Surgical outcomes of hand-assisted laparoscopic liver resection vs.open liver resection:A retrospective propensity scorematched cohort study
Shengtao Lin,Fan Wu,Liming Wang,Yunhe Liu,Yiling Zheng,Tana Siqin,Weiqi Rong,Jianxiong Wu
Department of Hepatobiliary Surgery,National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital,Chinese Academy of Medical Sciences and Peking Union Medical College,Beijing 100021,China
Abstract Objective:Hand-assisted laparoscopic liver resection has the advantages of open and laparoscopic surgeries.There is still lack of comparison of surgical outcomes between hand-assistied laparoscopic liver resection(HALLR)and open liver resection(OLR).This study compared the surgical outcomes of the two approaches between wellmatched patient cohorts.Methods:Patients who received liver resection during January 2014 and October 2017 in Cancer Hospital,Chinese Academy of Medical Sciences and Peking Union Medical College were included in this retrospective study.Propensity score matching(PSM)was performed to reduce selection bias between the two groups.Operation and short-term surgical outcomes were compared between the well matched groups.Results:During this period,232 patients with a median age of 55.1 years old received OLR,while 49 patients with a median age of 54.7 years old received HALLR.Compared with HALLR group,OLR group has a higher proportion in male patients(190/232,81.9% vs.34/49,69.4%,P=0.048)and lower albumin(43.2±4.5 vs.44.8±3.7,P=0.020).After PSM,49 patients from each group were included in the following analysis.Two groups were well balanced in their baseline characteristics,liver functions,preoperative treatments,abdominal surgery history,and surgical difficulty.None perioperative mortality was observed in both groups.Operation time and postoperative complications were similar in two groups(P=0.935,P=0.056).The HALLR group showed less bleeding amount(177.8±217.1 mL vs.283.1±225.0 mL,P=0.003)and shorter postoperative stay period(6.9±2.2 d vs.9.0±3.5 d,P=0.001).Conclusions:We demonstrated that hand-assisted laparoscopic surgery is feasible and safe for liver resection,including some difficult cases.HALLR can provide better bleeding control and faster recovery after surgery.
Keywords:Surgical outcomes;hand-assisted laparoscopic surgery;liver resection
Introduction
Surgeons constantly pursue minimally invasive and safe surgical approaches.With improved knowledge of liver anatomy,better understanding of the underlying liver disease and improvements in surgical techniques,laparoscopic surgery is now a widely preferred alternative to open liver resection(OLR)(1).Laparoscopic liver resection(LLR)can be performed in three ways:pure LLR,hand-assisted LLR(HALLR),and hybrid-LLR.In HALLR,the assisting hand of the surgeon that is placed in the cavity through the abdominal wall helps in dissection,exposure,palpation,and bleeding control(2).In other words,HALLR has the advantages of pure laparoscopic and open surgeries(3,4).
Several studies have introduced the procedures and applications of hand-assisted approaches in colorectal cancer,liver metastasis,and primary liver cancer(4-7).Hand-assisted laparoscopic surgery(HALS)has also been applied in liver transplantation(8)in combination with short upper midline laparotomy.Hepatic parenchymal transection using radiofrequency device was also feasible in HALS(9).In addition,it is recommended that hand assistance can be applied for the purpose of bleeding control or for completing a difficult surgery in pure-LLR(1).However,hand-assisted liver surgery constituted only 7% of all laparoscopic liver surgeries according to a survey conducted by a Japanese scholar(10).Whether HALS is safe and feasible in liver resection remained to be elucidated.Moreover,although HALS has been used for peripheral and small lesions,there were limited studies reporting HALS in difficult cases(11).There is still lack of high-level evidence comparing the outcomes of liver resection between open and hand-assisted approaches.More studies are needed in the future.
However,it is difficult to conduct randomized control trails comparing different surgical approaches in clinical practice.Propensity score matching(PSM)is a statistical matching method that can reduce selection bias induced by the differences in the baseline characteristics in observational non-randomized study(12-14).In this study,we retrospectively analyzed the surgical outcomes of patients who received different surgical treatment methods.Covariates that can affect the results of group allocation were considered in PSM.Two comparable groups balanced in the baseline characteristics were generated after PSM.In this study,we aimed at comparing the performance of HALLR with that of OLR.
