Caseous calcification of mitral annulus in the setting of multivessel disease
Swetha R Nuthulaganti?, Bijal R Patel, Carly A Rabinowitz, Maria Gutierrez, Khadeeja Esmail,Reeba Omman
Department of Medicine, Division of Cardiology, UF Health Jacksonvile, Jacksonville Fl, United States
Caseous calcification of the mitral annulus(CCMA) is a chronic degenerative process affecting the mitral valve fibrous ring. It is a rare variant of mitral annular calcification(MAC) that is frequently misdiagnosed as endocarditis, cardiac tumor, or abscess. Patients can present with palpitations and dyspnea; however, CCMA does not have a specific clinical presentation and diagnosis is typically made incidentally by presence of an intracardiac mass on cardiac imaging.Transthoracic echocardiography (TTE) remains the preferred imaging modality for diagnosis of CCMA;however, multimodality imaging with transesophageal echocardiography (TEE), cardiac computed tomography (CT), or cardiac MRI (CMRI) may be necessary when the diagnosis remains unclear. Although CCMA is frequently benign, it has been associated with cerebral embolization and valvular dysfunction. Multimodality imaging can clearly differentiate CCMA from other lesions and should be employed when diagnosis remains unclear. Uncomplicated CCMA can be managed conservatively and surgical intervention with mitral valve replacement is reserved for complicated cases. Calcifications of the mitral valve annulus have a higher prevalence in patients with multiple cardiovascular risk factors,as was seen in our patient. While her symptoms of chronic angina, dizziness, dyspnea, and palpitations were likely due to multivessel coronary artery disease (CAD), evaluation of her symptoms led to incidental discovery of a large mobile cardiac mass with high risk for embolization. This case demonstrates the importance of employing multimodality imaging to accurately diagnose CCMA in a highrisk patient (elderly, female, and multiple CAD risk factors).
We present the case of a 68 years old Hispanic female with past medical history hypertension, hyperlipidemia, heart failure with preserved ejection fraction, and diabetes mellitus (DM) who presented to the emergency department with one year history of typical anginal chest pain with radiation to the back, dyspnea on exertion, and occasional nighttime dizziness and palpitations. She had an outpatient stress TTE to evaluate chronic angina which revealed a mobile echoic mass on the posterior mitral valve leaflet concerning for tumor, thrombus, or vegetation. Stress echo was prematurely terminated upon detection of the mass and the patient was instructed to start Coumadin and seek further evaluation in the emergency department.
Upon admission, patient’s vital signs were within normal limits; basic labs and cultures obtained to rule out concerns for an infectious process were negative for acute infection. CT chest, however, demonstrated extensive calcification in the area of the mitral of the mitral valve annulus. Cardiology was consulted for a transesophageal echocardiogram to further characterize the mass. TEE revealed a hypermobile 0.7 × 1.0 cm pseudo-pedunculated hyperechogenic structure with areas of central lucency extending from the posterior mitral valve annulus. There was trace mitral regurgitation however no evidence of mitral stenosis or outflow tract obstruction.Surgical removal of the mass was pursued as its large size and degree of mobility conferred a high risk of embolization.
Pre-operative left heart catheterization was performed for evaluation of chronic angina which was remarkable for two-vessel obstructive CAD. Given her history of DM, patient had concomitant CABG at time of mitral valve mass removal. Surgical pathology resulted with diffuse granular calcifications,focal giant cell reaction, and endocardial cell proliferation. Gram stain was unremarkable for fungal or bacterial pathogens. Her postoperative course was notable for bilateral pleural effusions and hypervolemia which improved with diuresis and thoracentesis. She was weaned off supplemental oxygen and had appropriate wound healing at three months follow up with cardiothoracic surgery (Figures 1?4).
Mitral annular calcification (MAC) is a chronic degeneration of the mitral valve fibrous ring involving mainly the posterior annulus.[8]Caseous calcification of the mitral valve annulus (CCMA) is a rare variant of MAC that typically affects the posterior mitral annulus as opposed to the mid-base of the posterior leaflet. It accounts for 0.63% of all cases of MAC and affects 0.06-0.07% of the total population.[1]CCMA is more commonly observed in the elderly population with a predilection for females.
