphadenectomy,D1+lymphadenectomy was indicated for cT1N0 tumors and D2 lymphadenectomy for cN+or cT2-T4 tumors.More extended lymphadenectomy than D2 was performed in patients with suspicious metastasis to No.14v or No.13 lymph node station.Thus,176 patients underwent D2+lymph node dissection,764 patients had D2 dissection,and 67 patients had D1+dissection.Seven hundred ninety-two patients received postoperative adjuvant chemotherapy with capecitabine,S-1,or 5-fluorouracil,leucovorin and oxaliplatin(FOLFOX6),or capecitabine and oxaliplatin(XELOX)regimen.
Of the 1,007 GC patients who underwent gastrectomy,224(22.2%)patients had LVI.All the patients were categorized into 2 groups based on the LVI status:positive group(PG)and negative group(NG).Thus,224 patients were assigned to PG,and 783 patients to NG.The clinicopathological factors were compared inTable 1.No significant differences were found in sex,age at surgery,and preoperative CA19-9 levels between the groups,while factors such as tumor location,Borrmann type,tumor size,histology,depth of invasion,lymph node metastasis,TNM stage,extranodal tumor deposits and preoperative CEA levels were correlated with the presence of LVI.In multivariate analysis,only depth of invasion[hazard ratio(HR):1.270;95% CI:1.009-1.597;P=0.041]and lymph node metastasis(HR:1.476;95% CI:1.286-1.694;P<0.001)were independently associated with the presence of LVI(Table 2).
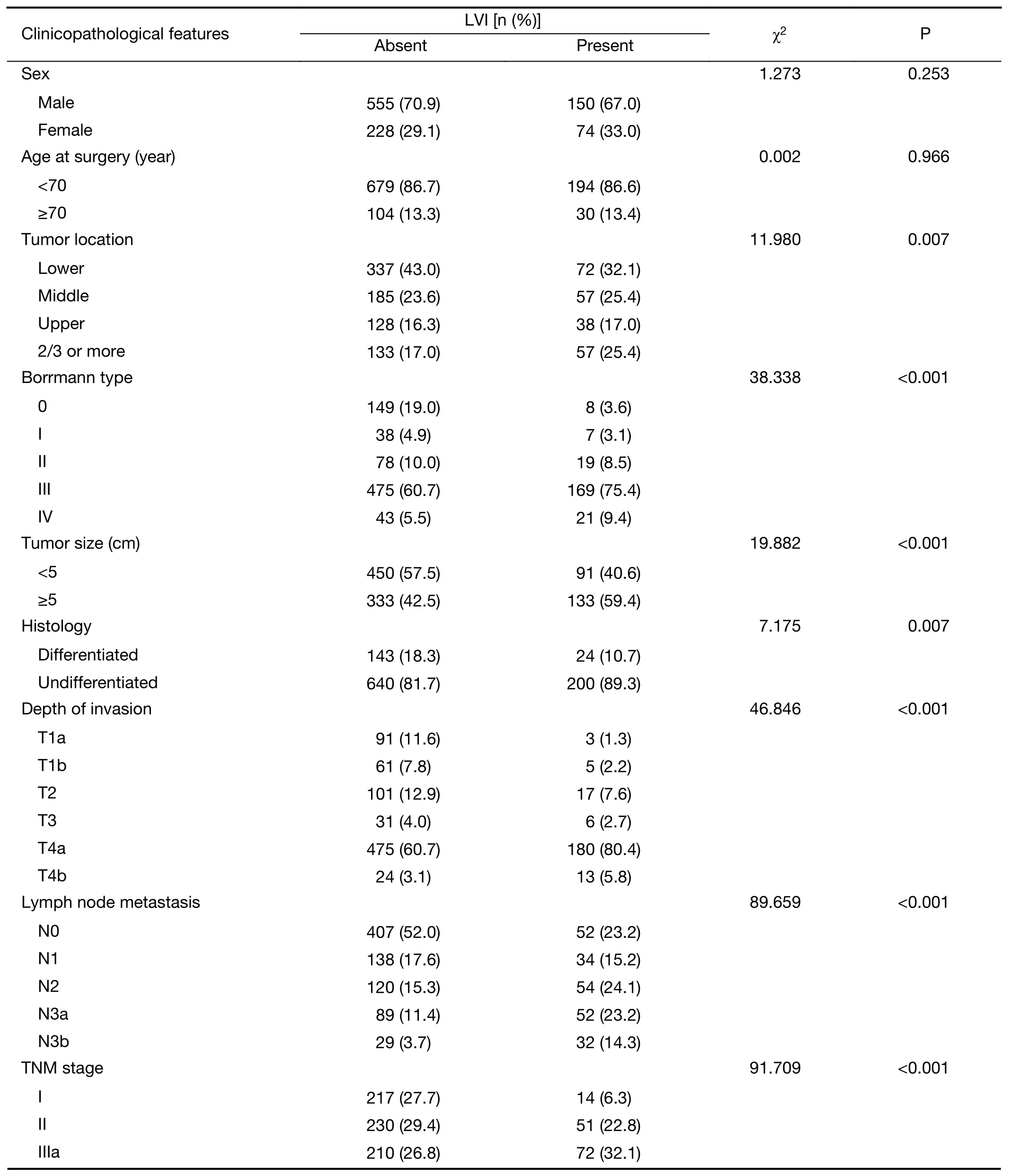
Table 1 Case characteristics
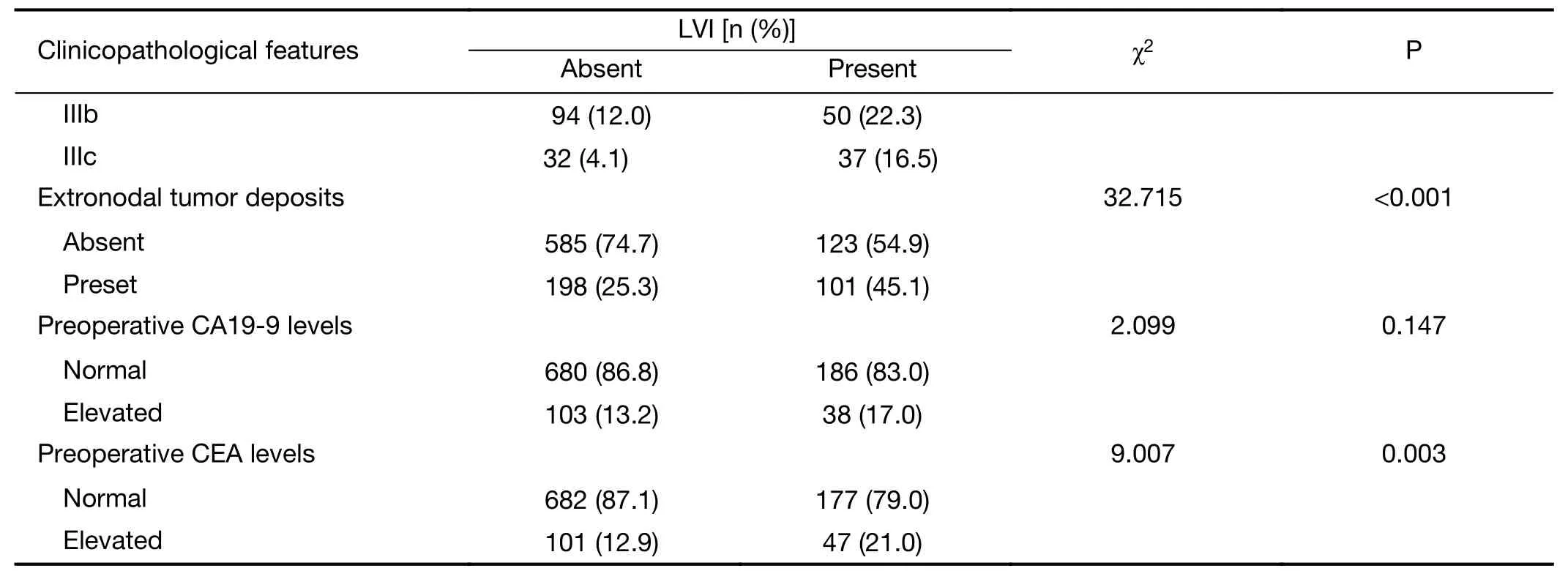
Table 1 (continued)
Survival analysis of all GC patients
Ten factors evaluated in univariate analysis had a significant effect on survival:age at surgery,tumor location,Borrmann type,tumor size,TNM stage,type of gastrectomy,extranodal tumor deposits,preoperative CA19-9 levels,CEA levels,and LVI status.GC patients with LVI had a significantly lower 5-year OS rate than those without LVI(5-year OS:42.8%vs.68.9%,respectively;P<0.001)(Figure 1A).In multivariate analysis,LVI(HR:1.370 for PG;95% CI:1.094-1.717;P=0.006)was found to be an independent prognostic factor for OS,as well as the following:age at surgery,Borrmann type IV,TNM stage and extranodal tumor deposits(Table 3).