Materials and methods
Study population and study design
This retrospective study has been approved by the Research Ethics Committee of Cancer Hospital,Chinese Academy of Medical Sciences and Peking Union Medical College.The inform consent was exempted in this retrospective study.Patients who received liver resection by a same surgical team at the Cancer Hospital,Chinese Academy of Medical Sciences and Peking Union Medical College in China during January 2014 and October 2017 were retrospectively reviewed in this study.Perioperative evaluation were conducted for all patients,including liver function tests,coagulation function,blood routine test,and radiographic evaluation[including enhanced magnetic resonance imaging(MRI)or enhanced computed tomography(CT)scan].The indications and procedures of liver resection for difficult cases were discussed in weekly multidisciplinary conferences.The exclusion criteria were:multivisceral resection,intraoperative radiotherapy,spontaneous rupture and bleeding of primary liver cancer,or conversion to open surgery.Conversion to open surgery contained several situations:1)Exploratory laparoscopy followed by OLR;2)Laparoscopic liver resection and laparotomy bile jejunum anastomosis/lymph node dissection;and 3)The preoperative evaluation was inaccurate and HALLR approach was not suitable.In addition,left lateral sectionectomy was routinely conducted through pure laparoscopic approach in Cancer Hospital,Chinese Academy of Medical Sciences and Peking Union Medical College,while OLR was routinely conducted for patients with three or more lesions.Therefore,left lateral sectionectomy and surgery for three or more lesions were excluded in the present study.
Surgical procedure
The procedures for OLR have been detailed elsewhere(12,15).Briefly,patients were placed in supine position and anatomical or non-anatomical liver resection was performed on them with a right subcostal or upper midline incision.All lesions were completely removed under hemihepatic vascular occlusion or Pringle maneuver,and no positive margin was noted in the pathology reports.
Several studies have reported the procedures for HALLR(5,16).Briefly,the patients were placed in a modified lithotomy position,and a small subcostal incision(6-8 cm)was made to place the hand-assistant device(17).With the surgeon’s left hand in the abdominal cavity,the tactile sensation was maintained.Palpation was performed,and adequacy surgical margin was obtained in non-anatomical liver resection.The surgeon’s hand also assisted in the exposure and bleeding control,which greatly improved the safety of the operation.Vascular occlusion was conducted using the Pringle maneuver in HALLR.
PSM
PSM was performed by using IBM SPSS Statistics(Version 22.0;IBM Corp.,NewYork,USA).The patients’baseline characteristics[age,gender,BMI(body mass index),ASA(American Society of Anesthesiologists)grade],liver function(total bilirubin,albumin,platelets and prothrombin time),preoperative treatments,abdominal surgery history,and difficulty of liver resection were considered for the generation of propensity scores.Patients in the HALLR group were matched with those in the OLR group,with a 1:1 matching ratio.The nearest neighbor matching without replacement was performed,with the caliper set at 0.02.The difficulty of liver resection was graded according to the difficulty scoring system(10-level index)proposed by Banet al.(18).The difficulty index of liver resection containing two lesions was calculated as follows:(difficulty of major lesion)+1/2×(difficulty of minor lesion).
Clinical outcomes
In this study,we compared the operative outcomes and short-term outcomes between the OLR and HALLR groups.Major vessels and difficulty index were defined according to Banet al.(18).Postoperative complications were graded according to the Clavien-Dindo Ranking System(19).Deaths occurring within 90 d of the surgery were regarded as postoperative mortality.Postoperative liver failure was defined according to the International Study Group of Liver Surgery parameters(20).
Statistical analysis
All continuous data were expressed asand the categorical data were presented with specific numbers and proportions.Studentt-test or Mann-Whitney U test was used for comparing the continuous data between the groups.The χ2test or Fisher’s exact test was applied to analyze the differences in the categorical data.All the statistical analysis were two tailed test and the result was considered to be statistically significant at P<0.05.
Results
During the study period,232 patients in the OLR group and 49 patients in the HALLS group were included for PSM.After matching at 1:1 ratio,49 patients were included for further analysis in each group.
Baseline characteristics
The baseline characteristics of the OLR and the HALLS groups are shown inTable 1.After PSM,the groups were balanced for their preoperative variables,including age;gender;BMI;ASA grade;previous abdominal operation history;previous transarterial chemoembolization;the total levels or counts of bilirubin,albumin,and platelets;prothrombin time(international normalized ratio);and surgical difficulty.
