Magnetic resonance imaging-guided prostate biopsy-A review of literature
Kulthe Rmesh Seethrm Bht , Srinivs Smvedi ,Mrio Covs Moshovs Fikret Ftih Onol Shnnon Roof Trvis Rogers Vipul R.Ptel Annthkrishnn Sivrmn
a Department of Urology, AdventHealth Global Robotics Institute, Celebration, FL, USA
b The Hays Medical Centre, University of Kansas Health System, Hays, KS, USA
c Chennai Urology and Robotics Institute, Chennai, Tamilnadu, India
Abstract Objective: Multiparametric magnetic resonance imaging(MP-MRI)helps to identify lesion of prostate with reasonable accuracy.We aim to describe the various uses of MP-MRI for prostate biopsy comparing different techniques of MP-MRI guided biopsy.Materials and methods: A literature search was performed for “multiparametric MRI”, “MRI fusion biopsy”,“MRI guided biopsy”,“prostate biopsy”,“MRI cognitive biopsy”,“MRI fusion biopsy systems”,“prostate biopsy”and“cost analysis”.The search operation was performed using the operator “OR” and “AND” with the above key words.All relevant systematic reviews,original articles, case series, and case reports were selected for this review.Results: The sensitivity of MRI targeted biopsy (MRI-TB) is between 91%-93%, and the specificity is between 36%-41% in various studies.It also has a high negative predictive value(NPV) of 89%-92% and a positive predictive value (PPV) of 51%-52%.The yield of MRI fusion biopsy (MRI-FB) is similar, if not superior to MR cognitive biopsy.In-bore MRI-TB had better detection rates compared to MR cognitive biopsy, but were similar to MR fusion biopsy.Conclusions: The use of MRI guidance in prostate biopsy is inevitable, subject to availability,cost, and experience.Any one of the three modalities (i.e.MRI cognitive, MRI fusion and MRI in-bore approach) can be used.MRI-FB has a fine balance with regards to accuracy, practicality and affordability.
KEYWORDS MRI targeted biopsy;MRI fusion biopsy;MRI cognitive biopsy;MRI fusion technology;Prostate biopsy
1.Introduction
Transrectal ultrasound (TRUS)-guided prostate biopsy is commonly used to diagnose prostate cancer(PCa).The use of TRUS for prostate biopsy was first described by Watanabe et al.in 1968 [1].The next major advancement in prostate biopsy is the sextant biopsy, described by Hodge et al.in 1989 [2].The appearance of the prostate malignant lesion on a TRUS could be either hypoechoic, isoechoic, or hyperechoic,none of which are pathognomonic.With these limitations in TRUS biopsy, magnetic resonance imaging(MRI) guided biopsy was investigated due to increased quality of images obtained by MRI.
In a Nobel prize winning paper in 1946, Felix Bloch proposed that the atomic nucleus acts like a magnet with momentum due to spinning protons, and its first ever clinical application [3].In 1960, Damadian et al.[4] differentiated between malignant and normal tissue in a rat,which formed the basis of use of MRI today.The use of MRI is popular due to its contrast resolution, especially in detecting soft tissue lesions.With further advancement in MRI and the use of multiparametric MRI (MP-MRI), radiologists were able to identify lesions with reasonable accuracy,especially in PCa.These advances triggered the use of MP-MRI for prostate biopsy, either in the form of in-bore magnetic resonance imaging targeted biopsy (MRI-TB),MRI cognitive biopsy(MRI-CB)or MRI fusion biopsy(MRI-FB).
2.Methods
A literature search for articles in English was performed with PubMed,Google Scholar,WHO Hinari,Web of Science,Scopus and Cochrane library using the terms “multiparametric MRI”, “MRI fusion biopsy”, “MRI guided biopsy”, “prostate biopsy”,“MRI cognitive biopsy”,“MRI fusion biopsy systems”and “cost analysis”.Articles primarily after 2014 and other important studies prior to 2014 were selected and reviewed in this article.The search operation was performed using operator “OR” and “AND” with the above key words.All relevant systematic reviews, original articles, case series and case reports were selected for this review.
3.MP-MRI
MP-MRI has been used for the diagnosis and staging of PCa[5].The MP-MRI is a combination of high-resolution T2-weighted images (T2WI), dynamic contrast-enhanced MRI(DCE-MRI), and diffusion-weighted imaging (DWI) to assess the anatomy and detect tumours >0.5 cm[6-9].The prostate imaging reporting and data system (PIRADS) is a scoring system proposed by the European Society of Urogenital Radiology (ESUR) to diagnose PCa in the year 2012[10].Later, magnetic resonance spectroscopic imaging(MRSI), which was initially part of PIRADS, has been discontinued in PIRADS v2.0 [11].Specific MP-MRI performed using “detection protocol” is used in MP-MRI guided biopsy[12-14].Prior to the PIRADS scoring, the radiologist used the Likert scale, wherein without strict criteria the radiologist used a 5 point grading system based on overall impression.More radiologists are familiar with this system,though it is subject to interpreter variability [15].Both PIRADS and LIKERT scales had similar rates of decision to biopsy, with LIKERT performing better in identifying clinically significant prostate cancer (csPCa).Unlike PIRADS,LIKERT is flexible, intuitive, and allows the radiologist to use clinical data.However,it is useful only if the radiologist has sufficient experience and it has the drawback of being subjective [16,17].