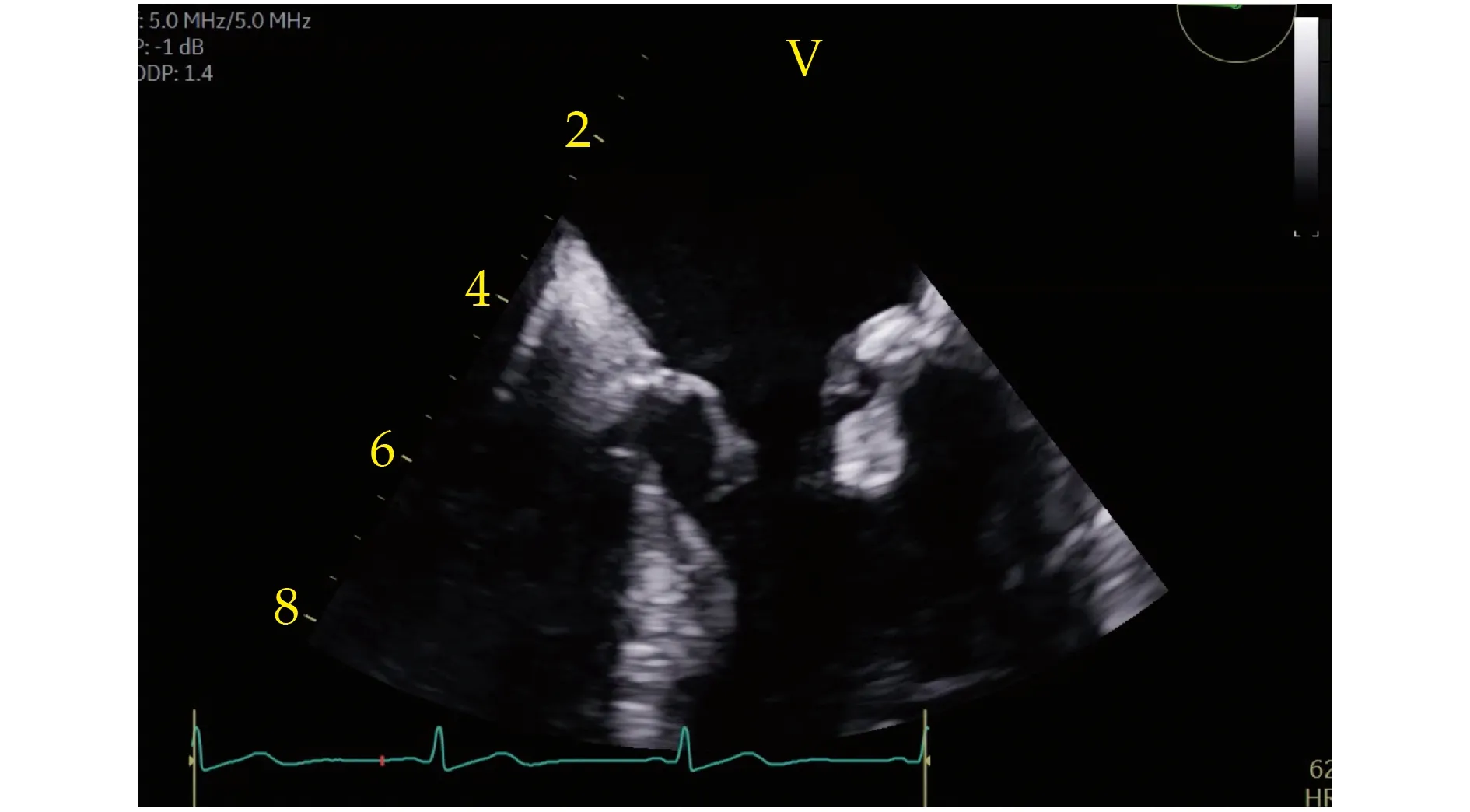
Figure 1 Hyper echogenic 0.7 × 1 cm mobile mass with central lucency extending from the posterior annulus (2D echo image, 4 chamber view).
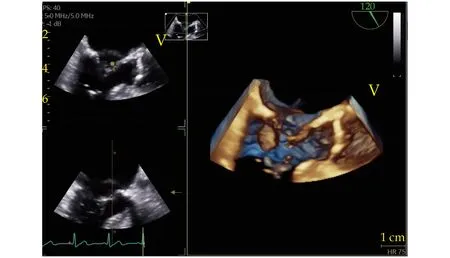
Figure 2 Mitral valve from ventricular side of valve (3D image).
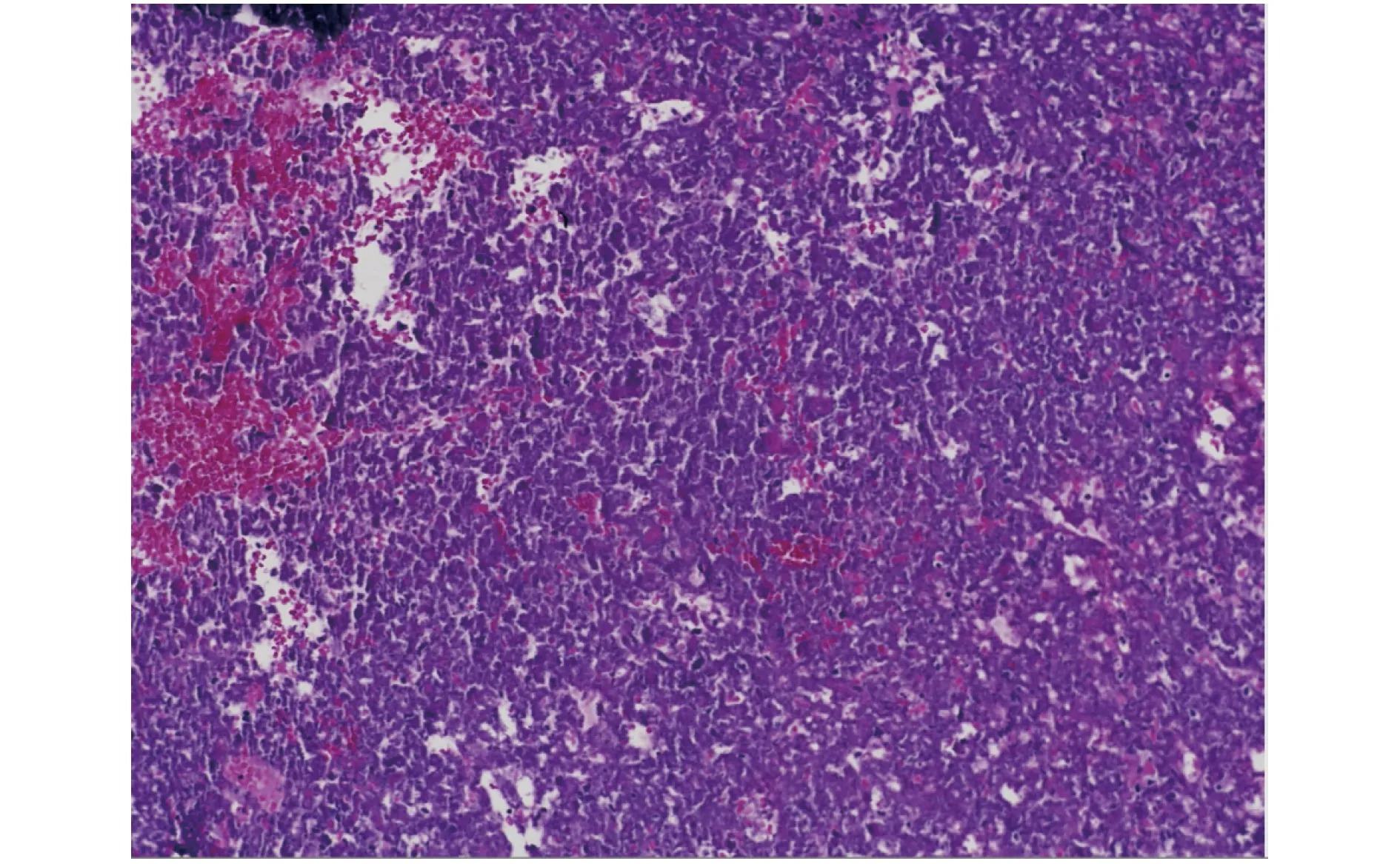
Figure 3 Pathology: higher power image shows purple granular deposits consistent with calcifications.

Figure 4 Arrows pointing towards granular deposits of calcification.
This condition typically runs a benign course, although associated cerebral embolization and valvular dysfunction have been reported.[8,3]CCMA can also result in turbulent flow across the mitral valve causing chronic mitral regurgitation, and less likely mitral stenosis. Given the proximity of the mitral annulus to the atrioventricular node and conduction system, CCMA may also result in bradyarrhythmias and atrioventricular blocks.[7]
The mechanism underlying liquefaction and caseation in CCMA is not well understood, however is thought to involve lipid-laden macrophages. Abnormal calcium phosphate metabolism has also been implicated in its pathogenesis as CCMA as there is a strong association between CCMA and end-stage renal disease and hypertension.[5]Histopathology may show a central region of amorphous eosinophilic acellular material surrounded by macrophages and lymphocytes and peripheral calcifications and zones of necrosis.[7]
CCMA is frequently discovered incidentally as an intracardiac mass on imaging.[7]Some patients develop dyspnea, palpitations, or syncope secondary to atrioventricular blocks, systemic embolization, or transient left ventricular outflow tract obstruction.[4]Given the rarity of this condition, it is frequently misdiagnosed as a myocardial abscess, cardiac tumor, vegetation, or calcified thrombi.[2]