Surgical outcomes
The tumor size,proximity to major vessels,and tumor location were considered as major factors associated with liver surgery difficulty(18).The difficulty index,related factors,and surgical outcomes are summarized inTable 2.There was no difference between the operation time and postoperative mortality between the two groups.Although the postoperative complications in the HALLR group were fewer,they were not significantly different from those in the OLR group(P=0.056).One patient in the HALLR group suffered from acute hepatic failure,but recovered after plasma transfusion,glucocorticoid,and hepatic protection treatments.Abdominal infection occurred in four patients in the OLR group,two of whom received abdominocentesis.One patient received plasma transfusion because of hepatic insufficiency in the OLR group.No postoperative death occurred in both groups.The bleeding amount(177.8±217.1 mLvs.283.1±225.0 mL,P=0.003)and the postoperative hospital stay duration(6.9±2.2 dvs.9.0±3.5 d,P=0.001)in the HALLR group were significantly less than those in the OLR group.
Discussion
With the developments of surgical technique and instruments,LLR is now widely accepted as an alternative to OLR.HALLR is a special form of laparoscopic surgery that combines the merits of laparotomy and laparoscopicsurgery.In this study,we retrospectively analyzed the surgical outcomes of 49 well-matched patients in each group.All the lesions were successfully removed,and none of the patients died during the perioperative period.Less bleeding amount and faster postoperative recovery were observed in the HALLR group.These results were consistent with those of some previous reports(4,7,8),which demonstrated the safety of HALS.
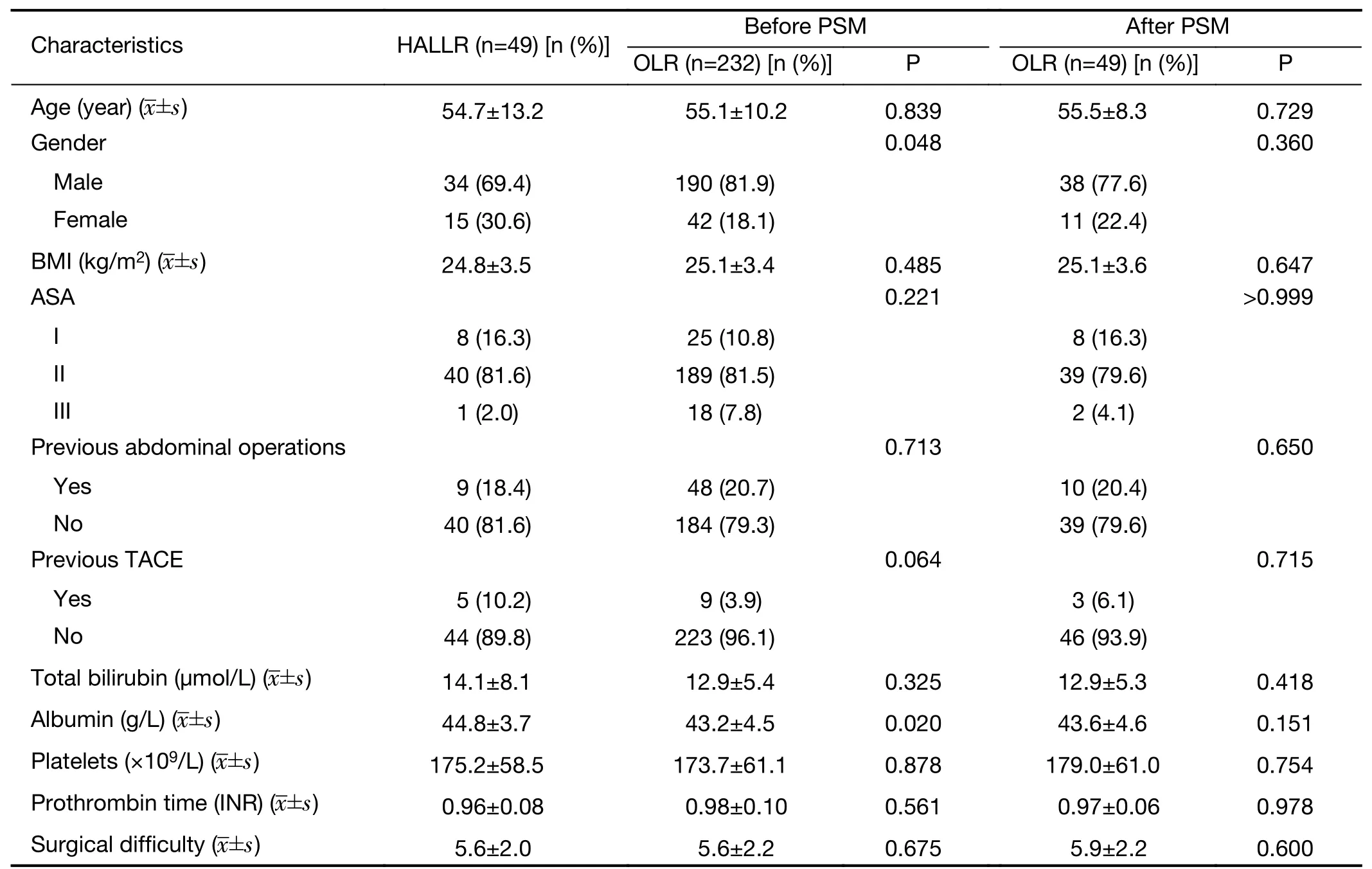
Table 1 Comparison of baseline characteristics before and after PSM
In Louisville statement,laparoscopic surgery is recommended for left lateral lobe resection as well as for lesions located in the peripheral segments(1).However,LLR for lesions located in the posterosuperior lobe,caudate lobe,and lesions adjacent to the major vessels remains challenging.Surgeons from Korea compared the outcomes of right posterior sectionectomy between 24 laparoscopy and 19 open surgeries.The operation time was significantly longer in the laparoscopy group(21).The main reasons for this were poor exposure and difficulty in bleeding control.It is noteworthy that HALLR provide better visualization and control of hemorrhage,which perplex surgeons in laparoscopy surgery.
