Increased risk of colorectal neoplasia in inflammatory bowel disease patients with post-inflammatory polyps:A systematic review and meta-analysis
INTRODUCTION
Post-inflammatory polyps (PIPs),commonly known as pseudopolyps in the past,are islets of mucosa that develop after severe ulceration and disruption of mucosal integrity in the setting of chronic inflammation,such as inflammatory bowel disease(IBD)[1-3].PIPs can be classified into four pathologic types:(1) Ragged mucosal remnant;(2) Granulation tissue polyps;(3) Mixed polyps;and (4) “hyperplasticadenomatous” polyps[1,4-6].Whether different types of PIPs lead to the same risk of colorectal neoplasia (CRN) in IBD patients awaits further study.The prevalence of PIPs in IBD patients was reported to range from 10% to 40%[7-24].This discrepancy may be due to the differences in diagnostic criteria,study year,and study population.PIPs are found more often in ulcerative colitis (UC) than in Crohn’s disease (CD)[25],and can be even 2-fold more in some studies[6,13].In addition,the incidence can increase with the extent and duration of colitis[9,10,16,26].
Colorectal cancer (CRC) is a serious complication in long-standing IBD and significantly increases the mortality rate due to this disease.Guidelines for Colorectal Cancer Screening and Surveillance in Moderate and High-Risk Groups (update from 2002)[27] recommend surveillance intervals among IBD patients according to risk stratification.Several risk factors such as duration and severity of disease,young age at IBD diagnosis,family history of CRC,whether accompanied by primary sclerosing cholangitis and stricture,categorize IBD patients into low-,medium-,and high-risk groups.Patients with PIPs are included in the medium-risk group and colonoscopy is recommended every three years.Similarly,the AGA technical review on the diagnosis and management of CRN in IBD[28] recommend that patients with multiple inflammatory pseudopolyps should undergo more frequent colonoscopy surveillance.
Both guidelines recommend the presence of PIPs as a risk factor for CRC in IBD patients.However,the literature cited in the guidelines comes from small case-control studies,indicating an insufficient level of evidence[14,29].In addition,different opinions have been raised in some recent high-quality literature[30-32].To comprehensively assess the impact of the presence of PIPs,we aimed to conduct a metaanalysis to quantify the impact of co-existing PIPs on the risk of CRN in IBD patients.We hypothesized that IBD patients with PIPs had an increased risk of CRN.
A cry came up in answer, O servant of God! we have been in the well a long time; in God s name get us out! After trying a thousand schemes, I drew up two blind women
MATERIALS AND METHODS
Our study followed PICOS principles and was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)statement[33].
Search strategy
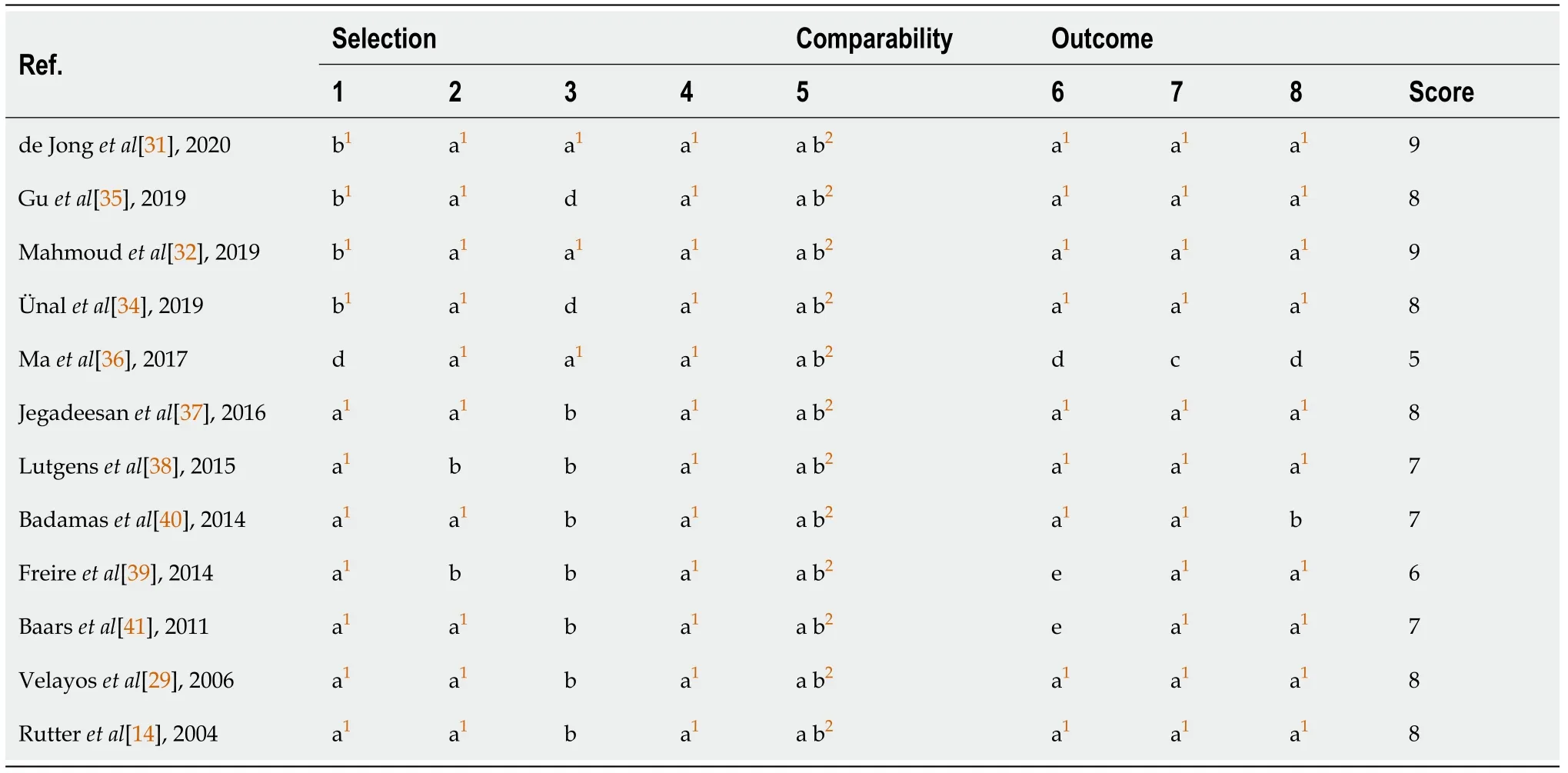
The quality of each study was evaluated separately using the NOS.The results showed that the scores of the studies ranged from 5 to 9 points,and most scored 7 or above[14,29,31,32,34,35,37,38,40,41].Table 2 shows the NOS results for the included studies.
It is interesting to note that most included studies from the last two years[31,32,34]had a contrary conclusion to previous studies[14,29,41],although the quality of relevant studies was relatively high.Recent studies reported that no independent association between PIPs and CRN was found[30-32,34],which was contrary to our findings.This may be explained by the differences in the included study population and changes in the treatment patterns of IBD patients in recent years[57-60].On the one hand,PIPs are the complication of prior extensive colon inflammation,leading to colectomy,and higher rates of early colectomy may result in a lower risk of CRN in these patients.On the other hand,with the widespread application of biological agents(such as infliximab,mesalazine,azathioprine,
.) in the treatment of IBD,the risk of CRN in IBD patients may decline.Recent studies might have included more bettertreated IBD patients,leading to a lower risk of CRN in their study population.However,our study included 5819 IBD patients since 1976,indicating that our results may be less influenced by these factors.