In 2019, an international group comprised of the American College of Radiology(ACR),the ESUR and the AdMeTech Foundation published an updated PIRADS v2.1[18].DWI MRI is the dominant sequence in the peripheral zone, and T2 weighted (T2w) MRI is the dominant sequence in the transitional zone.The latest scoring system is more specific about the uses of b values in DWI and DCE temporal resolution,especially in scores 2 and 3,thus adding more clarity to PIRADS score.The changes in T2w are in assessment in scores 1 and 2 defining encapsulated nodule and atypical nodules [18].
Final PIRADS v2.1 assessment categories [18]:
·1 Very low (clinically significant cancer highly unlikely)
·2 Low (clinically significant cancer unlikely)
·3 Intermediate (clinically significant cancer equivocal)· 4 High (clinically significant cancer likely)
·5 Very high (clinically significant cancer highly likely)
Recently published prospective validation studies of PIRADS v2 show the detection rates for PCa were 35%-39%,60%-72% and 91% for PIRADS 3, 4, and 5 lesions, respectively.The rates of csPCa were 17%-23%, 34%-49% and 67%-77% for PIRADS 3, 4, and 5, respectively [19,20].Pepe et al.[21]suggested the use of PIRADS 3 or above as the safe cutoff for MRI-TB, wherein 83.8% of the csPCa were diagnosed, with a false-negative rate of 16.2%, which negated the need for saturation biopsy.In a meta-analysis of 21 studies evaluating the diagnostic performance of PIRADS v2,the reported pooled sensitivity and specificity were 0.89(95% confidence interval [CI] 0.86-0.92) and 0.73 (95% CI 0.60-0.83) [22].In another meta-analysis by Zhang et al.[23],13 studies were reviewed and it was concluded that the pooled sensitivity and specificity were 0.85 (95% CI 0.78-0.91) and 0.71 (95% CI 0.60-0.80), respectively.A study comparing the reader agreement of six highly experienced uroradiologists from six institutions showed moderate reproducibility (kappa=0.55) [24].A subsequent study by Muller et al.[25] showed kappa interpreter agreement for overall suspicion score, T2W in the peripheral zone (PZ),T2W in the transitional zone(TZ),DWI,and DCE-MRI of 0.46,0.47, 0.37, 0.40 and 0.46, respectively.The limitations of MP-MRI include limited sensitivity for the detection of PCa in the TZ, especially in the setting of benign prostatic hyperplasia (BPH).Similarly, BPH nodules can mimic cancerous lesions, especially in DWI.Numerous benign and premalignant lesions like granulomatous prostatitis, adenosis, and prostatic intra-epithelial neoplasia can mimic PCa [26].
4.MRI-TB
With many multicentric prospectively designed studies and systematic reviews (Table 1) confirming superiority of the use of MRI guided TRUS biopsy, the current debate is if one should continue doing the systematic biopsy along with MRI guided biopsy.MRI-TB is highly sensitive when compared to standard TRUS biopsy and has better detection rates of csPCa.Combining both has been suggested to increase the yield of the biopsy [27].The sensitivity of MRI-TB is between 91%-93% and the specificity is between 36%-41% in various studies.Also,it has a high negative predictive value of 89%-92% and a positive predictive value of 51%-52%[28-30].
4.1.Approaches to MRI-TB
MRI-TB has three main approaches:
4.1.1.MRI-CB
MRI-CB involves visual registration by the operator,creating a mental map of the MRI images including suspicious lesions, and targeting those spots while doing a TRUS-biopsy.The operator mentally analyses the images and measures various distances using three-dimensional (3D) spatial reasoning and recognition of set patterns in MR images,thus locating the target spot.With regards to its yield,MRICB is superior to the systematic prostate biopsy, and in expert hands it could probably equal the MRI-FB in diagnostic yield.
Sciarra et al.[40]prospectively compared two groups of men, one undergoing systematic biopsy and the other undergoing MRI-CB, with significant differences in PCa detection rates in both groups (24.5% vs.45.5%, p=0.01).Similarly, Lee et al.[41] demonstrated a higher yield in previous negative biopsy patients who had MRI-CB vs.systematic core biopsy(28.8%vs.3.6%,p=0.012).MRI-CB was particularly useful in anterior and apical tumours that are often missed in systematic biopsy.