Using strata analysis,the significant prognostic differences between the groups were only observed in GC patients at stage I-IIIa or N0-2(Table 4).For patients at N0-2 stage(or with 0-6 lymph nodes metastasis),LVI had a significantly negative impact on OS,and the 5-year OS rates were 73.7% for those without LVI and 48.8% for those with LVI(P<0.001)(Figure 1B).
Incorporation of LVI status into the eighth edition of UICC pN staging system
The OS of N0-stage patients with LVI was similar to that of N1-stage patients without LVI.The OS of N1-or N2-stage patients with LVI was equal to that of N3a-stage patients without LVI.In the N3a and N3b stages,no significant survival differences were found between patients with and without LVI(Figure 2).Based on these results,we incorporated LVI into the eighth edition of the UICC pN stage system and introduced the new pathological lvN stages(Table 5).Multivariate analysis was used to evaluate the value of pN stage(model 1)and lvN classification(model 2)to assess the prognosis of GC.Factors including age at surgery,depth of invasion,Borrmann type and tumor deposits were adjusted in multivariate analysis.The 5-year OS rates were 82.5%,65.2%,51.5%,42.9%,and 26.2% in the lvN0,lvN1,lvN2,lvN3a and lvN3b stages,respectively(χ2=196.855,P<0.001).The 5-year OS rates were 80.1%,61.1%,49.9%,43.3% and 26.2% in the pN0,pN1,pN2,pN3a and pN3b stages,respectively(χ2=181.400,P<0.001)(Table 6,Figure 3).The differences in the prognostic prediction between the eighth edition of the pN staging system and lvN classification system were directly compared(Table 6).The lvN classification(HR=1.642,95% CI:1.522-1.771,P<0.001)system was confirmed to be a more appropriate prognostic classification to predict the OS of GC patients after curative resection rather than the eighth edition of the pN classification(HR=1.605,95% CI:1.491-1.729;P<0.001).The-2 log-likelihood of the lvN stage was 4,746.922,which is smaller than the value of pN(4,765.196),and the difference was statistically significant(χ2=18.434;P<0.001).
