Mesenchymal stem cell treatment for peripheral nerve injury: a narrative review
Rui-Cheng Zhang , Wen-Qi Du , Jing-Yuan Zhang , Shao-Xia Yu, Fang-Zhi LuHong-Mei Ding Yan-Bo Cheng , Chao Ren, , De-Qin Geng
Abstract Peripheral nerve injuries occur as the result of sudden trauma and lead to reduced quality of life. The peripheral nervous system has an inherent capability to regenerate axons.However, peripheral nerve regeneration following injury is generally slow and incomplete that results in poor functional outcomes such as muscle atrophy. Although conventional surgical procedures for peripheral nerve injuries present many benefits, there are still several limitations including scarring, difficult accessibility to donor nerve, neuroma formation and a need to sacrifice the autologous nerve. For many years, other therapeutic approaches for peripheral nerve injuries have been explored, the most notable being the replacement of Schwann cells, the glial cells responsible for clearing out debris from the site of injury. Introducing cultured Schwann cells to the injured sites showed great benefits in promoting axonal regeneration and functional recovery. However, there are limited sources of Schwann cells for extraction and difficulties in culturing Schwann cells in vitro.Therefore, novel therapeutic avenues that offer maximum benefits for the treatment of peripheral nerve injuries should be investigated. This review focused on strategies using mesenchymal stem cells to promote peripheral nerve regeneration including exosomes of mesenchymal stem cells, nerve engineering using the nerve guidance conduits containing mesenchymal stem cells, and genetically engineered mesenchymal stem cells. We present the current progress of mesenchymal stem cell treatment of peripheral nerve injuries.
Key Words: axonal regeneration; exosomes; genetic engineering; mesenchymal stem cells;neural conduit; peripheral nerve; peripheral nerve injury; peripheral nerve regeneration;Schwann cells; sudden trauma
Introduction
Peripheral nerve injury (PNI) is a common clinical neurological disorder that is characterized by sensory, motor, and autonomic dysfunction of the trunk or limbs. Unlike the central nervous system, peripheral nerves can regenerate spontaneously after injury because of the activation of the intrinsic growth capacity of neurons (Willand et al.,2016). Neurons are the basic structural and functional units of the nervous system and their axons are supported by neurolemmocytes, Schwann cells, which can be either unmyelinated or myelinated. In the latter, the medullary sheath, which comprises myelin and proteins forming the cell membrane of Schwann cells (SCs), is wrapped around axons repeatedly, acts as an insulator and accelerates the transmission of nerve signals. The Schwann cell has a nucleus and cytoplasm and its outer basement membrane wraps around the myelin sheath and has protective and regenerating functions (Muzio and Cascella, 2020). After peripheral nerve damage the nerve begins to degrade in an anterograde manner and involves mononuclear cell infiltration, neuroedema and even neurodegenerative demyelinating changes (El Soury and Gambarotta, 2019; Martin et al., 2019). PNI repairs occur using nerve chemotaxis and contact guidance (Faroni et al.,2015). SCs, which are derived from neural crest precursor cells and require the participation of fibroblast growth factor, bone morphogenetic protein and wingless/integrated signaling pathways, play an important role in the composition of the peripheral nerve structure and nerve regeneration (Stuhlmiller and Garcia-Castro, 2012). However, spontaneous repair of defective nerves in the peripheral nerve system is partial and leads to insufficient functionality.