Study selection
According to the inclusion and exclusion criteria,two investigators (He DG and Chen XJ) independently reviewed all the searched literature and resolved any discrepancies through discussion to reach a consensus.Studies meeting the following criteria were included:(1) A comparison of IBD patients with and without PIPs,with CRN as the endpoint;(2) A detailed number of IBD patients with and without PIPs,as well as the number of CRN cases among these patients;and (3) For republished studies,we included the most recent publications.
Studies were excluded if (1) They were review articles,case reports,letters,or laboratory studies;(2) Important data of interest were missing;(3) Republished literature;and (4) Not English literature.Twelve eligible studies were finally included in our meta-analysis[14,29,31,32,34-41].
The reasons and theories behind three s popularity are numerous and diverse. The number has been considered powerful across history in different cultures and religions, but not all of them. Christians have the Trinity, the Chinese have the Great Triad (man, heaven, earth), and the Buddhists have the Triple Jewel (Buddha, Dharma, Sanga). The Greeks had the Three Fates. Pythagoras considered three to be the perfect number because it represented everything: the beginning, middle, and end. Some cultures have different powerful numbers, often favoring seven, four and twelve.Return to place in story.
The purchase of the card each week is not done out of habit. It is my romantic mission each week to find the right card. At times, my search takes me to many different card stores to find that perfect offering. I have been known to spend a considerable amount of time in front of the card displays, reading up to a dozen different cards before I choose the right one. The picture and the words in the card must have specific meaning to me and must remind me in some way of Patricia and our life together. The card needs to evoke6 an emotion in me. I know that if a card brings a tear of happiness to my eyes, I have found the right one.
Data extraction
Raw data included in the study were extracted by two researchers (He DG and Huang JN) according to our pre-designed data extraction form.After discussing the deviations in detail with the senior investigator (He XS),we agreed on each study.The information extracted from the article were:study author,published year,published journal,study design,study type,surveillance period,sources of patients,race,age at IBD diagnosis,IBD type,quantitative data on the number of IBD patients,and the number IBD patients with concomitant PIPs,male gender and the presence of neoplasia or cancer.
Outcome measures
The primary outcome of the current study was whether PIPs increased the risk of CRN(including dysplasia and cancer) in IBD patients.The secondary outcome was whether PIPs increased the risk of CRC in IBD patients.
Methodological quality assessment of the included studies
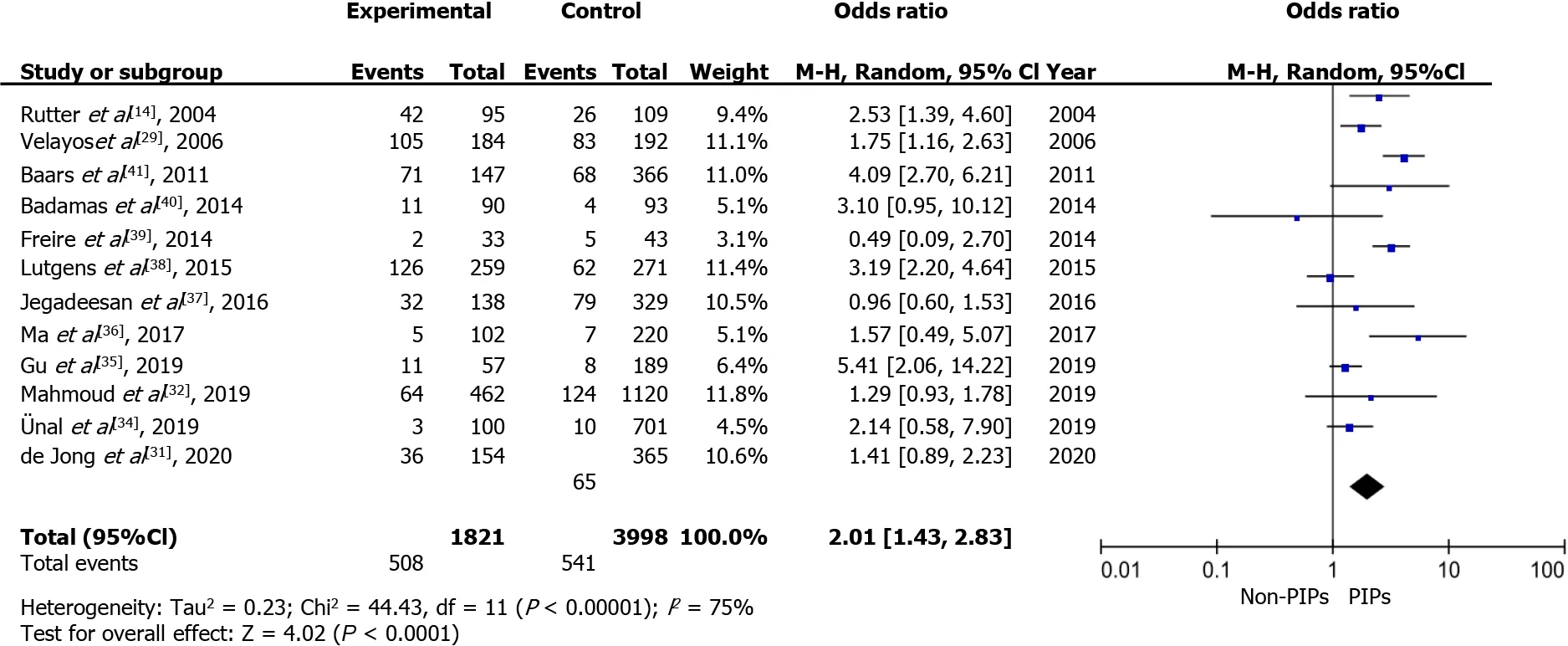
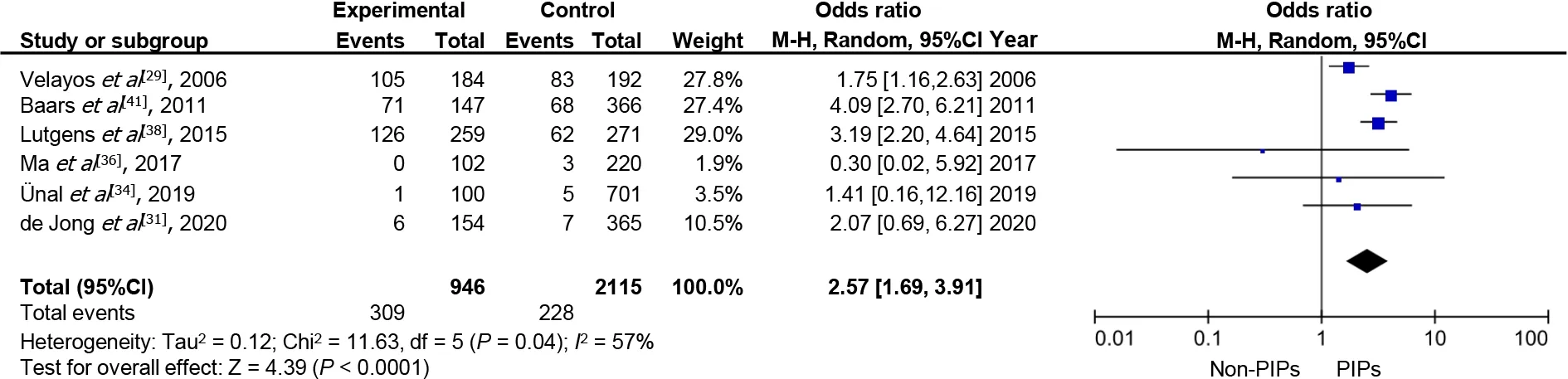
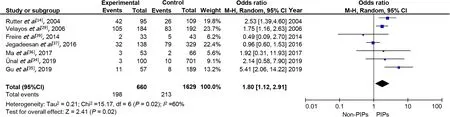
PIPs were associated with a higher risk of CRN in IBD patients (OR 2.01;95%CI:1.43–2.83) (Figure 2).When CRC was used as an endpoint,patients with PIPs had an approximately 2.5-fold increased risk compared to those without PIPs (OR 2.57;95%CI:1.69–3.91) (Figure 3).When UC patients were analyzed separately,the pooled OR was 1.80 (95%CI:1.12–2.97),suggesting that the existence of PIPs was related to a higher risk of CRN in UC patients (Figure 4).Limited data prevented us from performing a meta-analysis in CD patients,but the study by Ma
[36] indicated that no association was observed between PIPs and CRN in these patients (OR 1.27;95%CI:0.24–6.75).However,there was high heterogeneity among studies (
2=75%);therefore,the Mantel-Haenszel random-effects model was used to test the results.Furthermore,the sources of heterogeneity were assessed by subgroup analyses,sensitivity analysis,and assessment of publication bias.