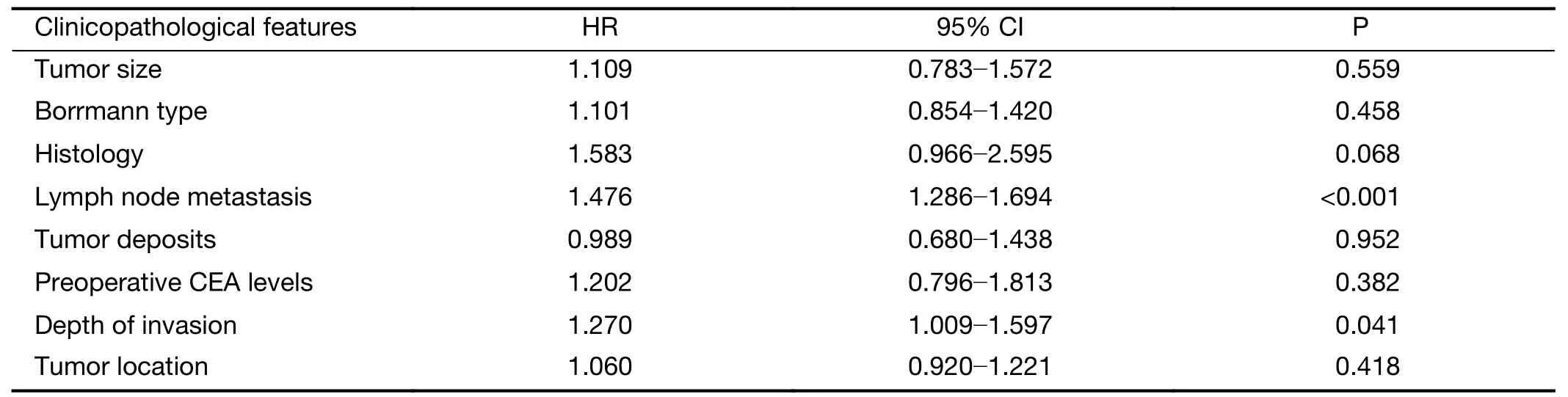
Table 2 Multivariate analysis of risk factors for presence of LVI
Figure 1 Survival curves according to status of lymphovascular infiltration.(A)All patients(P<0.001);(B)Patients with 0-6 lymph node metastases(P<0.001).
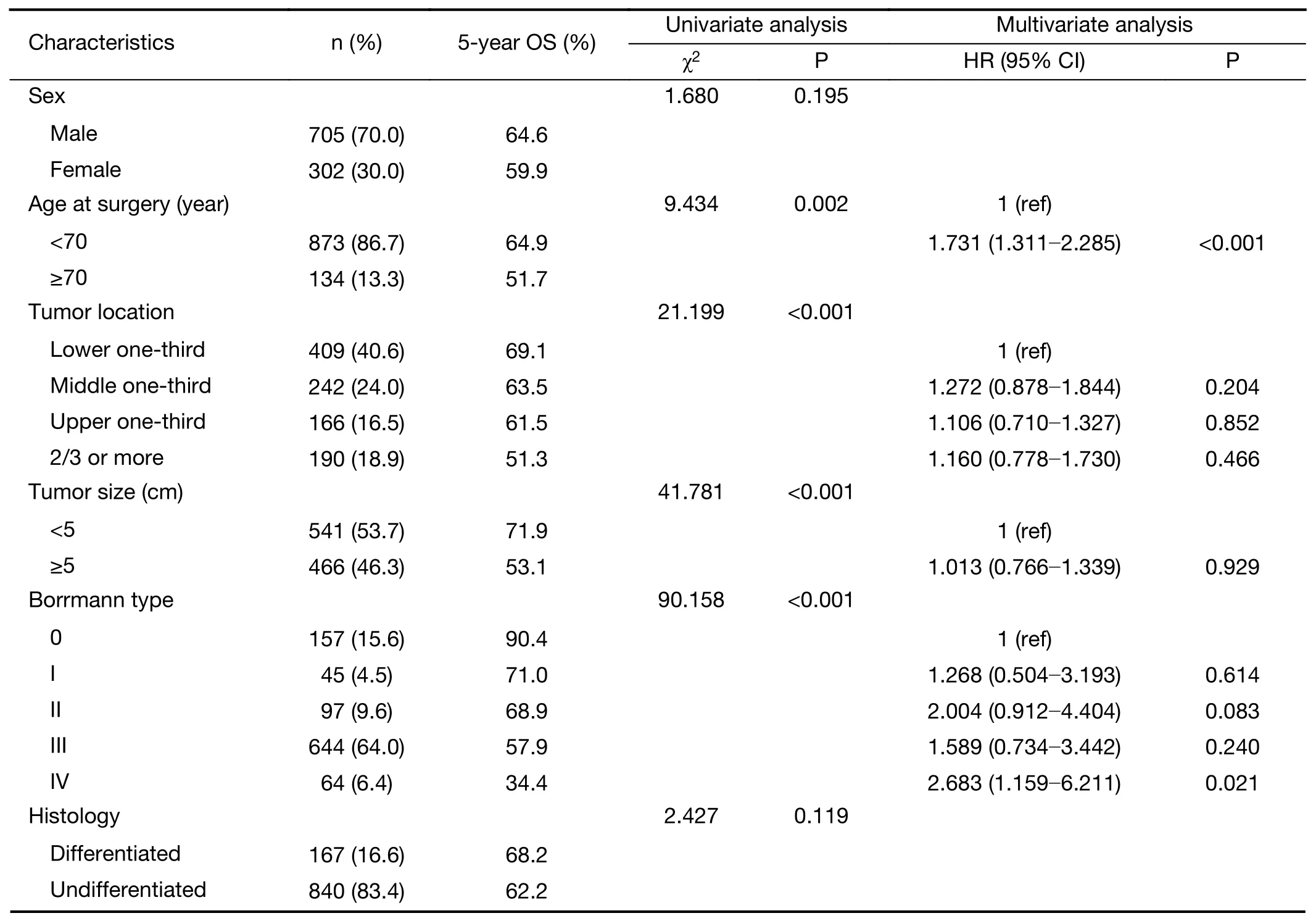
Table 3 Univariate and multivariate survival analysis of GC patients in the whole study series
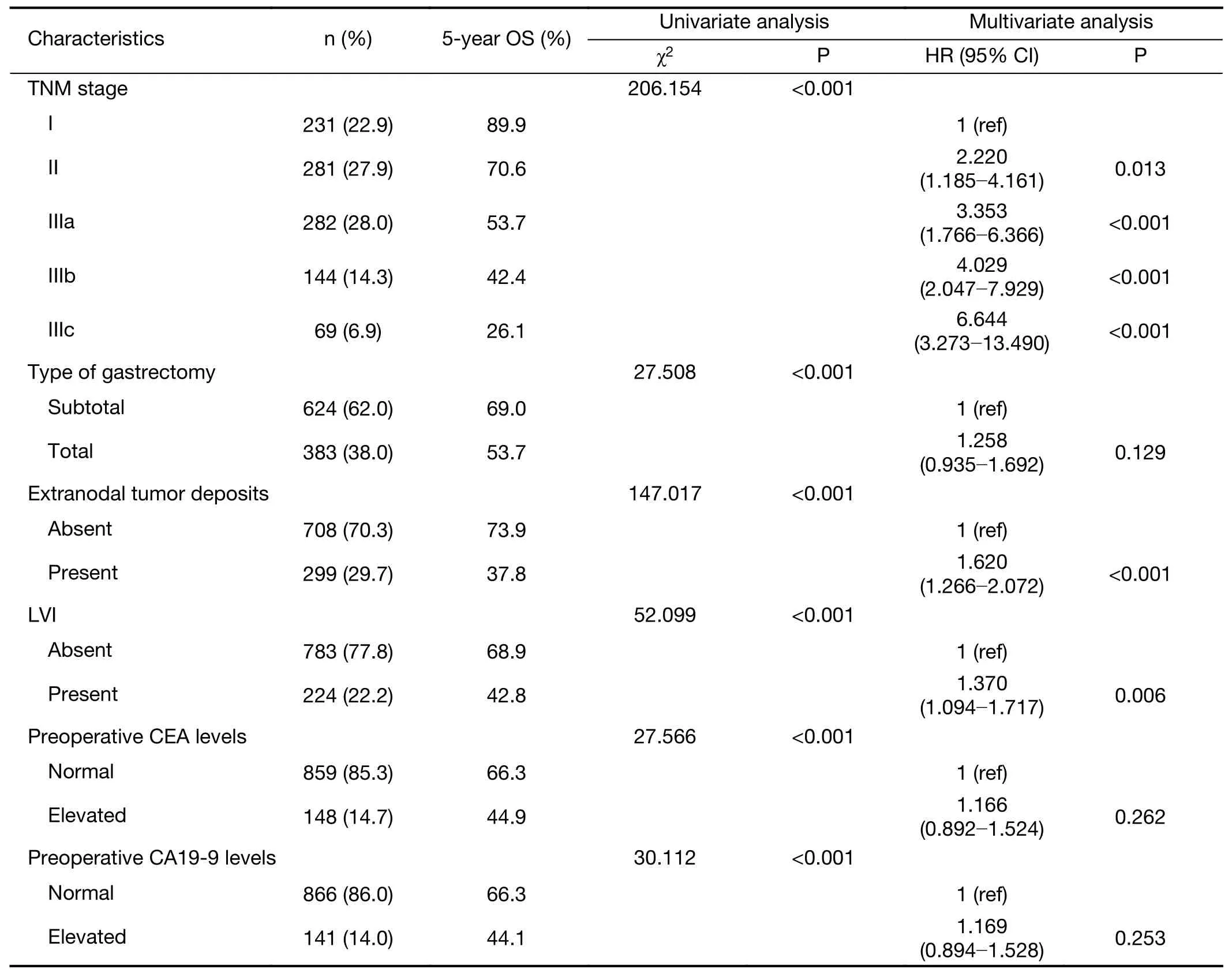
Table 3 (continued)
Discussion
LVI is the presence of tumor cells within the blood or lymphatic vessels.LVI is a common pathological finding in cancer specimens and is regarded as an indicator of a poor prognosis for many types of cancer(7-11).Additionally,LVI is incorporated into the staging system of hepatocellular carcinoma because of its ability to predict the prognosis and recurrence(12,14).Regarding GC,the presence of LVI in endoscopically resected specimens is considered as a high-risk factor for lymph node metastasis according to the Japanese GC Treatment Guidelines(1).However,the value of LVI in specimens of gastrectomy has not been widely realized and no consensus has been reached.Although several studies have affirmed that LVI is independently associated with a poor survival of GC patients after surgery(15-21),the significance of LVI in GC remains uncertain,and its staging value is rarely assessed presently.In the present study,we found that the depth of invasion and lymph node metastasis were independently correlated with the presence of LVI.LVI was identified as an independent prognostic factor for the whole study series.However,LVI did not affect the OS of GC patients at the pN3a and pN3b stages.After the incorporation of LVI into the pN stage,the new lvN classification can better predict the prognosis for GC patients after curative surgery than the eighth edition of the pN staging system.