Although microsurgical repair of damaged peripheral nerves is the current preferred treatment, surgery for PNI has entered a bottleneck stage. At present, there are two main methods for surgically repairing PNI when the nerve gap exceeds 1 cm (Bassilios Habre et al., 2018): autologous nerve transplantation and allogeneic nerve transplantation. Of these, autologous nerve transplantation has been considered the “gold standard” for PNI repair (Labroo et al., 2019).The common surgical approach is the direct suture of the two stumps (end-to-end suture) when a gap is not present(Tos et al., 2013). With the rapid development of medical technology, anastomosis of the nerve bundle and functionbeam anastomosis have gradually become the focus of researchers as they enable better clinical outcomes than endto-end anastomosis of the outer membrane of the nerve(Sakthivel et al., 2020). The primary problem currently facing allogeneic nerve transplantation is still immune rejection.Some researchers have used immunosuppressants to protect the main components, such as nerve membrane cells and interstitial cells, but certain adverse reactions remain in longterm use, including problems with liver and kidney functions(Nakayama et al., 2010; Loboda et al., 2018). Overcoming immune rejection is the primary requirement for the application of this technique in clinical treatment (Winfree,2005; Campbell, 2008). Tissue engineering is an emerging discipline in the category of biological high technology. A suitable biological model is established by applying the principles of cell biology, biomaterials, tissue engineering,and growth factors to repair PNI. Over the years, the use of stem cells in tissue engineering has been examined. In addition to neural stem cells, mesenchymal stem cells (MSCs),adipose-derived MSCs, muscle-derived stem cells and induced pluripotent stem cells have been used in the treatment of PNI (Barton et al., 2017; Lv et al., 2018). However, the current approved therapies are still not satisfactory.
MSCs, a class of multipotent stem cells derived from the mesoderm, have been characterized as having high selfrenewal ability, multi-directional differentiation potential and low immunogenicity. Because of their ubiquity, they can be easily isolated from various tissues such as bone marrow,umbilical cord and placenta (Pereira et al., 2018). Thus, they are often used as an ideal seed cell in cell therapy, with important clinical and research value. Great breakthroughs have been made using them in cardiovascular diseases,neurological diseases, autoimmune diseases and bone repair(Bartolucci et al., 2017; Chen et al., 2019). So far, MSCs have been combined with biological tissue engineering using various techniques to improve the effect of PNI regeneration and repair, but each application method has certain advantages and disadvantages. Therefore, the optimal method for MSCs to repair PNI needs further exploration. This review assesses the various techniques of MSCs for PNI (Figure 1) and provides a scientific basis for the direction of future research.
Search Strategy and Selection Criteria
The initial literature search was performed on PubMed and the following keywords: “mesenchymal stem cells”, “peripheral nerve injuries”, “axonal regeneration”, “exosomes”, “neural conduits”, “genetic engineering” and combinations of those words. All fields were included in the search, which was limited to publications from 2000 to 2020. A second broad search was performed by PubMed using the above keywords with the aim to update information. No time limits were used.
Peripheral Nerve Injuries Causes and Endogenous Repair
Peripheral nerves injuries may be caused by excessive pressure, complex soft-tissue injury or limb ischemia with compartment syndrome (Maricevic and Erceg, 1997; Rosen et al., 2012; Wang et al., 2017). Nowadays, the most common cause of injury is road traffic accidents, particularly motorcycle crashes (Stanec et al., 1997). Approximately 5% of PNI cases were related to sports (Hirasawa and Sakakida, 1983). After suffering from PNI, a patient’s nerve injury prognosis can be divided into neurotmesis, axonotmesis and neurapraxia at the anatomic level (Lee and Wolfe, 2000; Table 1). Neurotmesis often occurs with nerve avulsions, massive trauma, and cutting injury. In neurotmesis, the prognosis is poor without surgical therapy. Recovery from this type of trauma, which involves in major axon loss, is usually delayed and deficient (De la Rosa et al., 2018).