Statistical analysis
The primary data extracted from the included studies were dichotomous variables.The pooled odds ratio (OR) and 95% confidence interval (CI) were used to represent the pooled effect size.Study heterogeneity was assessed by the Q test and the I
statistic (which could quantify the level of heterogeneity).An
2 value more than 50%or
value less than 0.10 in the Q-test represented substantial heterogeneity.When study heterogeneity was present (
>50% or
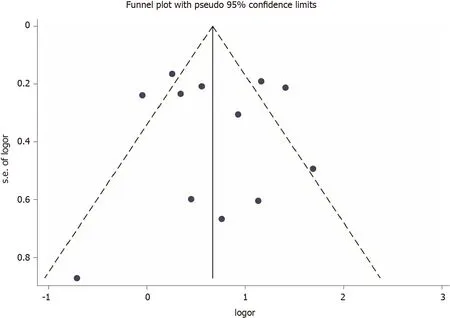
<0.10),the random-effects model was used to assess the pooled effect,otherwise,the fixed-effects model was used.Subgroup analysis was performed as stratified based on IBD subtype and study type.Publication bias in the included studies was assessed by funnel plots.If potential biases were detected,we performed further sensitivity analyses to assess the robustness of pooled effect estimates and the likely impact of biases.We also performed a sensitivity analysis to investigate the impact of each study on the overall risk estimate by omitting one study in turn.A two-sided
value less than 0.05 was considered statistically significant.All the statistics were analyzed by Review Manager 5.4 (Cochrane Collaboration,Oxford,UK) and STATA 15.1 (StataCorp,College Station,Texas,USA).The statistical methods used in this study were reviewed by Ping Lan from the Department of Colorectal Surgery,the Sixth Affiliated Hospital,Sun Yat-sen University.
RESULTS
Study selection
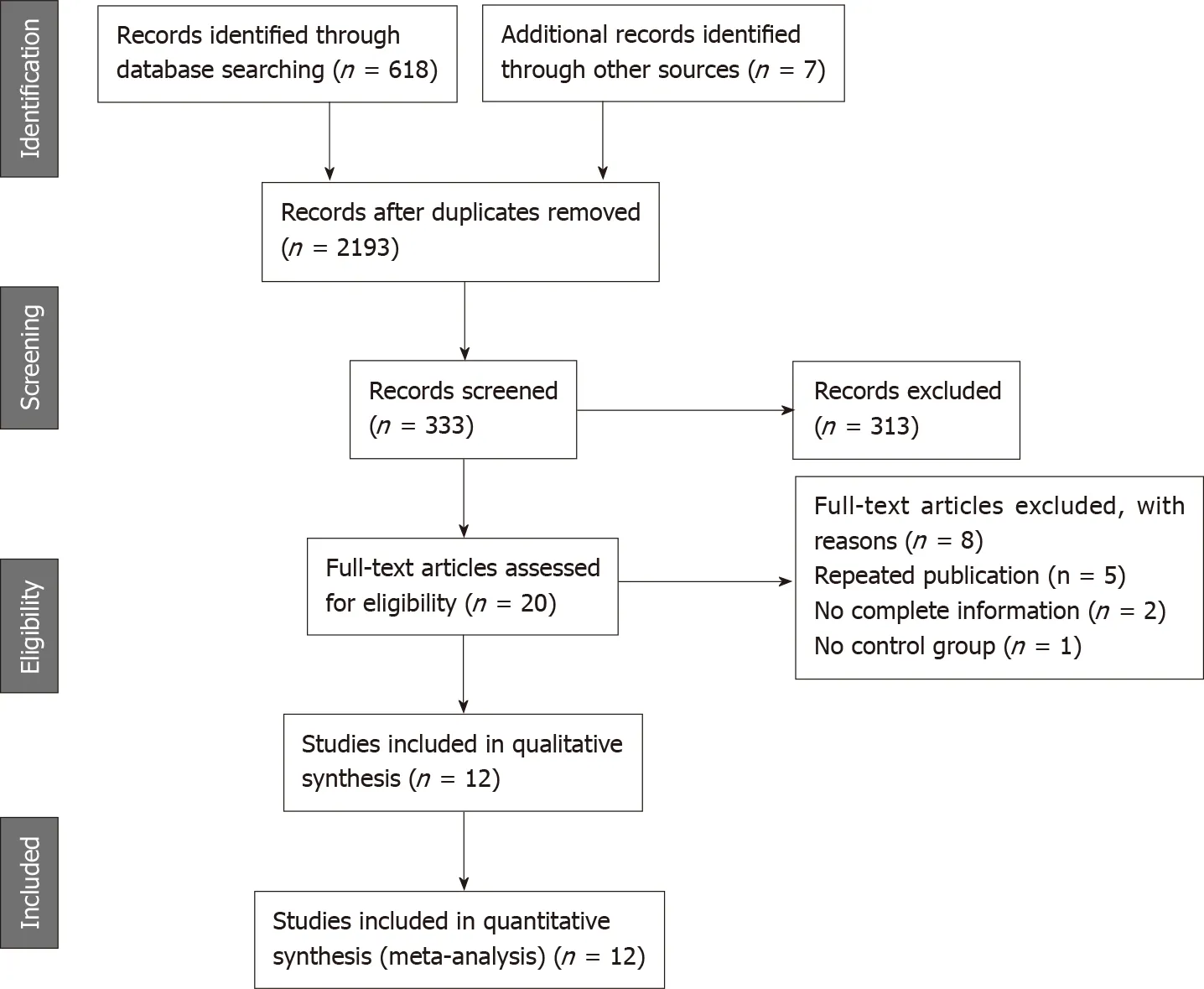
In the initial search,a total of 618 related articles were obtained according to the research strategy.We also obtained 7 articles from the reference lists and citation indices of the included studies[29,31,34,38,41,43,44].Twenty articles[14,29-32,34-41,45-51] that might be eligible for inclusion were reviewed.Among them,12 articles met our inclusion criteria (Figure 1)[14,29,31,32,34-41].Five studies were excluded due to duplication[45-49],2 studies due to incomplete data of interest[30,50],and one due to lack of a control group[51].