4.1.2.MRI-FB
This method involves a real time fusion of MP-MRI images which are superimposed on the real time TRUS images,thus targeting the lesion seen on MP-MRI during the prostate biopsy.There are several commercially available systems for co-registering MP-MRI scans with real time ultrasound(US) (Table 2).Of these, URONAV and Artemis are the two most commonly used systems throughout the United States.These machines differ in the following ways [42]:
- Registration algorithm-The prostate can become deformed for a number of reasons, such as a full bladder,endorectal coil during MP-MRI,patient position,haemorrhage, intra procedural distortion, etc.Based on the ability to compensate for the distortion, the type of fusion is classified as
a.Rigid-Does not consider the organ deformation and could potentially lead to suboptimal anatomic registration.
b.Elastic-Accounts for the gland deformation and provides a better fusion leading to improvement in accuracy.
- Strategy of navigation
a.Organ-based-This involves retrospective guidance,where the device performs an organ-based navigation in which the location of the US transducer, the proposed needle target, and the prostate are mapped retrospectively using software programs.
b.Electromagnetic tracking-This is a real time tracking system using a Global Positioning System (GPS) like tracking tool that tracks using electromagnetic fields and angle sensors.The drawback to this type of tracking is that it is cumbersome and expensive, as it uses extra hardware, like an electromagnetic field generator near the patient and a sensor on the US probe.
- Post biopsy needle track documentation
a.Operator performs a US of the prostate with biopsy needle in situ to exactly track the area of interest.
b.Approximation of the biopsy needle based on orientation relative to the target and US transducer.
- Design of the robotic arms
Some systems have articulating arms with steppers and coders to reduce operator dependency, thus improving consistency and accuracy, while other systems merely guide the operator to target the desired area for sampling.