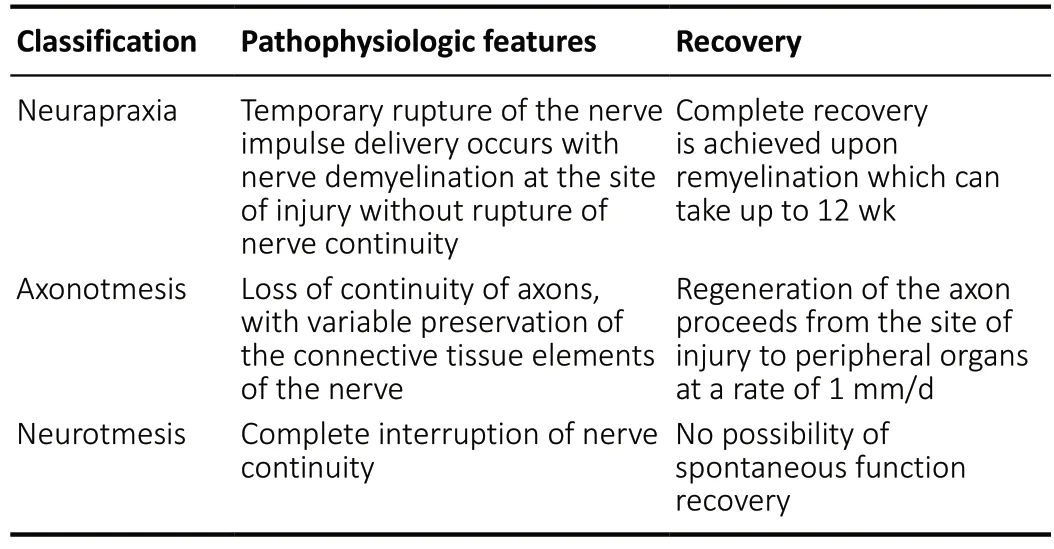
Table 1 |Classification of nerve injuries
Neurons in the peripheral nerve system can regenerate even after a severe PNI, but the potential for healing after accessible surgical therapy is dependent upon the brain as well as factors distal to the injury (Fex Svennigsen and Dahlin, 2013).Cortical plasticity has been identified as a contributary factor in the rehabilitation for patients with PNI (Baldassarre et al.,2020). Adult PNI patients may never achieve an encouraging outcome of functional recovery. This is because the brain is unable to accept the new afferent signaling patterns from the periphery caused by misdirection of the axonal regeneration after nerve injury. However, children show an admirable clinical recovery after PNIs, which may be because of the better regeneration and greater plasticity of the young brain (Chemnitz et al., 2013). At the time axons regenerate,the SCs have begun to proliferate, migrate and line up in nerves, which creates bands of Büngner and offers guidance substrates for the re-growth of axons (Bunn et al., 2019). SCs,specific type of cells that wrap around the axon of neurons in the peripheral nerve system, may play a vital role in the regeneration of axons (Gordon, 2020). The SCs in the bands of Büngner could produce an array of growth promoting factors,such as glial derived neurotrophic factor, ciliary neurotrophic factor, insulin like growth factor-1 and neuroregulin 1 (NRG1)(Springer et al., 1994; Tonazzini et al., 2017; Zhu et al., 2018;Godinho et al., 2020; Figure 2). PNI is followed by responses from the surrounding neural and non-neural cells, both proximally and distally to the damaged area. The endogenous repair process in neurons starts with an increase in its cell body size, the Nissl bodies dissolve and initiate a process of protein synthesis (Perrin et al., 2005). Then fragmentation of the axon is mediated by activated intrinsic proteases, including the ubiquitin-protease system and calpain (Zhai et al., 2003).Axonal and myelin debris is later phagocytosed by SCs and recruited macrophages that, attracted by specific chemokines,infiltrate through the myelin sheathing and broken bloodnerve-barrier (Coleman and Freeman, 2010; Figure 2).Clearance of myelin debris is a critical step for repair since myelin contains inhibitors of axonal regeneration (Berghoff et al., 2020). It is known that some adhesion proteins and growth factors affect axonal growth, Schwann cell proliferation and the formation of Büngner bands. Thus, understanding which proteins are critical in promoting the re-growth process will be useful for the improvements in peripheral nerve surgery and in the development to bridge nerve defects. It has been indicated that NRG1, probably along with laminin, is responsible for Schwann cell migration in nerve regeneration(Chang et al., 2013; Heermann and Schwab, 2013). The presence of laminin is also critical in the outgrowth of axons,and is now used clinically to reconstruct nerve defects (Kvist et al., 2011). Although axon regeneration and remyelination occur in the peripheral nerve system, the remyelinated axons often have a decreased internodal length and thinner myelin sheaths, which causes slower conduction (Sherman and Brophy, 2005). This is not only observed in the repair of acute nerve injury but is also observed after decompression of the median nerve in carpal tunnel syndrome and nerve repair in human median and ulnar nerves (Kim et al., 2000).These undesirable results might be due to either insufficient stimulation of redifferentiated SCs or inhibitory signals(Sherman and Brophy, 2005). Because of the unsatisfactory regaining of function, further improvements in PNI repair and regeneration have become an area of much interest.