9.Nothing but the cat: A cat would be useful to the miller for keeping rodents out of the mill. However, a cat would be of small or negligible value and easily replaced in the mill, unlike the ass and the mill itself. The youngest son, as last in line, has surely received the poorest inheritance.Return to place in story.
Study characteristics
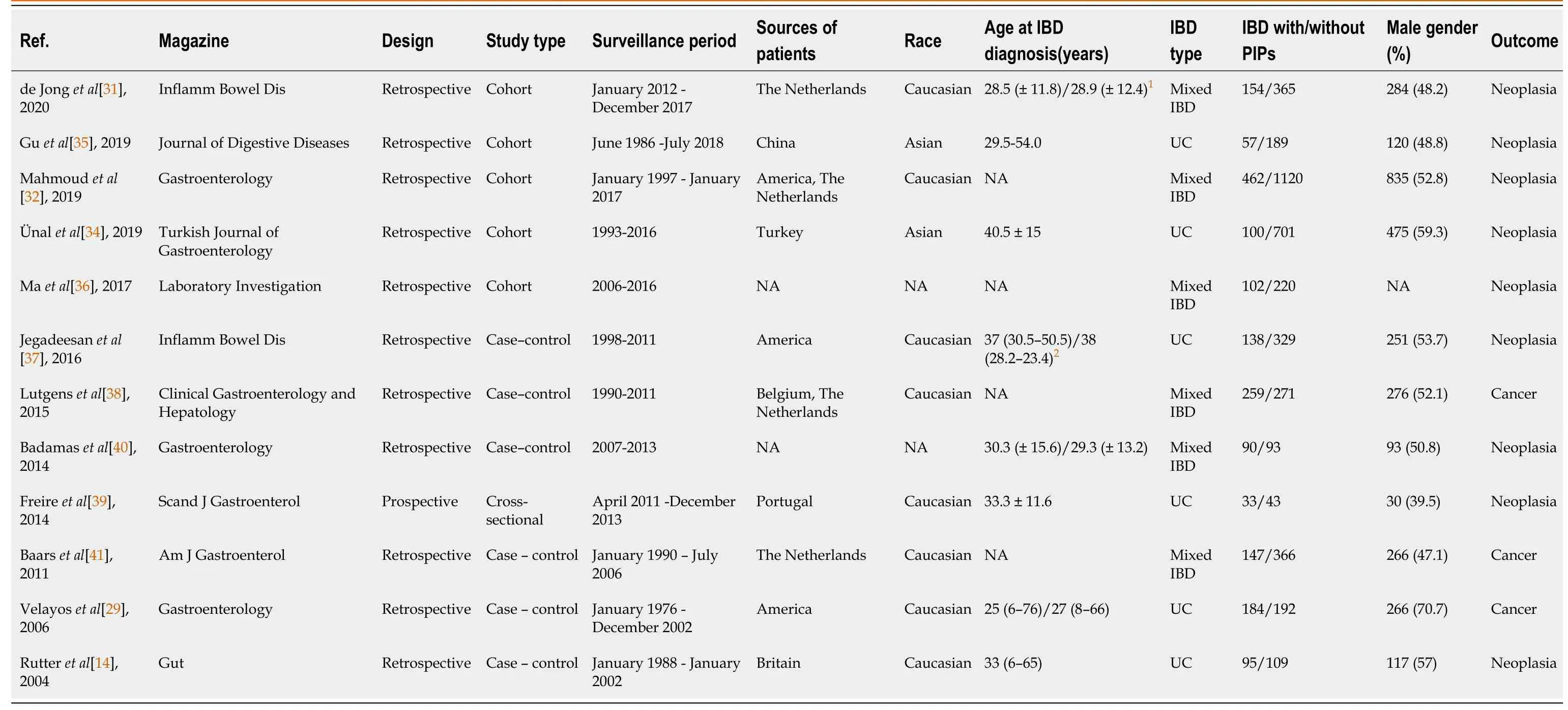
The baseline characteristics of the included studies are described in Table 1.Overall,the 12 included studies were published between 2004 and 2020.A total of 5819 IBD patients,including 1821 (22.01%) IBD patients who also had PIPs,were identified.Of these studies,5 studies were cohort studies[31,32,34-36],6 were case-control studies[14,29,37,38,40,41] and one was a cross-sectional study[39].One was a prospective study[39] and the others were retrospective studies[14,29,31,32,34-38,40,41].In addition,7 studies contained data that could be used to independently analyze UC patients[14,29,34-37,39],one study contained data that could be used to independently analyze CD patients[36],and in 5 studies we were unable to distinguish the data between UC patients and CD patients[31,32,38,40,41].In addition,all studies included raw data with the endpoint as CRN,and 6 studies reported on the number of IBD patients who developed CRC[29,31,34,36,38,41].
So she shall, cried the king, who overheard these words; she shall die my queen, for she is more beautiful than all the ladies of the court, and I will marry no one else
Quality assessment of the included studies
A systematic literature search strategy was designed to determine all published or unpublished studies comparing the risk of CRN in IBD patients with and without PIPs.A comprehensive literature search of the following databases was conducted:PubMed,Embase,Cochrane Library,and Web of Science (English literature only,each from inception to October 22,2020).We used medical subject headings and all free texts to retrieve the following keywords:‘ulcerative colitis’,‘crohn’s disease’,‘inflammatory bowel disease’,‘post-inflammatory polyps’,‘colorectal neoplasms’,‘colonic neoplasms’,‘rectal neoplasms’ and ‘dysplasia’.All searches were performed separately by two researchers strictly following our pre-designed search strategy.After consulting with the senior investigators (He XS and Lan P) regarding queries,we reached an agreement for the retrieval results.Also,citations from each article on the topic were manually searched for other potentially eligible studies.
Quantitative summary (meta-analysis)
The quality of the included studies was assessed using the Newcastle-Ottawa Scale(NOS),designed specifically for non-randomized studies in meta-analysis[42].The included studies were evaluated based on population selection (4 options),comparability (2 options),outcome of interest (cohort study) or determination of exposure(case-control study) (3 options).One point was assigned for each option,for a total of 9 points (Supplementary Table 1).A high-quality study required a score of 7 or above.