4.1.2.1.Artemis.Using computer software, the operator identifies the lesions and marks them prior to the biopsy.During the procedure, the Artemis fusion platform initially calibrates the MP-MRI images and the real time US image to the mechanical arm, developing a 3D fusion mode.The machine can track and save the needle tract,which is useful for patients who are on active surveillance during repeat biospy[43].This system is highly accurate,with an accuracy of about 1.2 mm±1.1 mm [44].Artemis device had thrice more detection rates of cancer versus the standard biopsy[43].However, the main drawback of this system is that the biopsy involves two devices, and change in patient position can alter the fusion requiring the procedure to be repeated.The robotic arm has a limited degree of freedom (doF), the prostate can become deformed during apposition of the TRUS probe and the fusion may not be accurate.
4.1.2.2.UroNav.UroNav uses a free hand approach to electromagnetically track the motion of a real-time transrectal US probe to MP-MRI loaded and has an accuracy of 2.3 mm±0.9 mm [45].The advantage of this system is that it enables rigid and elastic registration, and due to its freehand nature, it allows the operator to perform the procedure in the office.
There have been reports of MRI-FB being performed via the transperineal route using the conventional robotic system, by switching from transrectal to transperineal modules.The BiopSee system is used to perform transperineal biopsy, and it includes a transrectal probe with a mechanical stepper that aids in performing the biopsy transperineally [46].
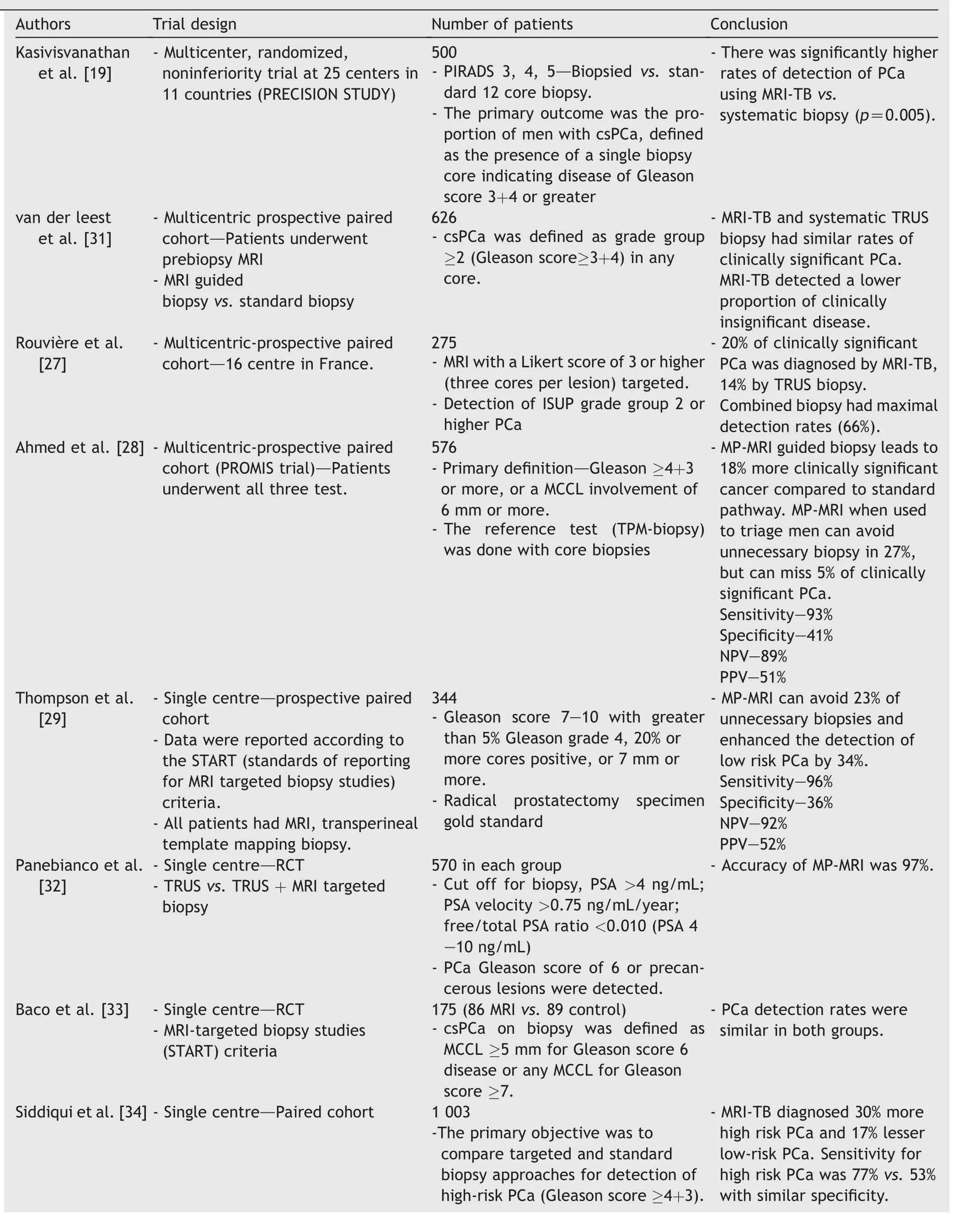
Table 1 Summary of studies comparing between MRI-targeted biopsy and systematic biopsy.

Table 1 (continued)
The major challenges these systems face are the associated cost and learning curve.It requires continuous learning and feedback between different specialities.The MRI fusion technology comes with significant cost and requires an initial investment with a steep learning curve.Mendhiratta et al.[47] showed the yield of MRI-FB increased over 33 months from 63% to 86%, thus supporting its use and demonstrating a learning curve.Inaccurate segmentation of MP-MRI images and misregistration of the MP-MRI images or transrectal US images can lead to discrepancies in targeting.In order to overcome the registration and targeting errors, it is a norm to obtain at least two spatially distributed samples from the target [48].
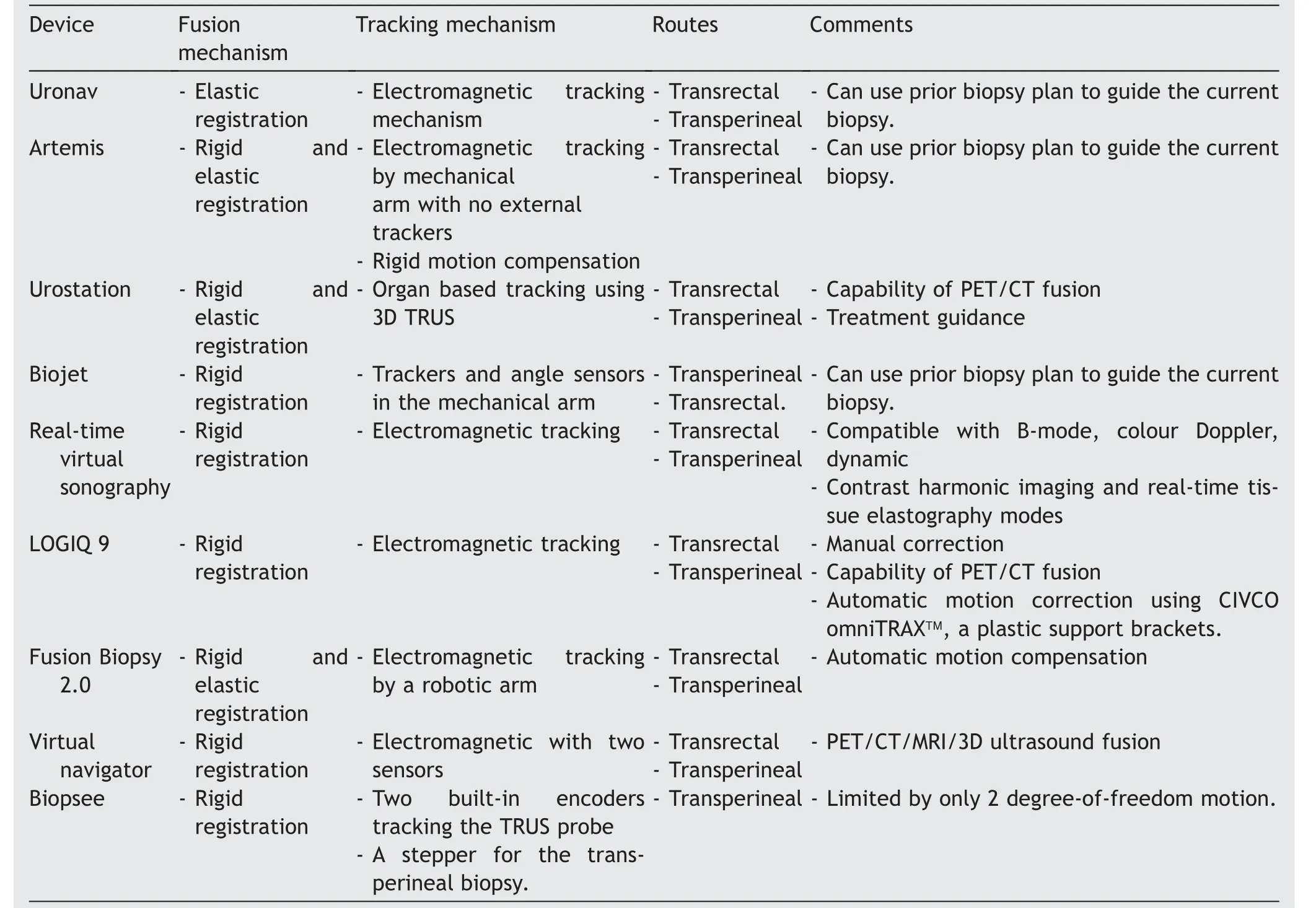
Table 2 Comparison of different MRI-fusion biopsy systems.