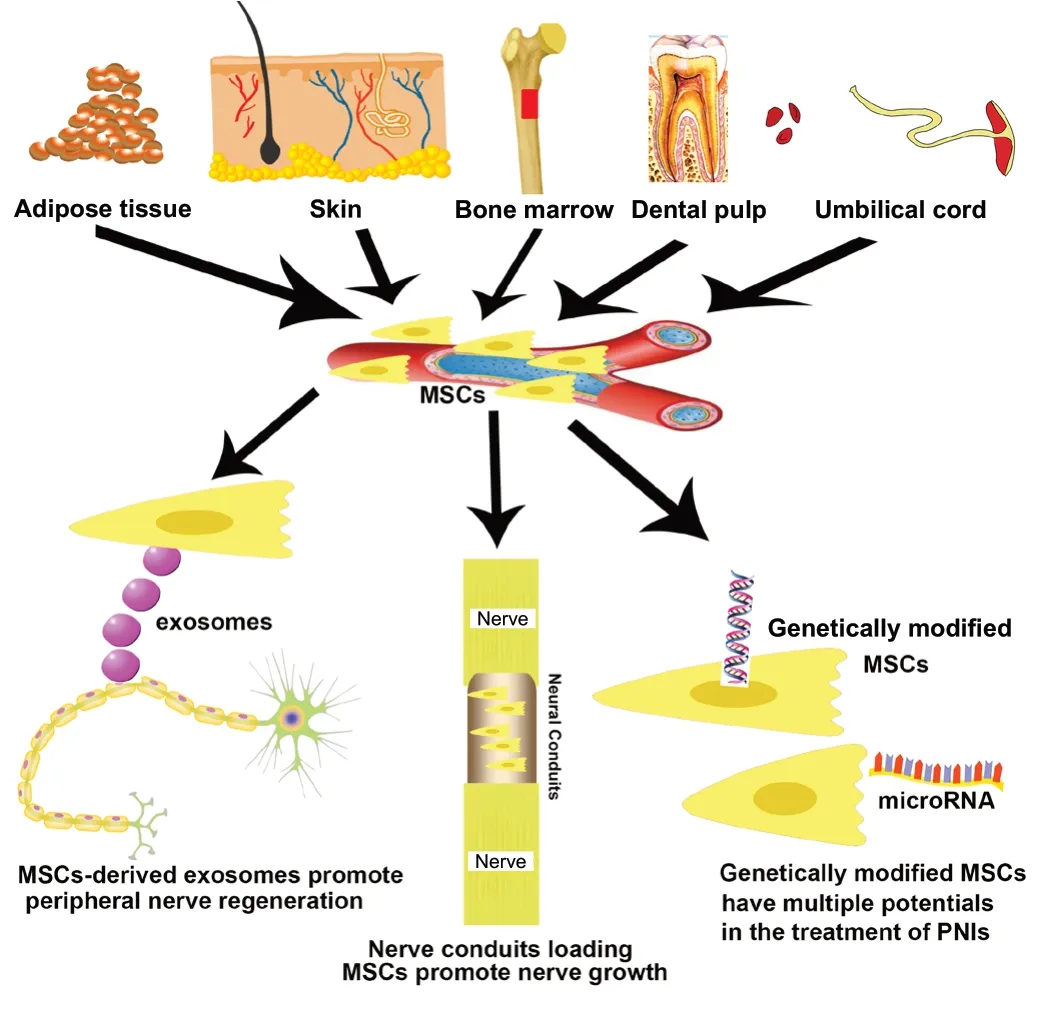
Figure 1 |Novel strategies using mesenchymal stem cells (MSCs) for curing peripheral nerve injury (PNI).