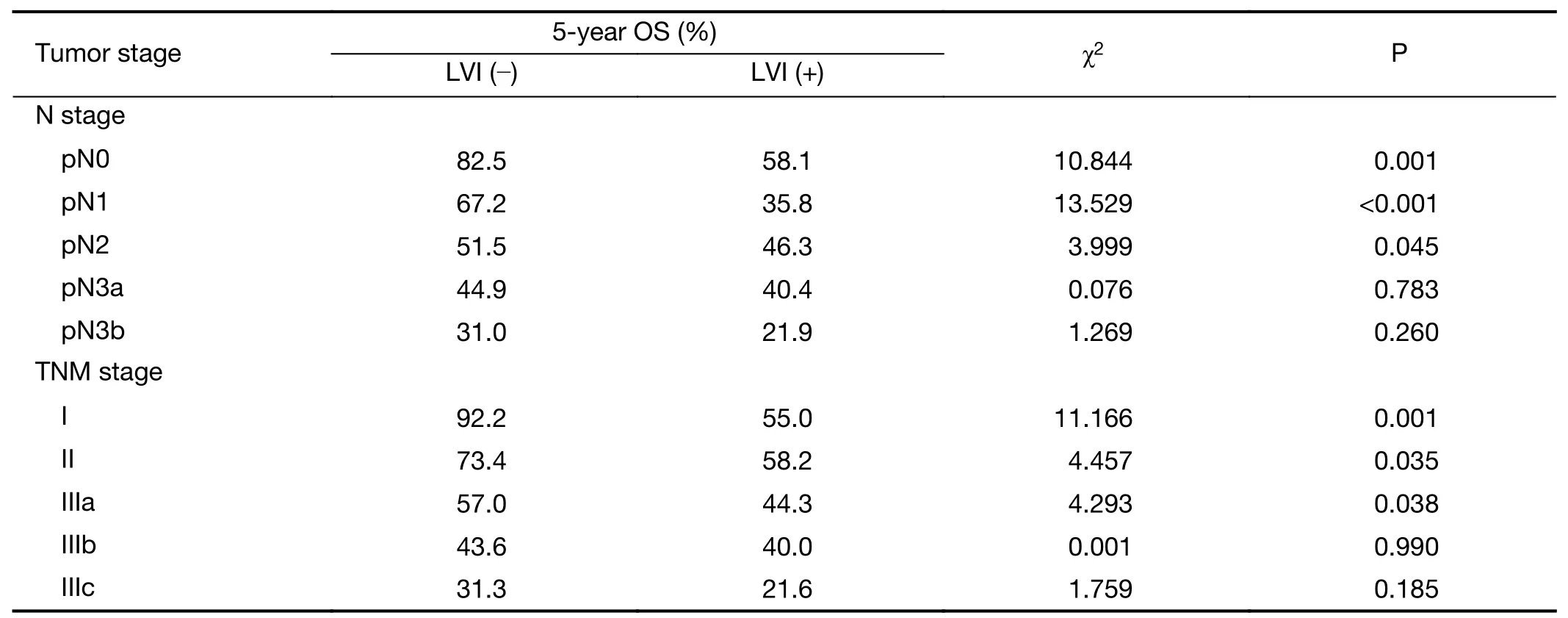
Table 4 Strata survival analysis of GC patients according to tumor stage
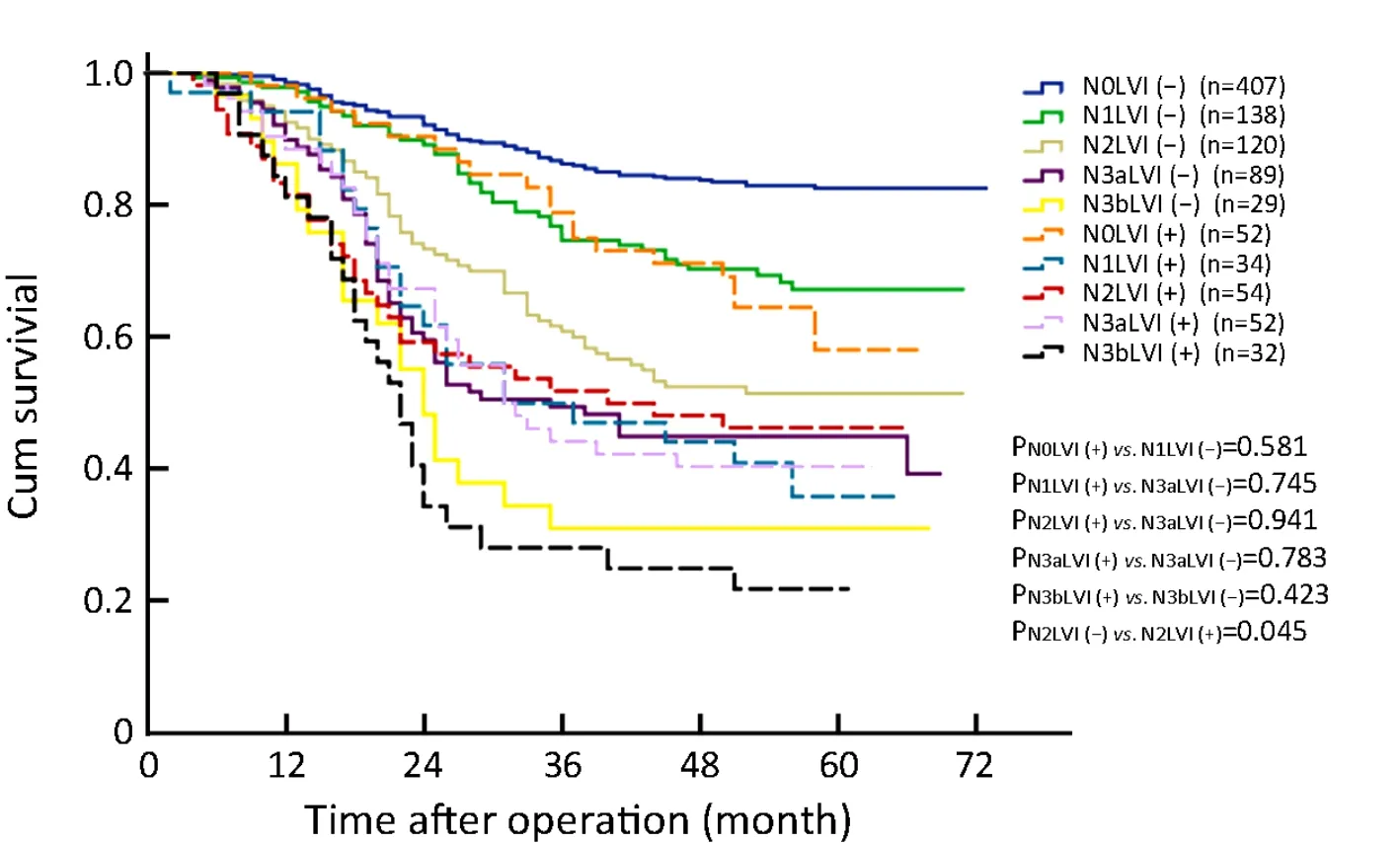
Figure 2 Comparison of survival curves of patients with different N stages and lymphovascular infiltration(LVI)status.Overall survival(OS)of N0-stage patients with