4.1.3.In-bore MRI target biopsy
This technique involves obtaining tissue samples with direct MRI guidance in MRI gantry, thus allowing the operator to target the lesion in real time.Though traditionally done using the open MRI system, this technique is now being performed in closed systems, as well using either 1.5 T or 3 T MRI systems.The biopsy can be performed either transrectally or transperineally.DynaTRIM is a commonly used portable device used to perform the in-bore biopsy transrectally[49].The patient is placed in a prone position and the device is fixed underneath the patient; it has an adjustable needle guide that has three degrees of freedom(cranial/caudal, anterior/posterior and left/right).Once positioned, a rectal sleeve is placed and Sagittal T2WIs are obtained to position the arm in a neutral position.Axial images are then processed in the DynaTRIM workstation to target the lesion [49].A key advantage of this method is that any series of MRI can be used to target the lesion effectively.After identification of the lesion, the software plans the trajectory of the 18-gauge needle to biopsy the prostate.This procedure has a learning curve of about 25-30 patients, and takes about 30 min with an additional target taking about 15 min [48].
The mainadvantageofthistechniqueisthat one can target the biopsy site more accurately.However, the evidence to support its usefulness in small lesions is at best anecdotal,and the data on the exact size of the lesion where this might be advantageous are lacking.The main limitations of this technique are its limited availability, long procedure time, and cost.Another drawback is the logistic issue to perform such a procedure by a urologist amidst their busy practice(Table 3).
4.1.4.Comparison between different MRI biopsy
techniques
There are various studies that show the superiority of the MRI-TB over the conventional standard 12 core biopsy.However, when it comes the comparison between the individual modalities of MRI-TB, the data are scarce.Though the current available literature does not show if one is superior over the other, MRI-FB is more popular, probably because it is practical and can easily be incorporated into the work flow.The MRI-CB may have similar advantages in terms of its practicality and lower cost.There is evidence suggesting the superiority of MRI-fusion technology over the cognitive biopsy.Table 3 compares different modalities of MR guided biopsy.
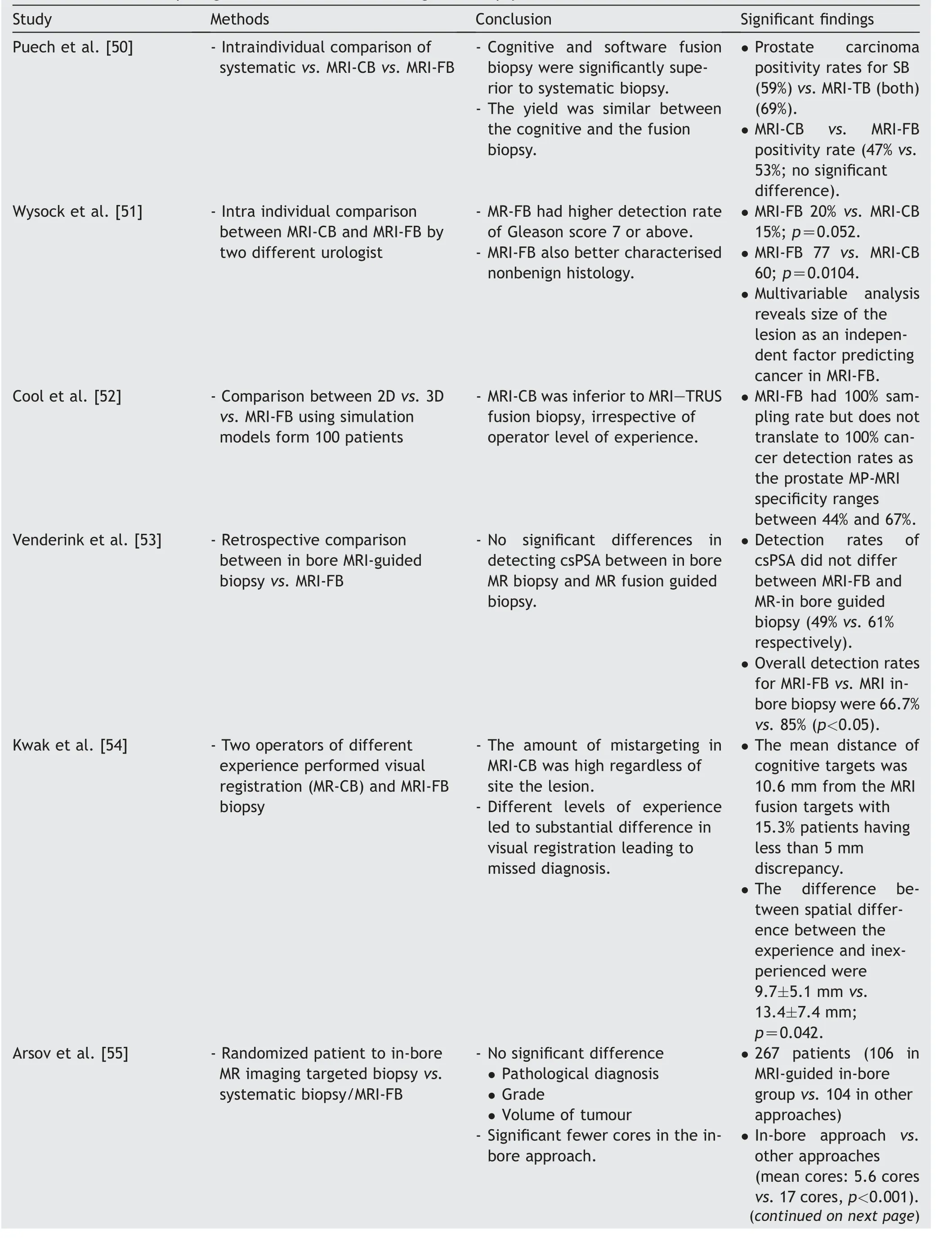
Table 3 Studies comparing different modalities of MR-guided biopsy.
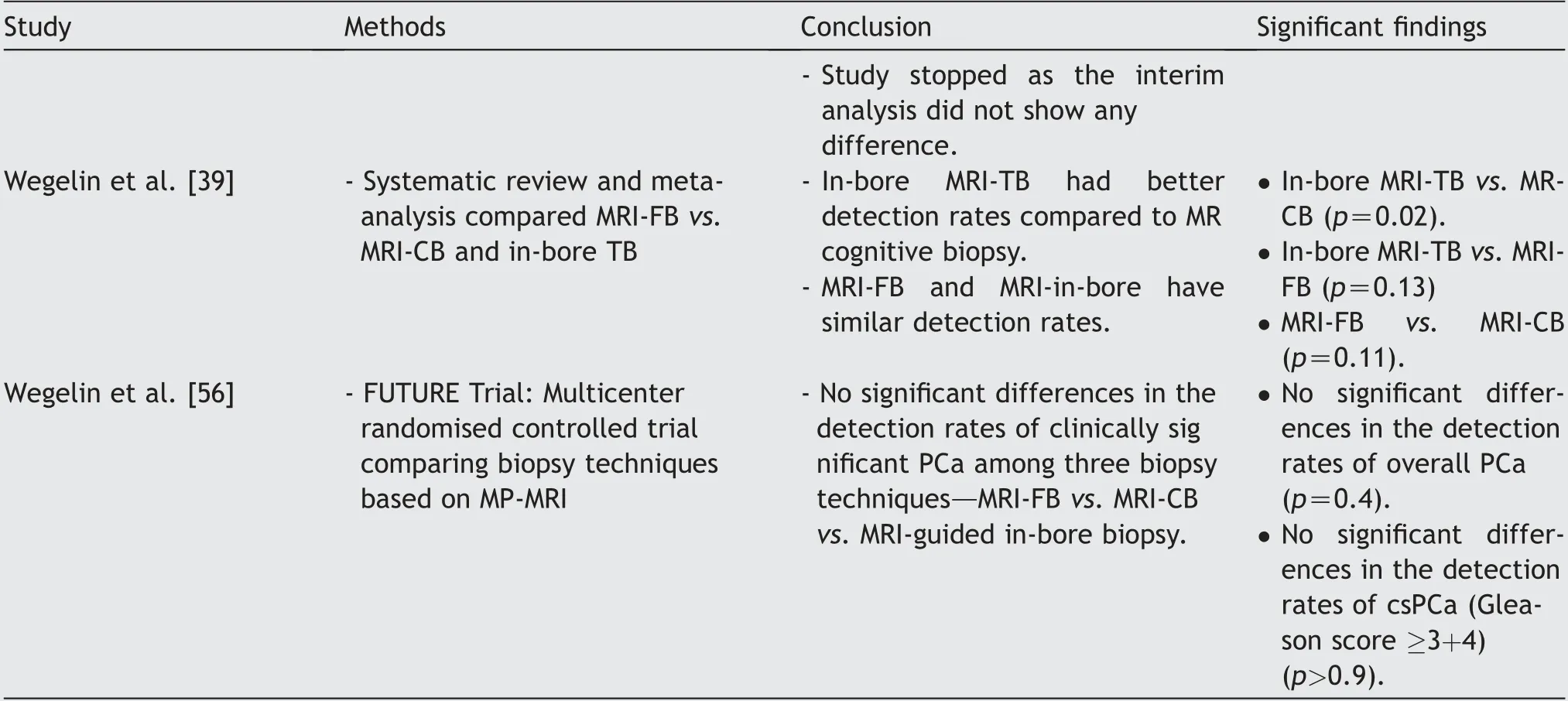