TTE remains the preferred imaging modality for diagnosis of CCMA which appears as a large, echodense, soft mass with central echolucency without acoustic shadowing. When the diagnosis remains unclear, multimodality imaging including TEE, cardiac CT, and CMRI can be employed to further support the diagnosis and avoid unnecessary surgery.[6]
CCMA typically resolves spontaneously; however,it can transform back to MAC or recur even after surgical excision. There is no consensus on management of CCMA, however conservative medical management is preferred. Surgical intervention is indicated in the presence of mitral valvular dysfunction (stenosis or regurgitation), embolic manifestations, or when malignancy cannot be ruled out.In these patients, mitral valve replacement is preferred over repair.[7]
 Journal of Geriatric Cardiology2022年3期
Journal of Geriatric Cardiology2022年3期
- Journal of Geriatric Cardiology的其它文章
- COVID-19: cardiovascular manifestations—a review of the cardiac effects
- Associations of body mass index and hospital-acquired disability with post-discharge mortality in older patients with acute heart failure
- Mortality in patients with heart failure and suicidal ideation discharged to skilled nursing facilities
- Association of time-varying changes in physical activity with cardiac death and all-cause mortality after ICD or CRT-D implantation
- Severe aortic stenosis and acute coronary syndrome in an elderly patient with idiopathic thrombocytopenic purpura:a therapeutic challenge
- Relationship of body fat and left ventricular hypertrophy with the risk of all-cause death in patients with coronary artery disease