In this study,left lateral lobe resection was excluded.More than 20% of the cases in each group had lesions of size≥5 cm or in the proximity to major vessels.More than half of the lesions were located in segments I,VII,and VIII.Such a scenario poses challenges in pure LLR.Despite these difficulties,in the present study,all the surgeries were successfully completed with hand assistances in the abdominal cavity.The operation time in the HALLR group was found to be similar to that in the OLR group(207.2±60.9 minvs.208.2±60.6 min,P=0.935).In addition,the laparoscopic approach provided better identification of the small vessels under magnified viewing(7).Precise intervention to the small blood vessels during the surgery led to lesser bleeding in the HALLR group(177.8±217.1 mLvs.283.1±225.0 mL,P=0.003).These results provided powerful evidence about the advantages of HALS in difficult liver resection.
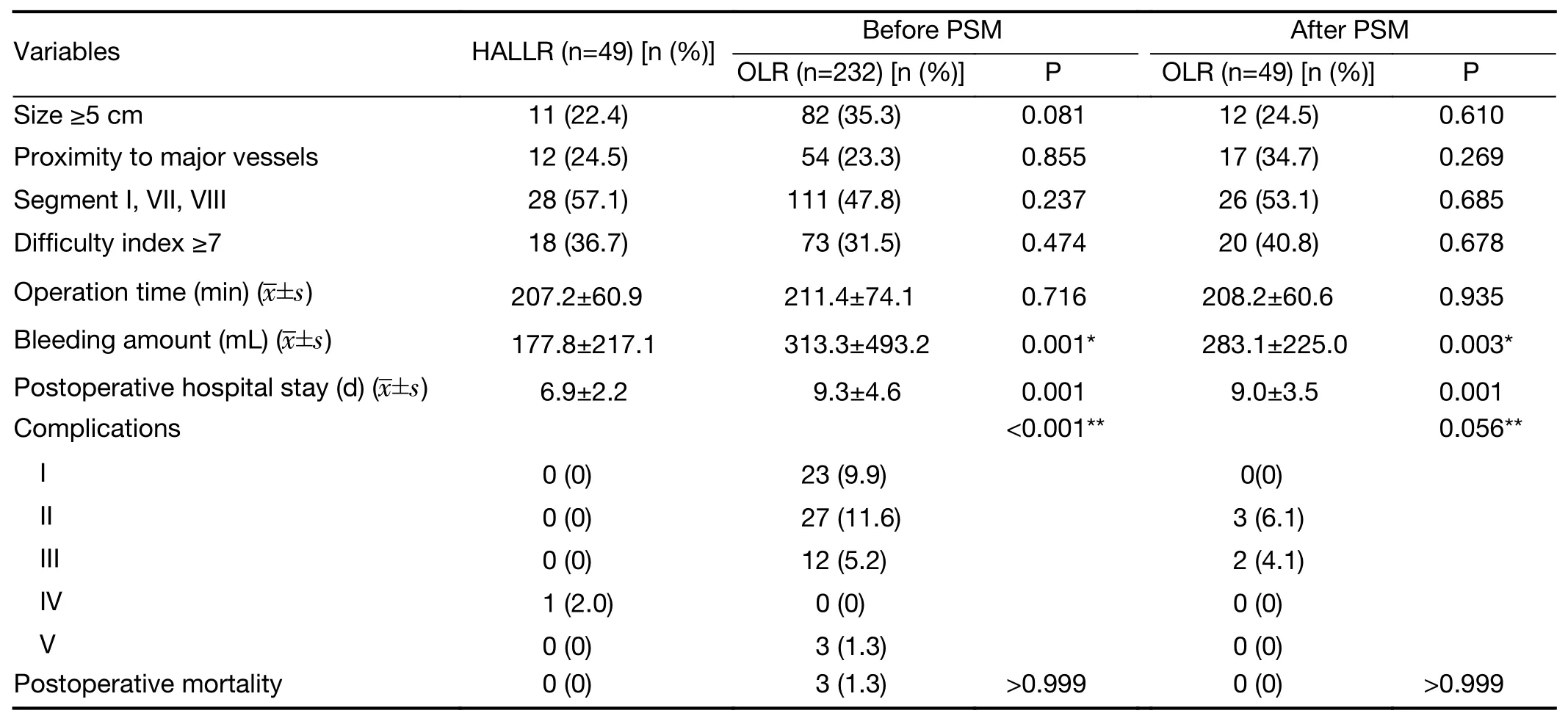
Table 2 Comparisons of operation information and surgical outcomes
Laparoscopy surgery thus offers advantages of reduced postoperative pain,intestinal dysfunction and hospital stay(22).In the present study,patients receiving HALLR recovered faster than those receiving OLR.The postoperative hospital stay was about 2 d shorter in the HALLR group than in the OLR group.These results were consistent with those of previous studies with respect to comparison of laparoscopy surgery with laparotomy(23-25).The number of patients suffering from postoperative complications was also fewer in the HALLR group,and the P value was found to be marginally significant.We believe that positive result may be obtained if the sample size is enlarged.