Mesenchymal Stem Cells Exosomes Based Therapy for Peripheral Nerve Injury Repair
Although some types of nerve damage can recuperate spontaneously, augmentation methods can accelerate the self-regeneration process after PNI. MSCs have been found to be a promising trigger for the regeneration following both axonal and nerve damage (Kizilay et al., 2017). MSCs are selfrenewing, multipotent progenitors that have the capability to promote neuroprotection and tissue-repair. MSCs can be isolated from the stromal vascular fraction of several tissues that are extrinsic to blood vessels, such as adipose tissue,skin, bone marrow and dental pulp (Lopez-Verrilli et al., 2016;Figure 1).
Exosomes, cell-derived small (~100 nm in diameter) vesicles,are one of several groups of secreted vesicles, including ectosomes (large membranous vesicles that are shed directly from the plasma membrane) and apoptotic blebs that are released by dying cells. Exosomes carry a cargo of lipids and proteins, as well as nucleic acid material in the form of DNA, mRNA, microRNA (miRNA), and noncoding RNA. These components could provide essential information associated with the physiological and pathological status. Exosomes can also convey these components to neighboring or even distant cells through circulation and participate in many biological processes and cell-to-cell communication and exchange proteins and nucleic acids between the donor cells and receptor cells (Kourembanas, 2015). Exosomes derived from scratch-wounding cells inhibit wound healing (Zhou et al.,2017). This important subclass of extracellular vesicles, which exhibit diverse intercellular communication biofunctions including antigen presentation, tumor progression and tissue regeneration regulation, have gained much attention in biomedical research (Malda et al., 2016; Lindenbergh and Stoorvogel, 2018; Duan et al., 2020). Cumulated evidence has shown that exosomes derived from MSCs exert beneficial effects on various disease models, including models of myocardial infarction (Zhao et al., 2015; Zhang et al., 2016; Liu et al., 2017; Ma et al., 2018), hepatic fibrosis (Li et al., 2013;Jiang et al., 2018) and even cancer (Reza et al., 2016; Phinney and Pittenger, 2017; Qi et al., 2017; Kim et al., 2018b).
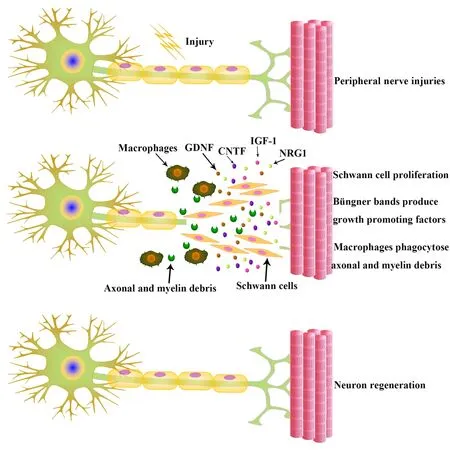
Figure 2 |Neurons regenerate after peripheral nerve injuries.
In the peripheral nerve system, SCs efficiently regulate many functions of axons and ongoing regenerative processes after nerve injury (Willand et al., 2016). Conversely, the regenerative capability in the central nervous system is poor because of glial responses that restrict regeneration and the intrinsic limitations of neurons (Filbin, 2003). After nerve damage, SCs dedifferentiate to a progenitor-like state and increase conduction velocities by myelinating axons as a source of trophic factors to neurons (Lopez-Verrilli et al.,2013). Importantly, the maintenance and development of peripheral nerves are dependent on local signaling between axons and SCs (Nocera and Jacob, 2020). The dedifferentiated SCs proliferate and provide a mechanical substrate and growth factors to regenerate axons. During this process, SCs secreted factors may be involved in processes activated after nerve injury. However, whether these effector molecules are soluble or delivered to axons using vesicular vectors has not been evaluated. Webber et al. (2011) demonstrated that transfer of SC-derived exosomes to axons constitutes a novel mechanism to facilitate the regeneration of nervous system.The clinical use of SC-derived exosomes is also emerging,as in reports that exploit the endogenous pro-regenerative activity of SC-derived exosomes by electroporating exosomesin vitroto load specific siRNAs (Alvarez-Erviti et al., 2011; Guo et al., 2019). These studies have indicated that MSC-derived extracellular vesicles exert functions similar to those of SCs by beneficially promoting peripheral nerve regeneration. It has been indicated that MSC-derived exosomes, as cellular paracrine products, may play a major role in recovery after PNI(Zhang et al., 2015a). Exosomes secreted from MSCs have a protective effect against glutamate-induced neuronal damage that may be mediated through the PI3-Akt signaling pathway(Wei et al., 2016). There is also increasing evidence to suggest that exosome miRNAs are ideal candidates for disease-related biomarkers with various applications in disease management and prevention programs (Bu et al., 2019). Although the exact biological functions of MSC exosomes have not been completely elucidated, it is widely accepted that they play a key role in the amelioration of disease (Huo et al., 2020; Li et al., 2020). Consequently, they are now subject to much research interest.