Table 3 (continued)
4.1.5.MRI guided transperineal biopsy
Transperineal biopsy has recently gained popularity, as transrectal biopsy has some disadvantages that are overcome by a transperineal route.A transrectal biopsy necessitates the use of prophylactic antibiotics because the needle passes through the rectum.Until now, flouroquinolone has been advocated as the antibiotic of choice, but the use of this particular group of antibiotics has been questioned for several reasons.First, its use is now restricted by the Federal Drug Agency(FDA).In 2016,the FDA advised against its use unless deemed necessary, due to the risk of permanent disabling joint issues[57].Second,the readmission rates following the quinolone use were similar to no antibiotic use, suggesting increasing antibiotic resistance due to the widespread use of fluoroquinolone[58,59].Therefore,this has led to the use of either a combination of antibiotics or the use of carbapenems as prophylaxis for prostate biopsy[60].In this context,rectal swab culture-specific antibiotic use is more effective[61].For the above-mentioned reasons, the transperineal route has been adopted in practice by many clinicians [58].The advantage of the transperineal biopsy compared to transrectal biopsy is the reduced chance of infection and better detection of cancer in the anterior zone of the prostate,with an almost 10% increased detection rate of these tumours[62-64].However, transperineal biopsy may have increased rate of urine retention[65].The targeting is done using either the freehand approach, the brachytherapy grid, or with robotic guidance.It is considered a relatively clean procedure,as the needle passes through the perineal skin.In a multicentric study by Pepdjonovic et al.[66],the readmission rate following transperineal biopsy was zero wherein the last 710 cases(59.5%)patients received a single dose of cephazolin as prophylaxis.
Historically, transperineal biopsy is usually performed under general anaesthesia.However, recently there are many studies reporting the feasibility of using local anaesthesia [67-69].Of note, the Cambridge Prostate Biopsy(CAMPROBE),developed by Thurtle et al.[70],has shown to be effective in administering local anaesthesia with reduced pain and 87% preference over TRUS biopsy.Technically, this is similar to the transrectal biopsy; the MRI targeted transperineal biopsy can be either cognitive guided, MRI software fusion biopsy, or in-bore MRI transperineal biopsy.MRI guided cognitive transperineal biopsy is done by placing the TRUS probe transrectally and using a brachytherapy grid.Using a stepper and a stabilizer, the prostate is imaged in sagittal and transverse views,and the needle is directed towards the target lesion site.The 5 mm grid spacing can accurately help in targeting the lesion.