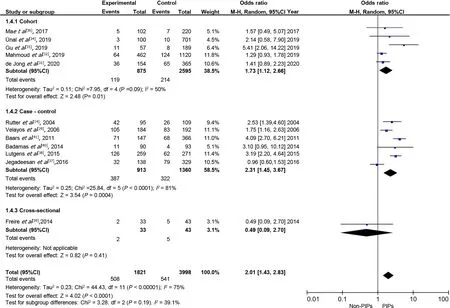
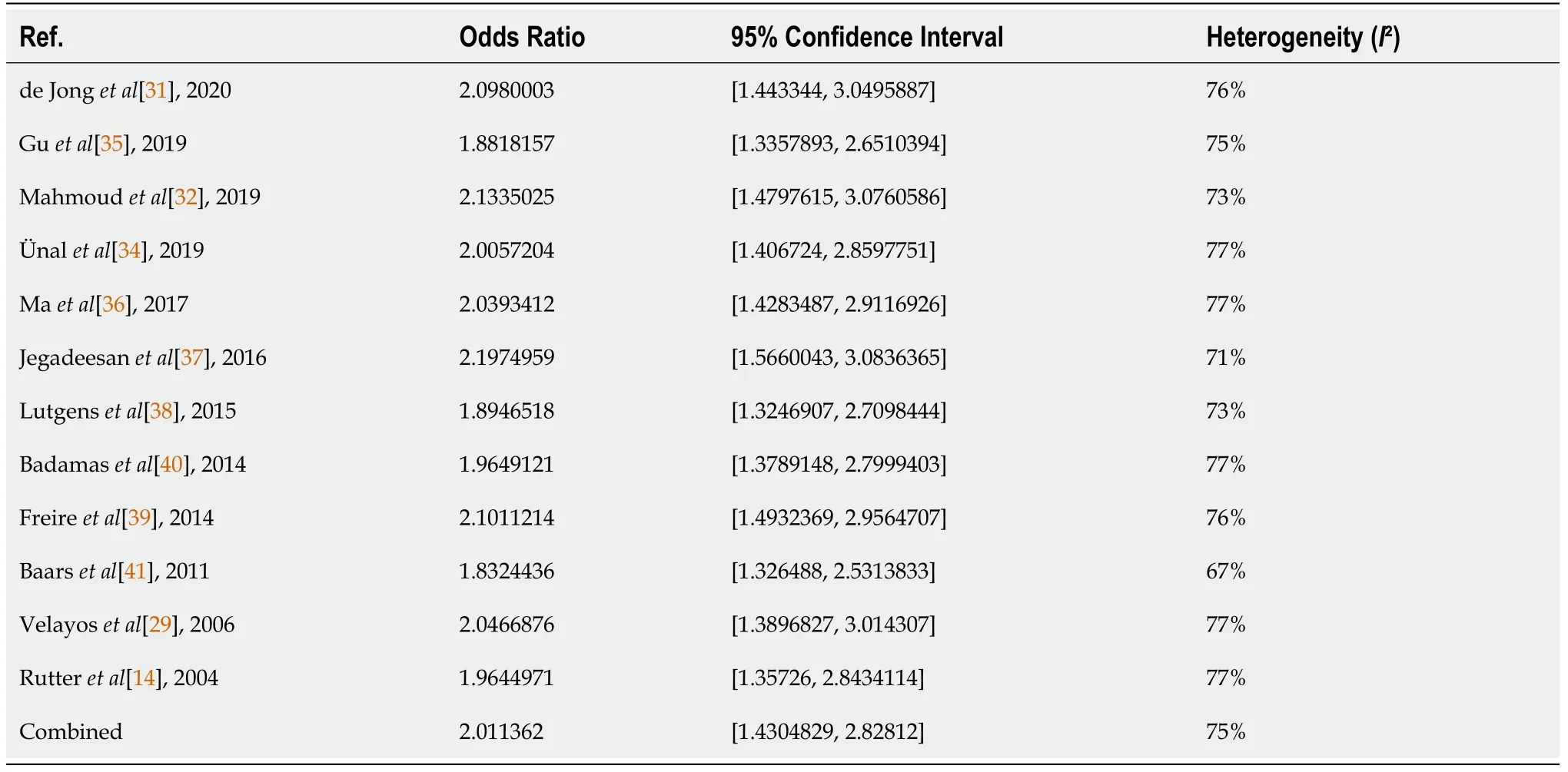
Subgroup analysis
High heterogeneity was found in our study.When subgroup analysis was conducted according to different study types (Figure 5),heterogeneity decreased to an acceptable level.In addition,sensitivity analysis and assessment of publication bias were performed to determine the sources of heterogeneity.We reanalyzed the included studies after excluding two studies with a score below 7[36,39];however,the results were similar to those before the exclusion of these studies (OR 2.14;95%CI:1.50–3.06;
2=78%).Also,when we excluded one of the included studies in turn,there were no significant changes in the results of the pooled effect size (Table 3) and heterogeneity.Furthermore,as shown in the funnel plot (Figure 6),there was no significant publication bias in our included studies.In general,we found that study type may be one of the sources of heterogeneity,and other potential heterogeneity may arise due to internal factors (such as IBD type,study population,statistical methods) within each included study.
Sensitivity analysis
Several limitations of our study should be considered.Firstly,heterogeneity was pronounced in our study,which may be related to the study types.Secondly,the studies included did not have standardized reports on PIPs.The reports on PIPs were mainly from endoscopy reports by endoscopists,which may have resulted in misclassification of PIPs.However,the reports on PIPs by a qualified endoscopist were usually reliable,and the relevant pathology reports confirmed the findings.Thirdly,some confounding factors,such as the degree of colitis at the time of the colonoscopy,duration of colitis,and endoscopy interval were not well controlled in the included studies,which prevented us from analyzing their impact on the results.Therefore,controlling these confounding factors and performing higher quality studies is the direction of our efforts in the future.Despite these limitations,to the best of our knowledge,this is currently the most comprehensive and high-quality meta-analysis with the largest population investigating the risk of CRN in IBD patients with PIPs.
Assessment of publication bias
A funnel plot with 12 studies was used to evaluate publication bias (Figure 6).It can be seen that the scatter point distribution was basically symmetrical,indicating no significant publication bias in the current meta-analysis.
March 12, 2007 issue - A few years ago, just as her father was about to disappear into the fog of dementia(), journalist Lucinda Franks stumbled upon a small box in a corner of his dilapidated() apartment. The contents shocked her. Beneath some mysterious maps and crumpled1 foreign bank notes, she found a military cap embellished2 with the raised metal insignia(,) of an eagle, a skull3 and crossbones—and a swastika. Franks knew little about her father s military service during World War II, and had always sensed that he was hiding something. Now questions consumed her. Was my sphinx-like father presenting one character and living another? she writes in her new memoir4, My Father s Secret War. Whose side was he really on? When she pressed for an explanation, her father refused to talk, citing a decades-old pledge of secrecy5.
But one day the Princess, wandering sadly by the river, spied Prince Featherhead fast asleep in the shade of a tree, and stole nearer to enjoy the delight of gazing at his dear face unobserved
DISCUSSION
Currently,the leading guidelines from Europe and the United States recommend more frequent colonoscopy for IBD patients with PIPs,in order to detect CRN in a timely manner[27,28].However,several high-quality studies have recently shown that the presence of PIPs is not an independent risk factor for CRN in IBD patients[30-32].The current meta-analysis of 12 observational studies including 1821 (22.01%) patients with PIPs indicated that IBD patients with PIPs had an approximately 2-fold increased risk of CRN.It is worth mentioning that we included two abstracts[36,40] with required data in our analysis,which may have introduced bias.However,even when we excluded these abstracts,we came to the same conclusion (OR 1.99;95%CI:1.37-2.88).Even when excluding dysplasia,the risk of CRC was still increased by approximately 2.5-fold in IBD patients with PIPs as compared with those without PIPs.In addition,UC patients with PIPs had an approximately 1.8-fold increased risk of CRN as compared with those without PIPs.Limited data on the risk of CRN in CD patients with PIPs may be related to the low incidence of PIPs among CD patients.
The reasons and mechanisms for the increased risk of CRN in IBD patients with concomitant PIPs remain unclear.One possible reason for this association is that PIPs are thought to be markers of previous episodes of severe inflammation.The incidence of PIPs increases with the severity of colitis,which may accelerate the development of CRN[9,32,52].Another possible reason is that multiple PIPs may weaken the ability of endoscopy to detect dysplastic lesions[29,31].However,both of these reasons only indicate that PIPs are indirect signs of increased risk of CRN in IBD patients.At present,it is generally believed that PIPs are benign and do not directly cause malignant transformation,even though there have been occasional reports of malignant transformation of PIPs[53,54].However,Jawad
[55] reported that PIPs may be the source of precancerous mutations following the analysis of DNA extracted from 30 different PIPs samples in which 4 identifiable mutations were found.In addition,Lozyns'ka[56] found 21.4% chromosomal anomalies in PIPs samples from IBD patients.Taken together,these findings suggest that we may have to re-think whether PIPs can directly lead to malignant transformation and the therapeutic strategy for PIPs may change in the future.