LVI was similar to that of N1-stage patients without LVI(P=0.581).OS of N1-or N2-stage patients with LVI was equal to that of N3a-stage patients without LVI(P values were 0.745 and 0.941,respectively).
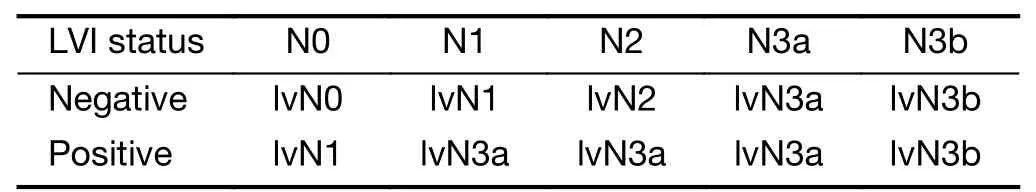
Table 5 LVI status of GC was incorporated into pN stage and composed the new lvN stage
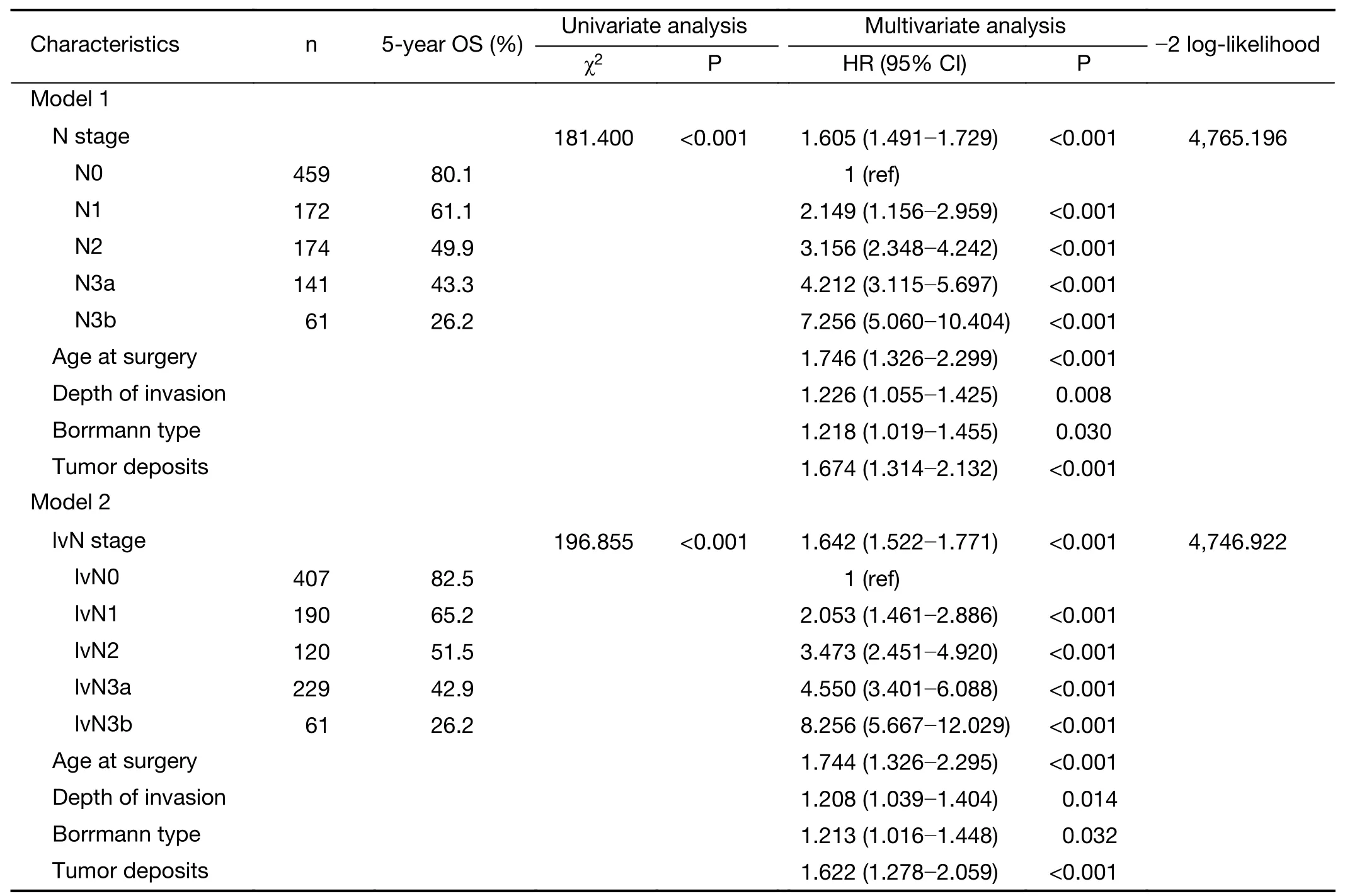
Table 6 Definitions of N categories and their impact on prognostic value of staging
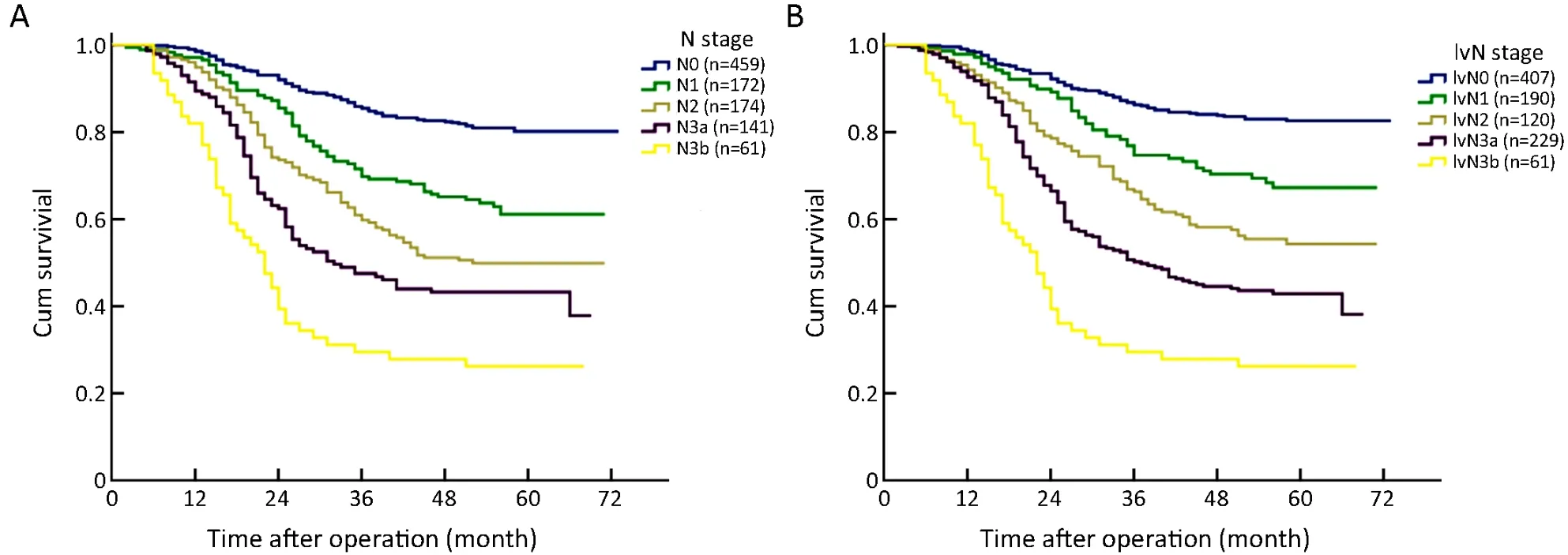
Figure 3 Survival curve of patients according to subgroups of pN stage(P<0.001)(A)and lymphovascular-node(lvN)classification(P<0.001)(B).