MRI guided fusion transperineal biopsy has the same principles as the MRI fusion transrectal biopsy.The difference is that the software compensates for the needle tracking transperineally.One can perform this either with or without the brachytherapy grid.After capturing the US images, the software performs rigid/elastic registrations and suggests appropriate grid holes that can be used for target sampling.The MRI-FB systems capable of performing transperineal biopsy are listed in Table 3.In a comparison between the systematic template transperineal biopsy(TPB) and MRI fusion biopsy, the template biopsy missed 21% of clinically significant cancer and MRI-TB missed 20%,thus concluding that their detection rates are similar and should be used in combination [71].
The first transperineal in-bore imaging biopsy was reported in 2001,and was useful in patients with limited rectal access due to previous proctocolectomy or rectal stenosis[72].Visualase is a commercially available system used to perform transperineal biopsy, wherein the patient is supine and a needle guide template with fiducial marker is strapped onto the perineum.The software then plans the needle adjustments and positioning to target the correct hole to sample the target on the prostate [48].In view of its cumbersome nature and difficulty in incorporating the inbore MRI transperineal biopsy into the routine workflow of a clinician’s practice,it is not very popular.Of note is a study comparing the use of manual versus robotic template in the in-bore MR TB, which found the robotic template had statistically higher accuracy in needle placement (p<0.032)[73].
The iSR’obot Mona Lisa is a robot exclusively developed for the transperineal biopsy.It performs the biopsy through two transperineal skin punctures that act as a pivot, thus giving a biconical configuration of core positions.The TRUS probe images the prostate from base to apex and generates a 3D model of the prostate.This image is then fused with MRI images of the prostate,thus marking out the targets for biopsy.Once the Mona Lisa device is positioned, the robot automatically creates a map and moves to the desired position for the biopsy.Under the US guidance, the clinician fires the needle, which is monitored, and the robot positions itself to the next target.A standard transperineal biopsy can be completed in half an hour [74].