3. Hansel: In the original manuscript of the story, the brother was referred to as Little Brother. The Grimms chose the name Hansel for the character and included it in the first edition of their tales. Hansel is a common name used for a male character in German folktales. Hansel is essentially53 the same as John Doe representing an anonymous54 or everyman character.Return to place in story.
Our findings may have implications for clinical practice as they might provide an individual reference for endoscopic surveillance strategies in IBD patients.The evidence cited in the current guidelines is inadequate.Our study,which included 5,819 IBD patients from 12 studies,confirms the viewpoint of the guidelines for more aggressive colonoscopy in IBD patients with PIPs and further improves the degree of evidence.Above all,we agree that executing an evidence-based risk stratification model to determine surveillance intervals is cost-effective and in line with the concept of individualized treatment.In addition,it is necessary to identify the time period of higher incidence of CRN in IBD patients with PIPs.In this time period,patients with PIPs will receive more frequent endoscopic surveillance to detect CRN early.Finally,PIPs may weaken the endoscopic recognition of dysplasia.Improving endoscopic techniques to recognize PIPs and dysplasia may further reduce the incidence of CRN in IBD patients with PIPs.Perhaps these proposals could be considered in the IBD surveillance guidelines in the future.
Subgroup analysis based on study types (cohort,case-control,cross-sectional) showed a significant reduction in heterogeneity (Figure 5).In other words,different study types may be a source of heterogeneity.An increased risk of CRN was found in cohort studies (OR 1.73;95%CI:1.12–2.66)[31,32,34-36] and case-control studies (OR 2.31;95%CI:1.45–3.67)[14,29,37,38,40,41].Nevertheless,no association between PIPs and CRN was found in cross-sectional studies (OR 0.49;95%CI:0.09–2.70)[39].
Sensitivity analysis was performed with the pooled OR and 95%CI.The results were essentially unchanged in the statistical outcomes of all the indicators after excluding any one study.The results are shown in Table 3.
CONCLUSION
In summary,IBD patients with PIPs have a higher risk of CRN than those without PIPs.Our best evidence-based study advocates the current guideline that IBD patients with PIPs require more intensive surveillance.
ARTICLE HIGHLIGHTS
Research background
Inflammatory bowel disease (IBD) patients with post-inflammatory polyps (PIPs) may carry an increased risk of colorectal neoplasia (CRN).Current guidelines recommend more aggressive colonoscopy follow-up in these patients.However,the guidelines are based on a low degree of evidence and several recent high-quality studies have shown that the presence of PIPs is not an independent risk factor for CRN in IBD patients.
Research motivation
Whether the risk of CRN in IBD patients with PIPs is increased will have a significant impact on the surveillance strategies of IBD patients.
Research objectives
The current study aimed to evaluate the risk of CRN in IBD patients with and without PIPs.
Research methods
A systematic literature search was performed to identify studies that compared the risk of CRN in IBD patients with and without PIPs.Pooled odds ratio (OR) was calculated using the random-effects model to explore the final pooled effect size of the included studies and determine whether PIPs increase the risk of CRN.Sensitivity analysis,subgroup analysis,and assessment of publication bias were performed to determine the sources of heterogeneity.
18. A great deal of money, and they betrayed the secret to her: Money often brings about corruption. Bribery, especially with money, is found often in literature, even some fairy tales. One of the most famous betrayals in history is Judas Iscariot s betrayal of Christ for 30 pieces of silver in the New Testament.Return to place in story.
Research results
We found that IBD patients with PIPs had an approximately 2-fold increased risk of CRN [OR 2.01;95% confidence interval (CI):1.43–2.83].The results were similar when colorectal cancer was used as the study endpoint (OR 2.57;95%CI:1.69–3.91).
Research conclusions
IBD patients with PIPs have a higher risk of CRN than those without PIPs,which support current guidelines that IBD patients with PIPs require more frequent surveillance.
Research perspectives
Our findings not only confirm the viewpoint of the guidelines,but may also improve the degree of evidence.We expect that our study can provide a reference for the development of surveillance strategies for IBD patients.
1 Politis DS,Katsanos KH,Tsianos EV,Christodoulou DK.Pseudopolyps in inflammatory bowel diseases:Have we learned enough?
2017;23:1541-1551 [PMID:28321155 DOI:10.3748/wjg.v23.i9.1541]
2 Gallart-Esquerdo A.[Anatomicopathological study of rectocolic inflammatory pseudo-polyposis following mucohemorrhagic rectocolitis (grave ulcerative colitis)].
1958;10:1-4 [PMID:13568179]
3 Goldgraber MB.Pseudopolyps in ulcerative colitis.
1965;8:355-363 [PMID:5830658 DOI:10.1007/bf02627260]
4 Munyer TP,Montgomery CK,Thoeni RF,Goldberg HI,Margulis AR.Postinflammatory polyposis(PIP) of the colon:the radiologic-pathologic spectrum.
1982;145:607-614 [PMID:7146388 DOI:10.1148/radiology.145.3.7146388]
5 Lumb G.Pathology of ulcerative colitis.
1961;40:290-298 [PMID:13764247]
6 Kelly JK,Gabos S.The pathogenesis of inflammatory polyps.
1987;30:251-254[PMID:3829873 DOI:10.1007/bf02556166]
7 Schneider R,Dickersin GR,Patterson JF.Localized giant pseudopolyposis.A complication of granulomatous colitis.
1973;18:265-270 [PMID:4695612 DOI:10.1007/bf01070986]
8 Baars JE,Nuij VJ,Oldenburg B,Kuipers EJ,van der Woude CJ.Majority of patients with inflammatory bowel disease in clinical remission have mucosal inflammation.
2012;18:1634-1640 [PMID:22069022 DOI:10.1002/ibd.21925]
9 De Dombal FT,Watts JM,Watkinson G,Goligher JC.Local complications of ulcerative colitis:stricture,pseudopolyposis,and carcinoma of colon and rectum.
1966;1:1442-1447 [PMID:5933046 DOI:10.1136/bmj.1.5501.1442]
10 Jalan KN,Walker RJ,Sircus W,McManus JP,Prescott RJ,Card WI.Pseudopolyposis in ulcerative colitis.
1969;2:555-559 [PMID:4185531 DOI:10.1016/s0140-6736(69)90260-8]
11 Chuttani HK,Nigam SP,Sama SK,Dhanda PC,Gupta PS.Ulcerative colitis in the tropics.
1967;4:204-207 [PMID:6053989 DOI:10.1136/bmj.4.5573.204]
12 Geboes K,Vantrappen G.The value of colonoscopy in the diagnosis of Crohn's disease.
1975;22:18-23 [PMID:1205096 DOI:10.1016/s0016-5107(75)73675-1]
13 Margulis AR,Goldberg HI,Lawson TL,Montgomery CK,Rambo ON,Noonan CD,Amberg JR.The overlapping spectrum of ulcerative and granulomatous colitis:a roentgenographic-pathologic study.