Neural Conduits of Mesenchymal Stem Cells for Peripheral Nerve Injury Repair
Neural conduit tissue engineering uses a supporting tubular type of scaffold to complement therapeutic technology for an autologous nerve graft and has been widely applied for peripheral nerve regeneration. At its core is the establishment of three-dimensional neural conduits composed of biological materials and seed cells (Kim et al., 2018a). Nerve conduits can prevent the ingrowth of surrounding tissue and reduce the incidence of neuromas (Ma et al., 2017). Although MSCs are transplanted to the stump of nerve injury by local injection to promote nerve repair and have achieved good repair results, some researchers have noticed that uncontrollable infiltration of surrounding tissues seriously affects the reconstruction of normal neural structures and there is a high probability of nerve scars (Cooney et al., 2016). However,nerve conduits loaded with MSCs could both promote nerve growth and regulate the microenvironment of the injured area. Therefore, the emergence of nerve conduit technology may solve the related problems of scarring and penetration by adjacent tissues.
To date, MSCs have been applied to biological tissue engineering through various techniques to improve the regeneration and repair effect after PNI. Adipose-derived MSCs come from a wide range of sources and are one of the most easily available types of MSCs. After Zuk et al. (2001)first reported the method of obtaining adipose-derived MSCs,they became popular among researchers. Adipose-derived MSCs have multi-directional differentiation potential and later studies confirmed that they can differentiate into neuron-like cells and nerve cells. Research on the application of adiposederived MSCs in the repair of PNI has been conducted in various animal models (Mathot et al., 2020; Zhou et al.,2020). Ghoreishian et al. (2013) extracted undifferentiated autologous adipose-derived MSCs from canine adiposetissue to repair canine facial nerve injury. They encapsulated undifferentiated adipose-derived MSCs in alginate hydrogels and successfully repaired a 7-mm nerve defect gap(Ghoreishian et al., 2013). Allbright et al. (2018) also used adipose-derived MSCs loaded in hydrogels for the repair of sciatic nerve defects in rats and showed an effective repair outcome. Sowa et al. (2016) loaded adipose-derived MSCs and SCs into gelatin hydrogel catheters and transplanted them to the sciatic nerve injury of mice. All these results showed that adipose-derived MSCs transplantation can promote axon regeneration, myelin formation and recovery from denervated muscle atrophy, results that are equivalent to the repair effect of Schwann cell transplantation (Sowa et al., 2016). However,the undifferentiated characteristics of adipose-derived MSCs inevitably change after multiple generations of proliferation,and the risk of tumor formationin vivoneeds to be assessed in further studies.