However,there were some limitations in this study.First,hemihepatic vascular occlusion was conducted more frequently in OLR and Pringle maneuver in HALLR.It was inappropriate to compare the vascular occlusion time between the two groups.Second,as we only illustrated the performance of HALS in liver resection and both benign lesions and malignant lesions were taken into analysis.As a result,the survival outcomes have not been displayed in the study.Third,the conversion to OLR was excluded in this study.The selection bias was inevitable,which may yield favorable results to HALLR.In the future,the risk for conversion will be analyzed and sufficient preoperative evaluation should be conducted to selected appropriate cases for HALLR.
Conclusions
We demonstrated that HALS is a feasible and safe approach for liver resection,including resection of lesions located in the posterosuperior lobe,caudate lobe,as well as those proximal to major vessels.HALLR offers the advantages of bleeding control and faster recovery after surgery.In the future,the survival outcomes of liver cancer patients receiving HALLR should be analyzed,and the performances of HALLR and pure LLR should be compared.Retrospective study on a larger sample size and more dedicated clinical trials are needed in the future.
Acknowledgements
This work was supported by PUMC Youth Fund/Fundamental Research Funds for the Central Universities(No.3332016031)and National Key Research and Development Plan(No.2016YFD0400604-03).
Footnote
Conflicts of Interest:The authors have no conflicts of interest to declare.
 Chinese Journal of Cancer Research2019年5期
Chinese Journal of Cancer Research2019年5期
- Chinese Journal of Cancer Research的其它文章
- A study on service capacity of primary medical and health institutions for cervical cancer screening in urban and rural areas in China
- Medical expenditures for colorectal cancer diagnosis and treatment:A 10-year high-level-hospital-based multicenter retrospective survey in China,2002-2011
- Texture analysis on gadoxetic acid enhanced-MRI for predicting Ki-67 status in hepatocellular carcinoma:A prospective study
- Machine-learning-assisted prediction of surgical outcomes in patients undergoing gastrectomy
- Prognostic significance of lymphovascular infiltration in overall survival of gastric cancer patients after surgery with curative intent
- Phosphoglucose isomerase gene expression as a prognostic biomarker of gastric cancer