1971;113:325-334 [PMID:5098634 DOI:10.2214/ajr.113.2.325]
14 Rutter MD,Saunders BP,Wilkinson KH,Rumbles S,Schofield G,Kamm MA,Williams CB,Price AB,Talbot IC,Forbes A.Cancer surveillance in longstanding ulcerative colitis:endoscopic appearances help predict cancer risk.
2004;53:1813-1816 [PMID:15542520 DOI:10.1136/gut.2003.038505]
15 Ray G.Inflammatory bowel disease in India--changing paradigms.
2011;26:635-644 [PMID:21063715 DOI:10.1007/s00384-010-1084-5]
16 Teague RH,Read AE.Polyposis in ulcerative colitis.
1975;16:792-795 [PMID:1205273 DOI:10.1136/gut.16.10.792]
17 Reinglas J,Gonczi L,Kurt Z,Bessissow T,Lakatos PL.Positioning of old and new biologicals and small molecules in the treatment of inflammatory bowel diseases.
2018;24:3567-3582 [PMID:30166855 DOI:10.3748/wjg.v24.i32.3567]
18 Teh LB,Koh D,Ng HS,Kwok KC,Lim TC,Ho MS,Seah CS.Ulcerative colitis in Singapore:a clinical study of sixty-one patients.
1987;16:474-479 [PMID:2893576]
19 Wright V,Watkinson G.The arthritis of ulcerative colitis.
1965;2:670-675 [PMID:14337733 DOI:10.1136/bmj.2.5463.670]
20 Wang Y,Ouyang Q;APDW 2004 Chinese IBD working group.Ulcerative colitis in China:retrospective analysis of 3100 hospitalized patients.
2007;22:1450-1455[PMID:17716349 DOI:10.1111/j.1440-1746.2007.04873.x]
21 Baars JE,Kuipers EJ,van Haastert M,Nicola? JJ,Poen AC,van der Woude CJ.Age at diagnosis of inflammatory bowel disease influences early development of colorectal cancer in inflammatory bowel disease patients:a nationwide,long-term survey.
2012;47:1308-1322 [PMID:22627504 DOI:10.1007/s00535-012-0603-2]
22 Chang DK,Kim JJ,Choi H,Eun CS,Han DS,Byeon JS,Kim JO.Double balloon endoscopy in small intestinal Crohn's disease and other inflammatory diseases such as cryptogenic multifocal ulcerous stenosing enteritis (CMUSE).
2007;66:S96-S98 [PMID:17709044 DOI:10.1016/j.gie.2007.01.016]
23 Luo YY,Chen J.[Clinical and colonoscopic characteristics of pediatric inflammatory bowel disease].
2009;47:129-133 [PMID:19573460]
24 Kosugi I,Tada T,Tsutsui Y,Sato Y,Mitsui T,Itazu I.Giant inflammatory polyposis of the descending colon associated with a Crohn's disease-like colitis.
2002;52:318-321 [PMID:12031089 DOI:10.1046/j.1440-1827.2002.01348.x]
25 Buck JL,Dachman AH,Sobin LH.Polypoid and pseudopolypoid manifestations of inflammatory bowel disease.
1991;11:293-304 [PMID:2028064 DOI:10.1148/radiographics.11.2.2028064]
26 Bacon HE,Carroll PT,Cates BA,Mcgregor RA,Ouyang LM,Villalba G.Non-specific ulcerative colitis,with reference to mortality,morbidity,complications and long-term survivals following colectomy.
1956;92:688-695 [PMID:13372871 DOI:10.1016/s0002-9610(56)80140-2]
27 Cairns SR,Scholefield JH,Steele RJ,Dunlop MG,Thomas HJ,Evans GD,Eaden JA,Rutter MD,Atkin WP,Saunders BP,Lucassen A,Jenkins P,Fairclough PD,Woodhouse CR;British Society of Gastroenterology;Association of Coloproctology for Great Britain and Ireland.Guidelines for colorectal cancer screening and surveillance in moderate and high risk groups (update from 2002).
2010;59:666-689 [PMID:20427401 DOI:10.1136/gut.2009.179804]
28 Farraye FA,Odze RD,Eaden J,Itzkowitz SH.AGA technical review on the diagnosis and management of colorectal neoplasia in inflammatory bowel disease.
2010;138:746-774 [PMID:20141809 DOI:10.1053/j.gastro.2009.12.035]
29 Velayos FS,Loftus EV Jr,Jess T,Harmsen WS,Bida J,Zinsmeister AR,Tremaine WJ,Sandborn WJ.Predictive and protective factors associated with colorectal cancer in ulcerative colitis:A casecontrol study.
2006;130:1941-1949 [PMID:16762617 DOI:10.1053/j.gastro.2006.03.028]
30 Al Bakir I,Curtius K,Kabir M,Saunders B,Suzuki N,Thomas-Gibson S,Wilson A,Moorghen M,Graham T,Hart A.Long-term outcomes following endoscopic resection of neoplastic lesions in ulcerative colitis:A large single-centre retrospective study.
2019;7:80 [DOI:10.1177/205064061985467]
31 de Jong ME,Gillis VELM,Derikx LAAP,Hoentjen F.No Increased Risk of Colorectal Neoplasia in Patients With Inflammatory Bowel Disease and Postinflammatory Polyps.
2020;26:1383-1389 [PMID:31677385 DOI:10.1093/ibd/izz261]
32 Mahmoud R,Shah SC,Ten Hove JR,Torres J,Mooiweer E,Castaneda D,Glass J,Elman J,Kumar A,Axelrad J,Ullman T,Colombel JF,Oldenburg B,Itzkowitz SH;Dutch Initiative on Crohn and Colitis.No Association Between Pseudopolyps and Colorectal Neoplasia in Patients With Inflammatory Bowel Diseases.
2019;156:1333-1344.e3 [PMID:30529584 DOI:10.1053/j.gastro.2018.11.067]
33 Shamseer L,Moher D,Clarke M,Ghersi D,Liberati A,Petticrew M,Shekelle P,Stewart LA;PRISMA-P Group.Preferred reporting items for systematic review and meta-analysis protocols(PRISMA-P) 2015:elaboration and explanation.
2015;350:g7647 [PMID:25555855 DOI:10.1136/bmj.g7647]
34 ünal NG,?zütemiz ?,Tekin F,Turan ?,Osmano?lu N.Colorectal cancer and dysplasia risk of ulcerative colitis patients in a tertiary referral center in Turkey.
2019;30:139-147 [PMID:30460897 DOI:10.5152/tjg.2018.18221]
35 Gu YB,Xu WM,Guo YG,Zhong J,Du P.Risk factors of colorectal stricture associated with developing high-grade dysplasia or cancer in ulcerative colitis:A multicenter long-term follow-up study.
2019;20:26 [DOI:10.1111/1751-2980.12808]
36 Ma YR,Ko HBM,Zhu H,Harpaz N,Polydorides AD.Gastrointestinal Pathology.
2017;97:157-210 [PMID:28134861 DOI:10.1038/labinvest.2016.168]
37 Jegadeesan R,Navaneethan U,Gutierrez NG,Venkatesh PG,Hammel JP,Sanaka MR,Shen B.Pattern of Inflammation on Surveillance Colonoscopy Does Not Predict Development of Colitisassociated Neoplasia.