Bone marrow MSCs are mainly derived from bone marrow tissue and have strong differentiation potentials towards osteocytes, cartilage and fat. Studies have shown that bone marrow MSCs can differentiate into neuron-like and gliallike cells in the presence of specific growth factors, which provides a theoretical basis for bone marrow MSCs for nerve injury repair (Guan et al., 2014). Bone marrow MSCs have the advantage that they do not stimulate the significant proliferation of T cells and are not targeted by CD8+T cells(Kim et al., 2018c). Therefore, when applied to autologous or allogeneic transplants, bone marrow MSCs could avoid the killing and elimination of immune cells in the body, thereby playing a repair role in PNIs. A previous study showed bone marrow MSCs in a polyglycolic acid nerve conduit could repair facial nerve defects in rats (Costa et al., 2013). The results demonstrated that bone marrow MSCs can be successfully integrated into the conduits, and survive up to 6 weeks in nerve tissue (Costa et al., 2013). In another study, researchers loaded bone marrow MSCs into a chitosan nerve duct and observed that the cells survived and proliferated within the duct for a period of 8-16 weeks, successfully promoting the repair of 8 mm nerve defects (Zheng and Cui, 2010). In a subsequent study, chitosan nerve conduits loaded with bone marrow MSCs not only accelerated the efficiency of nerve repair but also improved the quantity and quality of regenerated nerve fibers, obtaining a therapeutic effect comparable to autologous nerve transplantation (Zheng and Cui, 2012). Unfortunately, degradation products of nerve conduit materials often cause local immune responses,leaving the injury site in an inflammatory state, which affects the repair effect (Duffy et al., 2019). Thus, Hsu et al. (2013)modified chitosan neural conduits with laminin, which enhanced the adhesion of bone marrow MSCs to the conduits and observed successful inhibition of local inflammatory responses caused by the degradation of chitosan. Umbilical cord MSCs, which are more convenient to obtain compared with bone marrow MSCs and are less likely to be contaminated than adipose-derived MSCs, are highly proliferative cells. Cui et al. (2018) showed that the collagen catheters combined with umbilical cord MSCs promoted regeneration and repair after sciatic nerve transaction. The results demonstrated that collagen catheters could provide mechanical support for neural regeneration and, combined with umbilical cord MSCs,effectively promoted neural regeneration and functional recovery. In summary, MSCs tissue engineered nerve conduits could provide support for MSCs as a substitute for nerve transplantation and prevent the infiltration of tissues from around the injury site to the nerve stump, presenting satisfactory repairs for PNIs.
Application of Genetic Engineering of Mesenchymal Stem Cells in Peripheral Nerve Injury
Gene modification mainly refers to the use of biochemical methods to either modify the DNA sequence or introduce the target gene fragment into the host cell or delete specific gene fragments from the genome to achieve the effect of changing the host cell genotype or strengthening the original genotype(Gupta and Shukla, 2017). Once a modified gene is introduced into a cell, it can over-express a specific gene or constructed gene, and continuously synthesize a specific protein, making it more sensitive to physiological stimuli, including high blood sugar, hormone concentrations, drugs or chemical factors(Liang et al., 2009; Barros and Offenbacher, 2014). Original or genetically modified MSCs have been used in the regeneration of liver, heart muscle, nerves, bones, tendons, and other connective tissues. Normal MSCs have the disadvantages of short survival time and low concentration at the injury site after implantation into the host, whereas genetically modified MSCs can overcome the above defects. By optimizing stem cell and vector selection, effectively introducing specific genes into MSCs and verifying the ability of the modified MSC to express proteins throughin vitroexperiments, the selected modified MSCs can be used in the clinic to treat acquired and hereditary diseases (Wakitani et al., 2007). In the field of neural repair tissue engineering, the main purpose of genetic modification is to design target cells so that they can release growth factors, migration molecules and adhesion molecules in excess and can inhibit the expression of defective genes.
Genetically modified MSCs are widely applied in nervous system research. Kim et al. (2008) demonstrated that transcription factor, neurogenin 1 (Ngn1), can induce MSCs to differentiate into neurons, which present voltage-gated L-type calcium channels and tetrodotoxin-sensitive voltage-gated sodium channels. Transplantation of Ngn1-modified MSCs into the skull of a rat model of stroke was shown to promote contact between neurons and improve conduction function.Human telomerase reverse transcriptase-modified MSCs have be used for functional recovery in rat cerebral ischemia models (Honma et al., 2006; Kim et al., 2008). Modified MSCs can also promote neuronal cell survival and neurogenesis through a type of neuroregulatory molecule brain-derived neurotrophic factor (Ko et al., 2018). Zhang et al. (2015b)employed bone marrow MSCs transfected with brain-derived neurotrophic factor and ciliary neurotrophic factor for the treatment of sciatic nerve injury in rats. These MSCs combined with nerve transplantation improved the sciatic nerve function and increased the thickness of regenerating nerve myelin sheath, which suggests that they effectively promoted the growth of axons and facilitated the repair of PNIs.