Presently,the major detection methods of LVI include haematoxylin-eosin(H&E)staining and immunohistochemistry(IHC).In this retrospective study,the presence of LVI was detected in 22.2% of GC patients by H&E staining complemented by IHC with CD34.Liet al.reported that 35.2% of GC patients had presented with LVI as detected by H&E staining(18).However,a study by Dickenet al.indicated that LVI was detected in 59.6%of GC patients by IHC staining(19).According to previous studies,the positive rate of LVI in GC patients ranged from 10% to 60%(15-21).The different incidence rates of LVI may be due to different staining methods,number of examined samples,different criteria of LVI and different stages of the included patients.It was also reported that the accuracy of LVI diagnosis could be increased by using IHC with CD34(a pan-endothelial marker)and D2-40(a lymphatic endothelial)(22).Despite differences in the incidence of detection between the two methods,studies have confirmed that the presence of LVI,as detected by both H&E and IHC staining,is significantly correlated with the depth of invasion,lymph node metastasis and degree of malignancy(22-23).Our results were consistent with these findings,and multivariate logistic regression analysis identified that the depth of invasion and lymph node metastasis were independent risk factors correlated with the presence of LVI.Although the incidence of LVI is lower in early GC,the status of LVI determines the therapeutic strategy(24-28).ESD has been regarded as a standard curative therapy for selected T1a GC in the Japanese GC Treatment Guidelines(1).However,if LVI is presented in the specimen,additional gastrectomy plus lymph node dissection is needed to be performed(26,28)because the presence of LVI indicates a high incidence of lymph node metastasis.Actually,our data also supported this view.In the T1a stage GC patients,among the 3 patients with LVI,2 also had lymph node metastasis;among the 91 patients without LVI,86 were also absent of positive lymph nodes.The accuracy of the prediction of lymph node status by LVI was 93.6%[(86+2)/94×100%].In our opinion,LVI is a reliable indicator of lymph node status in T1a GC,and patients with LVI are at a high risk of lymph node metastasis.More aggressive treatment,such as gastrectomy or postoperative chemotherapy,should be considered.
Regarding the prognostic value of LVI,previous studies had affirmed the positive influence of LVI on OS for various types of malignancies,including GC(7-12,15-21).Dickenet al.found that LVI is an independent predictor of survival in GC(19).Liet al.affirmed that the presence of vascular invasion is a risk factor for recurrence and is independently associated with the poor survival of nonmetastatic GC(18).In the present study,GC patients with LVI demonstrated a significantly worse survival than those without LVI,and LVI was found to be an independent prognostic factor in multivariate analysis(HR:1.370;95%CI:1.094-1.717;P=0.006).These results were consistent with previous studies and might indicate that LVI is a nonnegligible factor for predicting the prognosis and determining the treatment strategies after surgery.The TNM classification of GC is the most important prognostic indicator and is considered a key clue for treatment.Nonetheless,it remains unclear whether LVI should be incorporated into the TNM staging system for GC.We found that the OS of N0-stage patients with LVI was similar to that of N1-stage patients without LVI.Additionally,no survival differences were observed among patients with LVI at N1,N2 and N3a disease,and the survival of N1-3a-stage patients with LVI was equal to that of N3a-stage patients without LVI.Based on these results,we incorporated the LVI status into the eighth edition of the UICC pN staging system,and then we proposed the new lvN classification system to evaluate the prognostic value of the pN stage and lvN classification in GC.We found that the lvN classification was a more appropriate prognostic classification to predict the OS of GC patients after curative resection than the eighth edition of the pN staging system.In our opinion,LVI contains some unique prognostic information that is not included in the TNM staging system and incorporating LVI into the new revision of the lvN classification for GC can better predict the prognosis and then determine treatment.
Conclusions
The presence of LVI indicates the aggressive characteristics of GC,such as deeper depth of invasion and more lymph nodes metastases.GC patients with LVI usually have a poorer prognosis,and survival of these patients at stage N0-2 is significantly worsened by LVI.Pathologists should be aware of this clinically important feature and carefully examine specimens from GC patients to determine the presence of LVI upon histological examination,and the LVI status should be recorded in the pathology report.Meanwhile,LVI should be considered in GC staging.GC patients with LVI should be closely followed up and more seriously treated with gastrectomy or adjuvant chemotherapy.
Acknowledgements
This study was supported in part by grants from the Program of National Natural Science Foundation of China(No.81572372);National Key Research and Development Program of Major Chronic Non-infectious Disease Prevention and Control Research(No.2016YFC1303202);National Key Research and Development Program“Precision Medicine Research”Program(No.2017 YFC0908300);Application Foundation and Advanced Technology Program of Tianjin Municipal Science and Technology Commission(No.15JCYBJC24800);and Scientific Research Project of Tianjin Municipal Education Commission(No.2018KJ015).
Footnote
Conflicts of Interest:The authors have no conflicts of interest to declare.
 Chinese Journal of Cancer Research2019年5期
Chinese Journal of Cancer Research2019年5期
- Chinese Journal of Cancer Research的其它文章
- A study on service capacity of primary medical and health institutions for cervical cancer screening in urban and rural areas in China
- Medical expenditures for colorectal cancer diagnosis and treatment:A 10-year high-level-hospital-based multicenter retrospective survey in China,2002-2011
- Surgical outcomes of hand-assisted laparoscopic liver resection vs.open liver resection:A retrospective propensity scorematched cohort study
- Texture analysis on gadoxetic acid enhanced-MRI for predicting Ki-67 status in hepatocellular carcinoma:A prospective study
- Machine-learning-assisted prediction of surgical outcomes in patients undergoing gastrectomy
- Phosphoglucose isomerase gene expression as a prognostic biomarker of gastric cancer