Pepe et al.[64] compared MRI targeted TRB versus MRI targeted cognitive transperineal biopsy.The study involved 200 patients who underwent standard template transperineal biopsy followed by MRI fusion transrectal biopsy of the suspicious lesions.These patients were then targeted again using MRI-targeted cognitive transperineal biopsy.Sixty cases were diagnosed with csPca,which was confirmed using an MP-MRI.Also, 20 of these cases were missed by MRI fusion, and only four were missed by MRI-CB.The major drawback of this study is that the definition of csPCa was restricted to two or more cores with Gleason score 6 or above,which is debatable.
4.1.6.Cost analysis of MRI-TB
With so many available options, the cost comes into consideration in choosing the optimal modality,based on the indication of the prostate biopsy.Compared to a standard TRUS biopsy under local anaesthesia,the cost of TRUS biopsy under sedation, the cost of transperineal template biopsy under general anaesthesia, MRI-FB under sedation and sedation in-bore prostate biopsy were significantly higher(1.9 vs.2.5 vs.2.5 vs.2.2, p<0.001).In the same series,cancer detection rates when compared to TRUS biopsy were higher in fusion biopsy (16% vs.36%, p<0.001) and transperineal template biopsy (16% vs.34%, p<0.001) [75].
In another cost analysis by Venderink et al.[76], the incremental cost-effectiveness ratio following a MRI-FB versus the systematic TRUS biopsy was $1 470 per quality-adjusted life year gained.An in-bore MRI guided biopsy would be cost effective if its sensitivity for csPCa is 11.8% higher than the sensitivity of MRI-FB [76].To improve the sensitivity of either modality, newer definitions of csPCa can be used.Also, to improve costeffectiveness, lowering the upper limit of the willingness to pay threshold recommended by National Institute for Health and Care Excellence (NICE) has been suggested.The major limitation of this study is that it depends on the input parameters into the complex calculation and as it was performed in Netherlands, one cannot extrapolate the findings to other populations[76].De Rooij et al.[77] concluded that MRI-guided biopsy is cost effective if the sensitivity of MRI guided biopsy is 90% for any PCa.
In order to cut down cost and avoid unnecessary biopsy in patients with lower suspicion of PCa, a biparametric MRI(bp-MRI)with axial T2WIs and diffusion weighted images(b values:0,100,800 and 2000)can be performed,as they are the two dominant parameters of PIRADS scoring.This exam has a high negative predictive value of 97%, and takes approximately 15 min to perform.Also, the corresponding apparent diffusion coefficient maps can be generated.However, the potential disadvantage is that dynamic contrast-enhanced imaging, which is a part of the MP-MRI,is lacking; as a result, lesions of equivocal score 3 in the peripheral zone may not be upgraded to 4.Seventeen percent of these PIRADS 3 lesions on bp-MRI had clinically significant malignancy, thus justifying need for performing biopsy on these lesions[78].Also,there are several reports suggesting follow-up using repeat MP-MRI in PIRADS 3 lesion, to avoid unnecessary biopsies, thus cutting overall cost [79-81].
5.Conclusion
The use of MP-MRI guidance in prostate biopsy is inevitable,and we have passed the point of doubt on its usage.However, depending on the availability, cost, and experience,any one of the three modalities (i.e.MRI cognitive, MRI fusion and MRI in-bore approach)can be used.MRI-FB has a fine balance with regards to accuracy, practicality and affordability.
Author contributions
Study concept and design: Vipul R.Patel, Kulthe Ramesh Seetharam Bhat, Ananthkrishnan Sivaraman.
Data acquisition: Kulthe Ramesh Seetharam Bhat, Marcio Covas Moschovas.
Data analysis: Travis Rogers, Fikret Fatih Onol.
Drafting of manuscript: Srinivas Samavedi, Kulthe Ramesh Seetharam Bhat.
Critical revision of the manuscript:Vipul R.Patel,Shannon Roof, Ananthkrishnan Sivaraman.
Conflicts of interest
The authors declare no conflict of interest.
 Asian Journal of Urology2021年1期
Asian Journal of Urology2021年1期
- Asian Journal of Urology的其它文章
- Single-port technique evolution and current practice in urologic procedures
- Robotic urologic surgery: Past, present and future
- Totally intracorporeal robot-assisted urinary diversion for bladder cancer(part 2).Review and detailed characterization of the existing intracorporeal orthotopic ileal neobladder
- Totally intracorporeal robot-assisted urinary diversion for bladder cancer(Part 1).Review and detailed characterization of ileal conduit and modified Indiana pouch
- The robot-assisted ureteral reconstruction in adult: A narrative review on the surgical techniques and contemporary outcomes
- An unusual scrotal mass:Morphological clues