2016;22:2221-2228 [PMID:27542134 DOI:10.1097/MIB.0000000000000862]
38 Lutgens M,Vermeire S,Van Oijen M,Vleggaar F,Siersema P,van Assche G,Rutgeerts P,Oldenburg B;Dutch Initiative on Crohn and Colitis.A rule for determining risk of colorectal cancer in patients with inflammatory bowel disease.
2015;13:148-54.e1[PMID:25041864 DOI:10.1016/j.cgh.2014.06.032]
39 Freire P,Figueiredo P,Cardoso R,Manuel Donato M,Ferreira M,Mendes S,Silva MR,Cipriano MA,Ferreira AM,Vasconcelos H,Portela F,Sofia C.Predictive value of rectal aberrant crypt foci for intraepithelial neoplasia in ulcerative colitis-a cross-sectional study.
2014;49:1219-1229 [PMID:25157637 DOI:10.3109/00365521.2014.951390]
40 Badamas J,Limketkai BN,Lazarev M.Risk of dysplasia according to severity of pseudopolyposis in inflammatory bowel disease.
2014;146:S-436 [DOI:10.1016/S0016-5085(14)61568-7]
41 Baars JE,Looman CW,Steyerberg EW,Beukers R,Tan AC,Weusten BL,Kuipers EJ,van der Woude CJ.The risk of inflammatory bowel disease-related colorectal carcinoma is limited:results from a nationwide nested case-control study.
2011;106:319-328 [PMID:21045815 DOI:10.1038/ajg.2010.428]
42 Stang A.Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses.
2010;25:603-605 [PMID:20652370 DOI:10.1007/s10654-010-9491-z]
43 Okugawa Y,Toiyama Y,Kusunoki M,Goel A.Re:Cumulative burden of inflammation predicts colorectal neoplasia risk in ulcerative colitis:a large single-centre study.
2019;68:575 [PMID:29535153 DOI:10.1136/gutjnl-2018-316205]
44 Lakatos L,Mester G,Erdelyi Z,David G,Pandur T,Balogh M,Fischer S,Vargha P,Lakatos PL.Risk factors for ulcerative colitis-associated colorectal cancer in a Hungarian cohort of patients with ulcerative colitis:results of a population-based study.
2006;12:205-211 [PMID:16534422 DOI:10.1097/01.MIB.0000217770.21261.ce]
45 Xu W,Ding W,Gu Y,Cui L,Zhong J,Du P.Risk Factors of Colorectal Stricture Associated with Developing High-Grade Dysplasia or Cancer in Ulcerative Colitis:A Multicenter Long-term Followup Study.
2020;14:601-610 [PMID:31816674 DOI:10.5009/gnl19229]
46 Ando T,Ishiguro K,Maeda O,Watanabe O,Miyake N,Nakamura M,Miyahara R,Ohmiya N,Goto H.Clinicopathological characteristics of colorectal cancer in patients with ulcerative colitis.
2010;71:AB345-AB346 [DOI:10.1016/j.gie.2010.03.919]
47 Lutgens M,Siersema PD,Vleggaar F,Broekman M,Van Bodegraven AA,Dijkstra G,Hommes DW,De Jong D,Stokkers PCF,Van Der Woude CJ,Oldenburg B.Risk factors for inflammatory bowel disease associated colorectal carcinoma.
2011;5:S12
48 Lutgens MW,Siersema PD,Vleggaar FP,Broekman M,Van Oijen MG,Van Bodegraven AA,Dijkstra G,Hommes DW,De Jong DJ,Ponsioen C,Van Der Woude CJ,Oldenburg B.Risk factors for advanced neoplasia of the rectal stump in IBD patients.
2011;140:S351-S352[DOI:10.1016/S0016-5085(11)61433-9]
49 Mahmoud R,Shah S,Ten Hove J,Torres J,Mooiweer E,Castaneda D,Glass J,Elman J,Kumar A,Axelrad J,Ullman T,Colombel JF,Oldenburg B,Itzkowitz S.Post-inflammatory polyps do not predict colorectal neoplasia in patients with inflammatory bowel disease:A multinational retrospective cohort study.
2018;12:S156-S157
50 Lewis AE,Kirchgesner J,Dray X,Svrcek M,Beaugerie L.Clinical Significance of Pseudopolyps for Patients With Inflammatory Bowel Disease.
2019;114:S179-S180 [DOI:10.14309/01.ajg.0000590752.06064.e8]
51 Abou Rached A,Saniour J,Shehab R,Abou Fadel C,Yaghi C,Khairallah S.The association between the severity of histological lesions with the disease location and presence of colonic lesions in patients with ulcerative colitis.
2019;13:S235-S236 [DOI:10.1093/ecco-jcc/jjy222.398]
52 Flores BM,O'Connor A,Moss AC.Impact of mucosal inflammation on risk of colorectal neoplasia in patients with ulcerative colitis:a systematic review and meta-analysis.
2017;86:1006-1011.e8 [PMID:28750838 DOI:10.1016/j.gie.2017.07.028]
53 Dukes CE.The surgical pathology of ulcerative colitis.
1954;14:389-400[PMID:13159102]
54 Kusunoki M,Nishigami T,Yanagi H,Okamoto T,Shoji Y,Sakanoue Y,Yamamura T,Utsunomiya J.Occult cancer in localized giant pseudopolyposis.
1992;87:379-381 [PMID:1539578]
55 Jawad N,Graham T,Novelli M,Rodriguez-Justo M,Feakins R,Silver A,Wright N,McDonald S.PTU-124 Are pseudopolyps the source of tumorigenic mutations in ulcerative colitis?
2012;61:A236 [DOI:10.1136/gutjnl-2012-302514c.124]
56 Lozyns'ka MR.[The spectrum of cytogenetic chages in polyps of the large intestine with different histologic structure].
2008;42:43-49 [PMID:19253754]
57 Liatsos C,Kyriakos N,Panagou E,Karagiannis S,Salemis N,Mavrogiannis C.Inflammatory polypoid mass treated with Infliximab in a Crohn's disease patient.
2010;4:707-708[PMID:21122587 DOI:10.1016/j.crohns.2010.09.006]
58 Cohen-Mekelburg S,Schneider Y,Gold S,Scherl E,Steinlauf A.Advances in the Diagnosis and Management of Colonic Dysplasia in Patients With Inflammatory Bowel Disease.
2017;13:357-362 [PMID:28690452]
59 Shah SC,Itzkowitz SH.Management of Inflammatory Bowel Disease-Associated Dysplasia in the Modern Era.
2019;29:531-548 [PMID:31078251 DOI:10.1016/j.giec.2019.02.008]
60 Choi YS,Suh JP,Lee IT,Kim JK,Lee SH,Cho KR,Park HJ,Kim DS,Lee DH.Regression of giant pseudopolyps in inflammatory bowel disease.
2012;6:240-243 [PMID:22325179 DOI:10.1016/j.crohns.2011.08.007]
 World Journal of Gastrointestinal Oncology2022年1期
World Journal of Gastrointestinal Oncology2022年1期
- World Journal of Gastrointestinal Oncology的其它文章
- Comment on “Outcomes of curative liver resection for hepatocellular carcinoma in patients with cirrhosis”
- Liquid biopsy:Precise diagnosis and therapy for cholangiocarcinoma
- Exosomes as potential diagnosis and treatment for liver cancer
- Effects of cognitive behavior therapy combined with Baduanjin in patients with colorectal cancer
- Intertwined leukocyte balances in tumours and peripheral blood as robust predictors of right and left colorectal cancer survival
- Digestive cancer incidence and mortality among young adults worldwide in 2020:A population-based study