Studies have shown that microRNAs play an important role in neural development and the differentiation of stem cells into neural cells. Researchers aim to promote the differentiation of MSCs into nerve cells by manipulating the expression of specific microRNAs. For example, Hu et al. (2017) achieved a good outcome by regulating microRNA-218 of adiposederived MSCs and using it to repair sciatic nerve injury in rats. Furthermore, Wang et al. (2014) illustrated that JMJD1C can maintain microRNA-302 expression through epigenetics,thereby inhibiting neural differentiation of stem cells.Therefore, knocking out JMJD1C can be beneficial to the neural differentiation ability of stem cells.
Genetically modified MSCs have multiple potentials in the treatment of PNIs. Transplanted, appropriately genetically modified MSCs can survive longer in the host environment and secrete specific proteins that are beneficial to the patient’s need. The urgent problem to be solved is how to accurately improve MSCs, translate specific proteins and effectively apply them to treat peripheral nerve system damage.
Conclusion and Perspectives
Although MSCs can differentiate into nerve cells and regulate the microenvironment of the injured area to accelerate the regeneration of peripheral nerves, the mechanism of MSCs differentiation and the ability to secrete neurotransmitters remain to be clarified. A large number of studies have reported the use of MSCs in treatment of neurological disease, such as multiple sclerosis, amyotrophic lateral sclerosis, Alzheimer’s disease and spinal cord injury models (Squillaro et al., 2016).However, fewer clinical trials have utilized MSCs after PNI.MSCs must be cultivatedin vitroto be used clinically because of the limited supply of MSCs in tissues. The cultivationin vitrois performed in an artificial environment, therefore, the cells may be biologically different from freshly extracted MSCs and may cause iatrogenic adverse reactions. In addition, aging is a common feature of all organisms, and stem cells are no exception. Thus, it is important to establish a system to detect the degree and proportion of aging and prevent or delay aging of MSCs. The clinical application of MSCs raises some ethical and safety concerns. In China, we attach great importance to the ethical issues, safety and effectiveness of stem cells in clinical application. However, with the increase of global clinical stem cell research projects and the accumulation of experience, the cost, safety, and effective consequences after transplantation are urgent problems to solve before MSC treatment is applied clinically.
Author contributions:DQG, CR and YBC designed the literature retrieval strategy. RCZ, WQD and JYZ summarized the information. RCZ and WQD wrote the first version of this paper. RCZ and JYZ made the illustrations.JYZ, SXY, FZL and HMD participated in the writing. YBC, CR and DQG reviewed and revised the manuscript. All authors approved the final version of the paper.
Conflicts of interest:The authors declare no conflicts of interest.
Financial support:This work was funded by Clinical Medicine Key Project from the Social Development and Collaborative Innovation Plans in Xuzhou City of China, No. KC14SX016 (to DQG). The funding sources had no role in study conception and design, data analysis or interpretation,paper writing or deciding to submit this paper for publication.
Copyright license agreement:The Copyright License Agreement has been signed by all authors before publication.
Plagiarism check:Checked twice by iThenticate.
Peer review:Externally peer reviewed.
Open access statement:This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix,tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
Open peer reviewer:Michele R Colonna, Universita degli Studi di Messina,Italy.
Additional file:Open peer review report 1.
- 中國神經(jīng)再生研究(英文版)的其它文章
- Mechanisms implicated in the contralateral effect in the central nervous system after unilateral injury: focus on the visual system
- Toward three-dimensional in vitro models to study neurovascular unit functions in health and disease
- Apolipoprotein A1, the neglected relative of Apolipoprotein E and its potential role in Alzheimer’s disease
- Oral frailty and neurodegeneration in Alzheimer’s disease
- Non-coding RNAs and other determinants of neuroinflammation and endothelial dysfunction:regulation of gene expression in the acute phase of ischemic stroke and possible therapeutic applications
- Altered microRNA expression in animal models of Huntington’s disease and potential therapeutic strategies

