Intraparenchymal hemorrhage after surgical decompression of an epencephalon arachnoid cyst: A case report
Xue-Jian Wang
Xue-Jian Wang, Department of Neurosurgery, Affiliated Hospital 2 of Nantong University(Nantong First People's Hospital), Nantong 226001, Jiangsu Province, China
Abstract BACKGROUND This study reports the clinical presentation of intraparenchymal hemorrhage as a rare complication after surgical decompression of an intracranial epencephalon arachnoid cyst (IEAC) at the posterior cranial fossa.CASE SUMMARY The clinical information of a patient with an IEAC was reported, and the related literature was reviewed. A female patient with nausea presented to our hospital.Computed tomography demonstrated an IEAC located at the posterior cranial fossa, which was large and required surgical intervention. After operation,postoperative intraparenchymal hemorrhage was detected. She had a good recovery with conservative treatment 1 mo later.CONCLUSION Though postoperative intraparenchymal hemorrhage is rare after surgical decompression of an IEAC, more attention should be paid to such a complication.
Key Words: Intracranial arachnoid cyst; Surgical decompression; Hemorrhage;Complication; Case report
INTRODUCTION
Intracranial epencephalon arachnoid cysts (IEACs) represent a relatively rare disease,accounting for less than 1% of all brain mass lesions[1]. IEACs are usually benign collections of cerebrospinal fluid (CSF), partly accompanied by a placeholder effect.Most patients with IEACs are asymptomatic and found incidentally. However, some of them may become symptomatic due to cyst enlargement. I here report a case of intraparenchymal hemorrhage as a rare complication after surgical decompression of an IEAC.
CASE PRESENTATION
Chief complaints
A previously healthy female (28 years old, right-handed) was admitted to our hospital with intractable nausea.
History of present illness
Medical treatment for nausea failed.
History of past illness
This patient had no history of past illness.
Personal and family history
This patient had no other previous medical history.
Physical examination
No neurological deficit or papilledema was observed in her neurological examination.
Laboratory examinations
Laboratory tests were in the normal range.
Imaging examinations
In her brain magnetic resonance imaging scan, a large fluid collection could be found at the posterior cranial fossa with a size of 6 cm × 7 cm (Figure 1A-C).
FINAL DIAGNOSIS
A large IEAC.
TREATMENT
Considering the mass effect and intractable nausea, the patient was admitted to the hospital for surgical decompression. During the operation, after occipital craniotomy,cerebellum dura was opened, and the wall of the cyst was resected and fully separated. Indirect surgical approaches with conservative procedures were used to gradually decompress this arachnoid cyst. Arachnoid cyst was opened and decompressed to the cisterna magna to avoid recurrence.
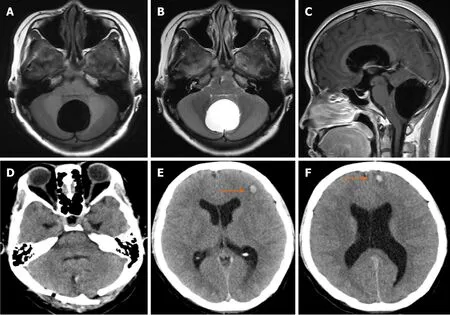
Figure 1 Imaging examinations. A-C: Axial T1-weighted (A), axial T2-weighted (B) and sagittal T1-weighted (C) magnetic resonance images of the head showing a well-defined lesion of cerebrospinal fluid in the subtentorial region; D: It prompts cysts is good decompression; E and F: Two foci of intraparenchymal hemorrhage were found in the frontal lobe.
OUTCOME AND FOLLOW-UP
From the postoperative routine review of computed tomography (CT), a good decompression was achieved (Figure 1D), while two focuses of intraparenchymal hemorrhage were found in the frontal lobe (Figure 1E and F). She had slight vomiting and headache. The neurological examination was normal. She achieved an excellent recovery 1 mo later with conservative treatment.
DISCUSSION
IEACs are collections of intro-arachnoidal CSF, which account for less than 1% of all non-traumatic brain mass lesions and are often asymptomatic[1,2]. Nevertheless, the patients can be symptomatic due to cyst enlargement. Early diagnosis is critical as cysts cause the mass effect, which may require surgical intervention. The therapeutic schemes of IEACs remain controversial because of their variable manifestation patterns. Therapeutic options for larger cysts include CSF shunting, endoscopic fenestration, or craniotomy and open fenestration[3].
IEACs are frequently found in the middle cranial fossa in 50% of cases, with a slight predilection for the left side and the male gender[1]. Symptoms include headache,behavioral problems, ataxia, cerebellar signs, nausea, vomiting, visual disturbance,and seizures. Deet al[4,5]have reported that the most common symptom is a headache,followed by behavioral problems. For example, a change in personality and impaired mental function are the second most frequently reported symptoms and sometimes may be the only presenting features. Its origin remains unknown. The diagnosis is always apparent in CT. The most effective treatment for IEACs is surgical decompression of the cyst[6,7]. In clinical practice, if there is a space-occupying lesion or apparent clinical symptoms, it is considered that there is an operative indicator.
There are several complications after the surgical decompression of arachnoid cysts,including recurrence, hydrocephalus, subdural hematomas, cerebral edema, infection,and seizures[3,8-10]. However, intraparenchymal hemorrhage in the brain parenchyma is a rare complication after the decompression of IEACs[11,12]. Few studies have reported the hemorrhage after surgical decompression of IEACs[11-13]. To the best of our knowledge, the first description of intraparenchymal hemorrhage after surgical decompression of IEACs was reported by Borgeset al[14]in 1995. They reported a case of brainstem hemorrhage after surgical removal of IEAC of the lateral fissure[14]. Until now, the pathogenesis of such complication remains largely unexplored, which may be attributed to reperfusion injury[11]. It is well known that intracerebral hemorrhage may occur after rapid decompression of chronic subdural hematomas, and hypoperfusion of brain parenchyma after surgical decompression for cerebral tumor has also been reported[11,15,16]. It is believed that hemorrhage could be mainly attributed to the rapid decompression of the cyst, although the risk of rapid decompression was considered, and a gradual decompression of IEAC, in this case, was given to avoid rapid decompression and decrease the incidence of such rare complications.
CONCLUSION
Collectively, hemorrhage in a postoperative arachnoid cyst is a rare complication.However, it is critical to establish a timely and accurate diagnosis after a routine postoperative CT scan. Symptoms and signs are usually non-specific, and the diagnosis relies on a precise history, imageological examination, and careful observations.
 World Journal of Clinical Cases2021年1期
World Journal of Clinical Cases2021年1期
- World Journal of Clinical Cases的其它文章
- Endoscopic salvage treatment of histoacryl after stent application on the anastomotic leak after gastrectomy: A case report
- Residual tumor and central lymph node metastasis after thermal ablation of papillary thyroid carcinoma: A case report and review of literature
- Necessary problems in re-emergence of COVID-19
- Simultaneous bilateral acromial base fractures after staged reverse total shoulder arthroplasty: A case report
- Krukenberg tumor with concomitant ipsilateral hydronephrosis and spermatic cord metastasis in a man: A case report
- Immunosuppressant treatment for IgG4-related sclerosing cholangitis: A case report
